The annual number of infectious syphilis notifications in Australia increased four‐fold during 2011–2019, from 1332 to 5912,1 and similar rises for tertiary syphilis, including neurosyphilis, are anticipated. In Australia, information about neurosyphilis epidemiology is limited because national surveillance reports do not usually stratify data by syphilis stage.1 However, neurosyphilis‐related hospital admission rates can serve as proxy measures of its prevalence. We therefore investigated neurosyphilis admissions in Australia, including the duration of hospital admissions and associated costs.
We analysed publicly available admissions data (Australian Institute of Health and Welfare National Hospital Morbidity database2) for people aged 15 years or more admitted to public and private Australian hospitals during 1 July 2007 – 30 June 2020 with neurosyphilis as the principal diagnosis (International Classification of Diseases, tenth revision, Australian modification codes A52.1 or A52.3). We calculated the annual admission rate by financial year and sex (based on Australian Bureau of Statistics population data3), and estimated the incident rate ratio (IRR) with 95% confidence interval (CI) for the study period. In subgroup analyses, we estimated admission rates for people of reproductive age (15–50 years) by sex, and separately assessed more recent changes in admission rates (2014–20). We used Independent Hospital Pricing Authority (IHPC) data on acute hospital care4 to estimate costs (mean cost per admission day, $1271 to $2223; further details: Supporting Information). The Alfred Hospital Ethics Committee approved the study (project 97/22).
During 2007–20, 1063 men and 312 women were admitted to Australian hospitals with neurosyphilis. The mean duration of hospital admission was 11.3 days (standard deviation [SD], 3.4 days) for men and 10.1 days (SD, 3.2 days) for women (Supporting Information, table 1). Based on IHPC data, the admission cost was $13 981 to $24 453 per person per episode (for mean length of stay of 11 days).
The annual admission rate increased across 2007–20 for men (IRR, 1.04; 95% CI, 1.03–1.06) but not for women (IRR, 1.00; 95% CI, 0.97–1.03). During 2014–20, the annual hospital admission rate increased for both men (IRR, 1.16; 95% CI, 1.10–1.22) and women (IRR, 1.16; 95% CI, 1.05–1.28) (Box; Supporting Information, figure 1). A total of 458 men and 62 women of reproductive age (15–50 years) were admitted to hospital with neurosyphilis; the annual admission rate for this age group increased for both men (IRR, 1.08; 95% CI, 1.05–1.10) and women (IRR, 1.10; 95% CI, 1.02–1.18) (Supporting Information, figure 2).
We found that the population rate of men admitted to hospital with neurosyphilis increased during 2007–20, paralleling reported increases in syphilis notifications. The rate for women has increased since 2014–15, also reflecting increased syphilis notification numbers.1 Our findings indicate that the increase in the number of neurosyphilis admissions is probably a consequence of the recent rise in the incidence of syphilis in Australia.
If the number of syphilis infections continues to increase, neurosyphilis‐related admissions and their hospital costs will also rise. More effective syphilis control is needed, including better access to sexually transmitted infections services for people with symptoms and increased testing for and treatment of syphilis. Raising awareness of neurosyphilis in primary care is important for timely diagnosis and referral. Improving the collection of neurosyphilis surveillance data and integrating neurosyphilis incidence data into syphilis reports may enhance our understanding of the epidemiology of neurosyphilis.
Box – Neurosyphilis‐related public and private Australian hospital admissions of people aged 15 years or more, 2007–20, by year and sex*
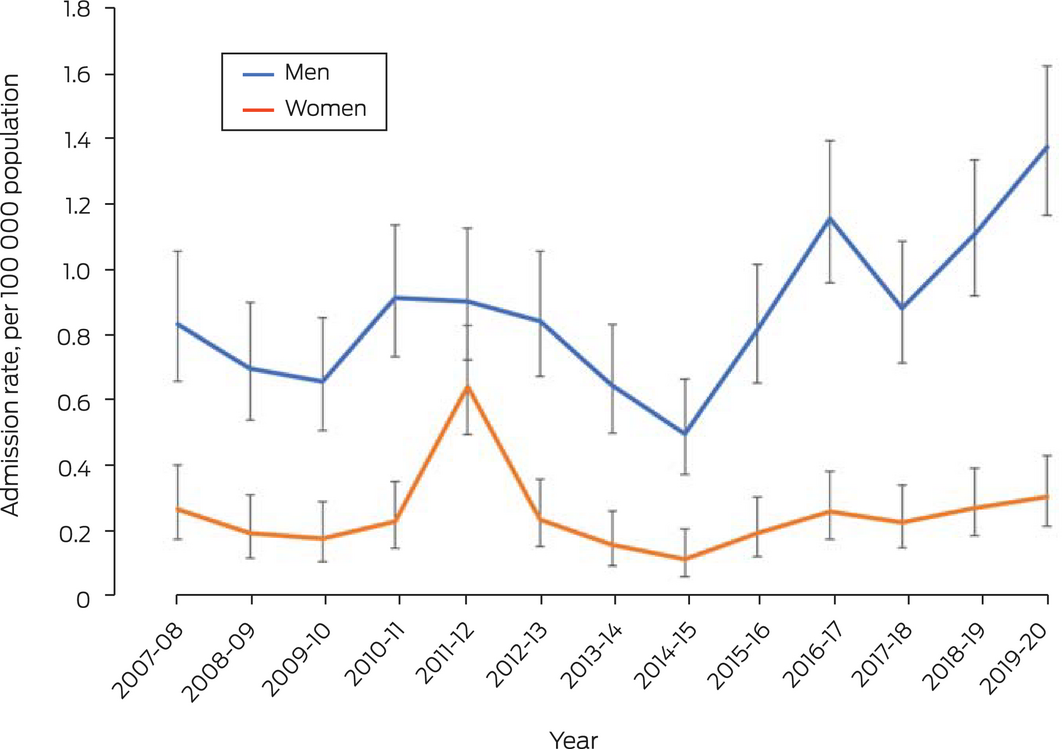
* Admission rates with 95% confidence intervals estimated using Poisson regression. The data for this graph are included in the Supporting Information, table 2.
Received 24 May 2022, accepted 1 December 2022
- 1. Kirby Institute. HIV, viral hepatitis and sexually transmitted infections in Australia: annual surveillance report 2021. Sydney: Kirby Institute, UNSW Sydney, 2021. https://kirby.unsw.edu.au/sites/default/files/kirby/report/Annual‐Surveillance‐Report‐2021_STI‐221107.pdf (viewed Aug 2022).
- 2. Australian Institute of Health and Welfare. Separation statistics by principal diagnosis (ICD‐10 11th edition), Australia, 2019–20 (Cat. no. WEB 216). Updated 8 July 2022. https://www.aihw.gov.au/reports/hospitals/principal‐diagnosis‐data‐cubes/contents/data‐cubes (viewed Aug 2022).
- 3. Australian Bureau of Statistics. Population by age and sex: national. 16 Dec 2021. https://www.abs.gov.au/statistics/people/population/national‐state‐and‐territory‐population/jun‐2021#data‐downloads‐data‐cubes (viewed Aug 2022).
- 4. Independent Hospital Pricing Authority. National hospital cost data collection report, public sector, round 24 (financial year 2019–20). Oct 2021. https://www.ihacpa.gov.au/sites/default/files/2022‐08/NHCDC%20Round%2024%20Report_0_0.pdf (viewed Aug 2022).






Open access
Open access publishing facilitated by Monash University, as part of the Wiley – Monash University agreement via the Council of Australian University Librarians.
Ei T Aung is supported by an Australian Government Research Training Program scholarship administered by Monash University and a Research Entry Scholarship from the Chapter of Sexual Health Medicine of the Royal Australasian College of Physicians. Christopher K Fairley (GNT1172900) and Eric PF Chow (GNT1172873) are supported by National Health and Medical Research Council (NHMRC) Emerging Leadership Investigator Grants. Jason J Ong is supported by an NHMRC Emerging Leadership Investigator Grant (GNT1193955).
No relevant disclosures.