The known: Outcomes for older people with COVID‐19 since the emergence of the Omicron virus variant have been less extensively reported than for the Delta variant.
The new: In residential aged care residents with COVID‐19, hospitalisation was more likely for people with dementia, heart failure, chronic kidney disease, or asthma, and death for people with dementia, diabetes, heart failure, or chronic lung disease; the likelihood of each was greater for men and for residents who had not received three vaccine doses.
The implications: Vaccination is a modifiable risk factor that may reduce the likelihood of hospitalisation and death for aged care residents with COVID‐19. Factors related to general health and frailty identify older people at greater risk of severe COVID‐19.
The first case of coronavirus disease 2019 (COVID‐19) in Australia was detected in January 2020.1 The subsequent distribution of cases across Australia to December 2021 was heterogeneous; clusters of infections linked by community transmission were reported in Queensland, but the overall incidence remained low,2 predominantly because of public health suppression measures, including border restrictions.3 Queensland COVID‐19 case numbers grew exponentially following the easing of border restrictions on 13 December 2021. The 7‐day mean case detection rate increased from fewer than five per day prior to 13 December 2021 to 15 000 per day on 24 January 2022.2 However, the incidence was probably underestimated because testing centres were overwhelmed and rapid antigen test (RAT) results were not centrally reported.4
The impact of COVID‐19 was particularly marked in residential aged care facilities (RACFs). More advanced age was the strongest predictor of adverse outcomes, and RACFs are often conducive to viral transmission.5,6,7,8 A meta‐analysis of 49 studies of outbreaks in 8502 RACFs in North America, Europe, China, South Korea, and Australia estimated that the overall case fatality rate for RACF residents was 23% (95% confidence interval [CI], 18–28%).7 In Australia, prior to widespread vaccination against COVID‐19, RACF outbreak case fatality rates reached 46%,6 and 74% of COVID‐19‐related deaths were of RACF residents.9
In our study, we assessed the COVID‐19 burden in RACFs in the Metro South Hospital and Health Service area of southeast Queensland during the first six weeks of easing interstate border restrictions (December 2021 – January 2022). At this time, the dominant circulating severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) strain was the Omicron variant (lineage BA.1).10 We determined the characteristics associated with the likelihood of hospitalisation and death of people with COVID‐19 living in RACFs who had not previously contracted COVID‐19.
Methods
In our retrospective cohort study, we collated data for all confirmed (polymerase chain reaction testing) or probable SARS‐CoV‐2 infections (rapid antigen tests) among residents of RACFs in the Metro South Hospital and Health Service area during 13 December 2021 – 24 January 2022. In 2019, the Metro South Hospital and Health Service area included 1 184 764 people (13% aged 65 years or more), or 23.3% of the Queensland population.11
Cases were primarily ascertained in reports to the Metro South Public Health Unit by pathology service providers, surveillance and contact tracing activities, and hospitals. Clinical data, including cardiopulmonary resuscitation status (record of whether a resident wanted to be resuscitated in the event of cardiac arrest), were obtained from chart review of Queensland Health electronic medical records or RACF reports for all residents with SARS‐CoV‐2 infections. Vaccination status was determined in the Australian Immunisation Register, medical records, and the Queensland Notifiable Conditions Register.
Outcomes
The primary outcomes were hospitalisation within 14 days and death within 28 days of COVID‐19 diagnosis. Hospitalisations were reported by RACFs. We reviewed the clinical records of all residents with recorded SARS‐CoV‐2 infections to determine whether they had presented to a Queensland Health facility. Deaths were reported by RACFs (active surveillance), clinicians caring for residents in the community (including general practitioners; reporting to the Public Health Unit), the Metro South Hospital and Health Service (reporting to the Public Health Unit), or Queensland Health data compilation processes (data from the Registry of Births, Deaths and Marriages; possible COVID‐19‐related deaths reported to the Public Health Unit). We reviewed the clinical records of all residents with SARS‐CoV‐2 infections to ensure that no inpatient deaths were missed (Supporting Information, supplementary methods).
Statistical analysis
We separately assessed associations between COVID‐19‐related hospitalisations and deaths and age, sex, cognitive status, number of COVID‐19 vaccine doses received, selected comorbid conditions, and body mass index in univariable and multivariable logistic regression models adjusted for confounders identified in directed acyclic graphs; we report unadjusted and adjusted odds ratios (aORs) with 95% CIs. The primary analyses excluded cases with missing data for any evaluated comorbid condition; sensitivity analyses assumed missing data indicated the absence or presence of the condition (univariable models only). All analyses were undertaken in Stata 14.2.
Ethics approval
The Metro South Hospital and Health Service Human Research Ethics Committee exempted our study from formal human research ethics approval (EX/2022/QMS/83664).
Results
Eighty‐six federal government‐supported RACF sites in the Metro South Hospital and Health Service area were home to about 10 500 permanent staff and 8700 residents during the study period (as reported by RACFs). All RACFs reported COVID‐19 infections during this period (only among staff for 15 RACFs): 1425 infections in staff members (about 14%) and 1080 in residents (about 12%). As identifying information was inadequate for nine residents, 1071 RACF residents with COVID‐19 were included in our analysis (Box 1).
At least 90% of residents had received at least two vaccine doses in 51 RACFs (59%), 80–89% of residents in 25 (29%), and fewer than 80% in eight (9%); two facilities did not provide cumulative vaccination data. Of the 1071 residents with COVID‐19, 151 were hospitalised within 14 days (14%) and 126 died within 28 days of diagnosis (12%); 64 people who died had been hospitalised with COVID‐19.
The proportions of residents diagnosed with COVID‐19, admitted to hospital, or who died were similar for for‐profit and not‐for‐profit RACFs, and did not differ by the proportion of RACF staff with COVID‐19; each proportion was slightly larger for RACFs in socio‐economically disadvantaged areas than for those in areas of middle or low disadvantage (Supporting Information, table 1).
Likelihood of hospitalisation and death
The likelihood of death increased with age (per five years: aOR, 1.38; 95% CI, 1.21–1.57), but not that of hospitalisation (aOR, 1.06; 95% CI, 0.96–1.17). The likelihood of hospitalisation (aOR, 1.7; 95% CI, 1.2–2.4) and death (aOR, 2.5; 95% CI, 1.7–3.6) were each higher for men than women. Diagnosed dementia was associated with greater likelihood of hospitalisation (aOR, 1.9; 95% CI, 1.2–3.0) and death (aOR, 2.2; 95% CI, 1.3–3.7). The likelihood of hospitalisation and death were each higher for residents who had received no, one, or two doses of any COVID‐19 vaccine than for those who had received three doses (Box 2, Box 3).
The likelihood of hospitalisation was greater for those with heart failure (aOR, 1.7; 95% CI, 1.1–2.7), chronic kidney disease (aOR, 1.7; 95% CI, 1.1–2.5), or asthma (aOR, 2.2; 95% CI, 1.2–3.8). The likelihood of death was greater for residents with diabetes mellitus (aOR, 1.9; 95% CI, 1.3–3.0), heart failure (aOR, 2.0; 95% CI, 1.1–3.3), or chronic lung disease (aOR, 1.7; 95% CI, 1.1–2.7) (Box 2, Box 3).
Sensitivity analyses
The outcomes of univariable analyses that assumed that missing comorbid condition information indicated that a resident did not have the condition (the most plausible scenario, based on potential referral bias) were similar to those of the main analysis. In the converse analysis, which assumed that the condition was present if data were missing, diabetes and obesity were associated with lower likelihood of hospitalisation, asthma and obesity with lower likelihood of death, and diagnosed dementia with greater of death (Supporting Information, table 4).
Discussion
Our study focused on identifying characteristics associated with the hospitalisation or death of RACF residents with first time COVID‐19 during a period when the predominant circulating SARS‐CoV‐2 strain was the Omicron BA.1 variant.10 During the 6‐week study period, about 12% of RACF residents in the Metro South Hospital and Health Service area were diagnosed with COVID‐19, and 12% of residents with COVID‐19 died. This case fatality rate was much lower than reported for RACFs earlier in the COVID‐19 pandemic, but higher than the case fatality rate for Australia during the study period for people aged 80 years or more (4.7%).10 High vaccination rates, more and better treatment options, and possibly the low virulence of the Omicron BA.1 strain compared with earlier variants, might explain the lower case fatality rate.12,13 Case fatality rates for influenza outbreaks in Australian RACFs range between 4.0% and 4.5%.14,15
The hospitalisation rate in our study (14%) was lower than found by a systematic review of COVID‐19 outbreaks in RACFs on four continents during 2020 (37%; 95% CI, 35–39%).7 Outreach services provided by specialist emergency physicians and geriatricians probably minimised unnecessary hospital presentations.16 The proportions of RACF residents who contracted COVID‐19, were hospitalised, or died were larger in socio‐economically disadvantaged areas. In 2020, the age‐standardised COVID‐19 mortality rate was higher in socio‐economically disadvantaged areas of Australia (females, 2.7 per 100 000; males, 4.3 per 100 000 population) as in areas of greatest advantage (females, 1.3 per 100 000; males, 1.6 per 100 000 population).6 Higher SARS‐CoV‐2 infection incidence has also been related to socio‐economic disadvantage, financial stress, and lower baseline health status and health literacy.17
The likelihood of death was lower for residents who had received three vaccine doses than for those who had received fewer, but we could not determine whether the number of doses or the recent administration of the third dose was more important for this effect. A United Kingdom study found that 168 of 199 healthy staff volunteers (83%) had developed neutralising antibodies against the Omicron variant two to six weeks after their second Pfizer–BioNTech BNT162b2 dose (but with lower titres than for the Delta variant), and 82 of 85 (96%) two to six weeks after their third dose.18 Similarly, in an observational study in Singapore (703 209 people), the incidence of severe COVID‐19 (Delta variant) was much lower among people who had received three rather than two vaccine doses (incidence rate ratio, 0.05; 95% CI, 0.03–0.08).19 However, the proportion of people in our study who had recorded wishes to not be resuscitated was larger among those who were unvaccinated (49%) than among residents who had received three doses (35%), which may have affected our finding. In a representative sample prior to the COVID‐19 pandemic, 160 of 198 people (83%) with advanced care plans in the Metro South Hospital and Health Service had opted to not receive cardiopulmonary resuscitation if required.20
Characteristics linked with frailty were associated with greater likelihood of death, particularly advanced age (80 years or older). A 2020 population‐based NSW study (4054 people with COVID‐19) found that the risk of severe illness or death was significantly higher for people aged 70 years or more, and rose with each decade of age.5 We found that dementia was associated with both hospitalisation and death, consistent with other reports.21,22 In 2019, dementia contributed to 9.5% of deaths in Australia.23 It is also possible that the resuscitation wishes of residents with dementia were more clearly defined; 50% of those with dementia (and 42% of residents without cognitive impairment) had documented wishes to not receive cardiopulmonary resuscitation. Social interaction is important for people with dementia,24 and the isolation of lockdowns may have adversely affected their health.
Hospitalisation and death were both more likely for men, as previously reported in a NSW population study (severe disease: adjusted hazard ratio, 1.4; 95% CI, 1.0–1.9)3 and in a Spanish study of 345 RACF residents with COVID‐19 (death: aOR, 3.4; 95% CI, 2.4–4.7).21 However, a systematic review of five Italian studies (3327 RACF residents) found no sex difference (relative risk of death, 0.98; 95% CI, 0.7–1.4).25 Differences in innate and adaptive immunity have been proposed as reasons for sex‐related differences;26 sex differences in frailty in older people may also contribute.27
The likelihood of death was higher for those with chronic lung disease and heart failure, consistent with an earlier report on RACF residents with COVID‐19.25 As the interaction of age, chronic illness, and frailty is complex, some of these associations may indicate poor general health status rather than the condition directly influencing the outcome of COVID‐19.
Diabetes mellitus was associated with greater likelihood of death but not of hospitalisation, consistent with previous reports.25,28 Possible reasons for the lack of influence on hospitalisation include neuropathy; early warning signs of severe lower respiratory tract infections, such as pleuritic chest pain or myocardial ischaemia related to hypercoagulability, may be missed because the associated pain is not experienced. Acute COVID‐19 exacerbates diabetic neuropathy.29 Alternatively, people with diabetes may be preferentially managed in the RACF.
Asthma was associated with greater likelihood of hospitalisation, but not of death. A meta‐analysis of four studies of people with COVID‐19 (744 with asthma, 8151 without asthma) did not find an association with death (OR, 0.96; 95% CI, 0.70–1.30).30 However, a recent Scottish study found that the risks of COVID‐19‐related hospitalisation and death were higher for adults with asthma, particularly those with poorly controlled asthma.31 We do not know how many residents in our study regularly used inhaled corticosteroids, which may reduce the risk of death from COVID‐19.32 Because they are predisposed to bronchial hyperresponsiveness, people with asthma may develop respiratory symptoms early in COVID‐19, which may in turn lead to earlier hospital admission and access to disease‐modifying treatment. Asthma is frequently missed in older people,31 increasing the risk of misclassification of whether residents had this condition.
Limitations
Our ascertainment of hospitalisations and deaths was probably close to complete, but admissions of residents to private hospitals not reported by their RACFs would not be included. However, private hospitals did not admit people with COVID‐19 during the study period. That oral antiviral agents were not available during the study period should be considered when interpreting our findings.
One major limiting factor was that COVID‐19 case ascertainment may have been incomplete, which would affect our case fatality rates. Case ascertainment was limited by resource constraints during the Queensland‐wide pandemic and our reliance on RACFs reporting cases. Residents with COVID‐19 may have been missed because they were not tested (including those with asymptomatic infections) or not reported. Early in the Omicron variant wave (at the beginning of our study period), case numbers could be checked against the reported results of pathology testing; all residents in an RACF with one infected resident or staff member were tested. However, because of the increase in demand for PCR testing later in the wave, only people with symptomatic infections and their close contacts were tested, or they were tested on an ad hoc basis guided by individual facility risk assessments. Testing capacity was improved by the introduction of RATs, but supply problems limited early access.2 No clinical or system factors are known that would influence the likelihood of choosing PCR or RAT testing of residents.
A second major limitation was incomplete information about comorbid conditions for about 15% of residents with COVID‐19, because we gathered this information by reviewing Queensland Health medical records. This information was not available for residents who had not previously presented to public hospitals, introducing referral bias: people with mild COVID‐19 were less likely to be admitted to hospital, while people with only a few (or no) comorbid conditions may have been less likely to require hospitalisation. Integrated electronic records linking private and public hospital data with general practice data are not available in Queensland.
Conclusion
We identified characteristics associated with the likelihood of hospitalisation or death of RACF residents with COVID‐19 in Queensland during late December 2021 – early January 2022 (during the Omicron wave). Most of these characteristics were non‐modifiable factors linked with frailty and general health status, but having received three doses of a COVID‐19 vaccine was associated with lower likelihood of hospitalisation or death. While the case fatality rate during the study period was lower than at the start of the pandemic, it was higher than that for influenza in RACFs and the overall Australian case fatality rate among older people with COVID‐19.
Box 1 – Characteristics of 1071 residential aged care facility residents in the Metro South Hospital and Health Service area of southeast Queensland diagnosed with COVID‐19, 13 December 2021 – 24 January 2022*
|
|
Admitted to hospital |
Died |
|||||||||||||
|
Characteristic |
No |
Yes |
No |
Yes |
|||||||||||
|
|
|||||||||||||||
|
Number of people |
920 |
151 |
945 |
126 |
|||||||||||
|
Age (years) |
|
|
|
|
|||||||||||
|
Median (IQR) |
84 (78–90) |
84 (78–89) |
83 (77–89) |
87 (82–91) |
|||||||||||
|
Under 70 |
73 (8%) |
11 (7%) |
79 (8%) |
5 (4%) |
|||||||||||
|
70–79 |
219 (24%) |
31 (21%) |
233 (25%) |
17 (13%) |
|||||||||||
|
80–89 |
390 (42%) |
74 (49%) |
400 (42%) |
64 (51%) |
|||||||||||
|
90 or more |
238 (26%) |
35 (23%) |
235 (25%) |
40 (32%) |
|||||||||||
|
Sex |
|
|
|
|
|||||||||||
|
Women |
528 (57%) |
69 (46%) |
546 (58%) |
51 (40%) |
|||||||||||
|
Men |
392 (43%) |
82 (54%) |
399 (42%) |
75 (60%) |
|||||||||||
|
Cognitive status |
|
|
|
|
|||||||||||
|
No impairment |
225 (24%) |
32 (21%) |
234 (25%) |
23 (18%) |
|||||||||||
|
Mild impairment |
219 (24%) |
33 (22%) |
231 (24%) |
21 (17%) |
|||||||||||
|
Diagnosed dementia |
336 (37%) |
84 (56%) |
345 (37%) |
75 (60%) |
|||||||||||
|
Missing data |
140 (15%) |
2 (1%) |
135 (14%) |
7 (6%) |
|||||||||||
|
Vaccine doses |
|
|
|
|
|||||||||||
|
None |
100 (11%) |
30 (20%) |
95 (10%) |
35 (28%) |
|||||||||||
|
One |
46 (5%) |
11 (7%) |
50 (5%) |
7 (6%) |
|||||||||||
|
Two |
421 (46%) |
88 (58%) |
436 (46%) |
73 (58%) |
|||||||||||
|
Three or more |
332 (36%) |
22 (15%) |
343 (36%) |
11 (9%) |
|||||||||||
|
Missing data |
21 (2%) |
0 |
21 (2%) |
0 |
|||||||||||
|
Diabetes mellitus |
|
|
|
|
|||||||||||
|
No |
554 (60%) |
105 (70%) |
586 (65%) |
73 (58%) |
|||||||||||
|
Yes |
212 (23%) |
44 (29%) |
211 (22%) |
45 (36%) |
|||||||||||
|
Missing data |
154 (17%) |
2 (1%) |
147 (16%) |
8 (6%) |
|||||||||||
|
Ischaemic heart disease |
|
|
|
||||||||||||
|
No |
564 (61%) |
99 (66%) |
581 (61%) |
82 (65%) |
|||||||||||
|
Yes |
201 (22%) |
50 (33%) |
215 (23%) |
36 (29%) |
|||||||||||
|
Missing data |
155 (17%) |
2 (1%) |
149 (16%) |
8 (6%) |
|||||||||||
|
Cerebrovascular disease |
|
|
|
||||||||||||
|
No |
576 (63%) |
107 (71%) |
605 (64%) |
78 (62%) |
|||||||||||
|
Yes |
187 (20%) |
42 (28%) |
190 (20%) |
39 (31%) |
|||||||||||
|
Missing data |
157 (17%) |
2 (1%) |
150 (16%) |
9 (7%) |
|||||||||||
|
Atrial fibrillation |
|
|
|
|
|||||||||||
|
No |
604 (66%) |
109 (72%) |
630 (67%) |
83 (66%) |
|||||||||||
|
Yes |
158 (17%) |
40 (26%) |
163 (17%) |
35 (28%) |
|||||||||||
|
Missing data |
158 (17%) |
2 (1%) |
152 (16%) |
8 (6%) |
|||||||||||
|
Heart failure |
|
|
|
|
|||||||||||
|
No |
656 (71%) |
114 (75%) |
680 (72%) |
90 (71%) |
|||||||||||
|
Yes |
109 (12%) |
34 (23%) |
116 (12%) |
27 (21%) |
|||||||||||
|
Missing data |
155 (17%) |
3 (2%) |
149 (16%) |
9 (7%) |
|||||||||||
|
Chronic lung disease |
|
|
|
||||||||||||
|
No |
622 (68%) |
112 (74%) |
647 (69%) |
87 (69%) |
|||||||||||
|
Yes |
143 (15%) |
37 (25%) |
149 (16%) |
31 (25%) |
|||||||||||
|
Missing data |
155 (17%) |
2 (1%) |
149 (16%) |
8 (6%) |
|||||||||||
|
Asthma |
|
|
|
|
|||||||||||
|
No |
711 (77%) |
130 (86%) |
727 (77%) |
114 (90%) |
|||||||||||
|
Yes |
53 (6%) |
19 (13%) |
68 (7%) |
4 (3%) |
|||||||||||
|
Missing data |
156 (18%) |
2 (1%) |
150 (16%) |
8 (6%) |
|||||||||||
|
Cancer history |
|
|
|
|
|||||||||||
|
No |
647 (70%) |
118 (78%) |
674 (71%) |
91 (72%) |
|||||||||||
|
Yes |
116 (13%) |
31 (21%) |
120 (13%) |
27 (21%) |
|||||||||||
|
Missing data |
157 (17%) |
2 (1%) |
151 (16%) |
8 (6%) |
|||||||||||
|
Hypertension |
|
|
|
|
|||||||||||
|
No |
292 (32%) |
57 (38%) |
302 (32%) |
47 (37%) |
|||||||||||
|
Yes |
478 (52%) |
92 (61%) |
498 (53%) |
72 (57%) |
|||||||||||
|
Missing data |
150 (16%) |
2 (1%) |
145 (15%) |
7 (6%) |
|||||||||||
|
Chronic kidney disease |
|
|
|
||||||||||||
|
No |
580 (63%) |
96 (64%) |
601 (54%) |
75 (60%) |
|||||||||||
|
Yes |
184 (20%) |
53 (35%) |
194 (21%) |
43 (34%) |
|||||||||||
|
Missing data |
156 (17%) |
2 (1%) |
150 (16%) |
8 (6%) |
|||||||||||
|
Body mass index |
|
|
|
|
|||||||||||
|
< 30 kg/m2 |
599 (65%) |
124 (82%) |
622 (66%) |
101 (80%) |
|||||||||||
|
≥ 30 kg/m2 |
118 (13%) |
24 (16%) |
130 (14%) |
12 (10%) |
|||||||||||
|
Missing data |
203 (22%) |
3 (2%) |
193 (20%) |
13 (10%) |
|||||||||||
|
|
|||||||||||||||
|
COVID-19 = coronavirus disease 2019; IQR = interquartile range. * The characteristics of residents by cardiopulmonary resuscitation status are reported in the Supporting Information, table 2. |
|||||||||||||||
Box 2 – Likelihood of hospitalisation for 1071 residential aged care facility residents in the Metro South Hospital and Health Service area of southeast Queensland diagnosed with COVID‐19, 13 December 2021 – 24 January 2022, by clinical characteristic*
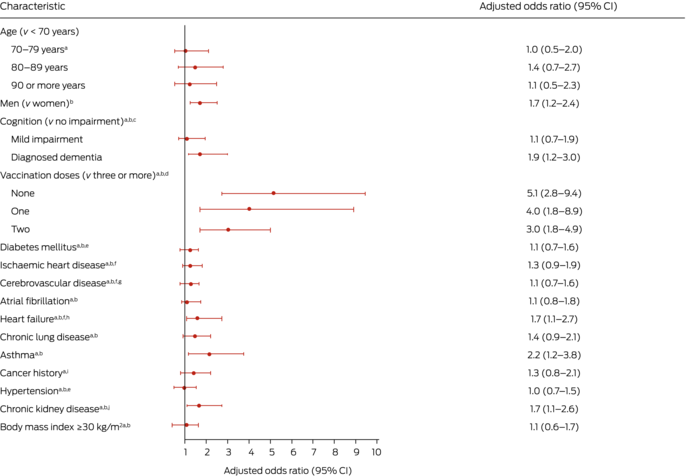
COVID‐19 = coronavirus disease 2019.* The unadjusted (univariable) analysis is reported in the Supporting Information, table 3. Adjustments in multivariable analyses: a. sex; b. age; c. diabetes mellitus, ischaemic heart disease, cerebrovascular disease, hypertension; d. cognition; e. obesity; f. diabetes mellitus, obesity, hypertension, chronic kidney disease; g. atrial fibrillation; h. ischaemic heart disease; i. chronic lung disease; j. diabetes, hypertension, obesity.
Box 3 – Likelihood of death for 1071 residential aged care facility residents in the Metro South Hospital and Health Service area of southeast Queensland diagnosed with COVID‐19, 13 December 2021 – 24 January 2022, by clinical characteristic*
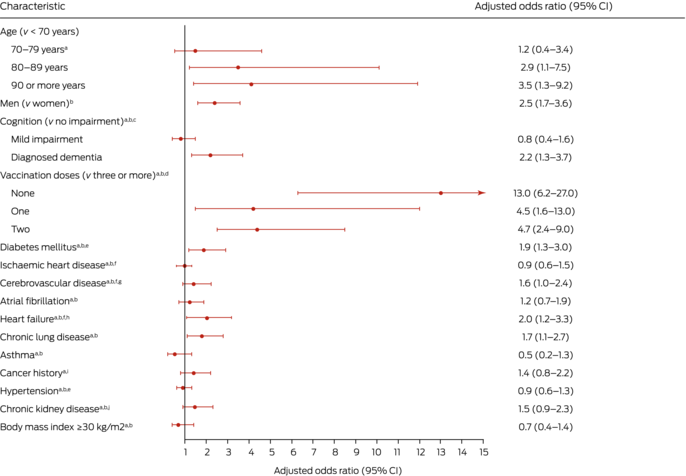
COVID‐19 = coronavirus disease 2019.* The unadjusted (univariable) analysis is reported in the Supporting Information, table 3. Adjustments in multivariable analyses: a. sex; b. age; c. diabetes mellitus, ischaemic heart disease, cerebrovascular disease, hypertension; d. cognition; e. obesity; f. diabetes mellitus, obesity, hypertension, chronic kidney disease; g. atrial fibrillation; h. ischaemic heart disease; i. chronic lung disease; j. diabetes, hypertension, obesity.
Received 19 July 2022, accepted 26 October 2022
- Robert J Ellis1,2,3
- Cameron RM Moffatt1
- Luke T Aaron3
- Greta Beaverson1
- Khin Chaw1,4
- Corinne Curtis1
- Rhett Freeman‐Lamb1
- Deborah Judd1
- Khadija Khatry1,3
- Yee Sum Li1,2
- Terry Nash1,3
- Bonnie Macfarlane1
- Karen Slater1,5
- Yudish Soonarane1
- Mark Stickley1,2
- Satyamurthy Anuradha1,2
- 1 Metro South Public Health Unit, Brisbane, QLD
- 2 The University of Queensland, Brisbane, QLD
- 3 Princess Alexandra Hospital, Brisbane, QLD
- 4 Australian Red Cross Lifeblood, Brisbane, QLD
- 5 Griffith University, Brisbane, QLD
Open access
Open access publishing facilitated by the University of Queensland, as part of the Wiley – the University of Queensland agreement via the Council of Australian University Librarians.
We acknowledge the Metro South Public Health Unit staff who contributed to data collection, compilation, and analysis but were not included as authors of this article. We also thank the residential aged care facility staff for compiling data for outbreak reporting throughout the pandemic.
No relevant disclosures.
- 1. Minister for Health and Aged Care. First confirmed case of novel coronavirus in Australia [media release]. 25 Jan 2020. https://www.health.gov.au/ministers/the‐hon‐greg‐hunt‐mp/media/first‐confirmed‐case‐of‐novel‐coronavirus‐in‐australia (viewed Nov 2022).
- 2. QLD cases: new and cumulative confirmed cases. COVID Live [website]. https://covidlive.com.au/report/daily‐cases/qld (viewed Nov 2022).
- 3. Queensland Government. Border Restrictions Direction (No. 59) (Qld). 30 Dec 2021. https://www.health.qld.gov.au/system‐governance/legislation/cho‐public‐health‐directions‐under‐expanded‐public‐health‐act‐powers/revoked/border‐restrictions‐59 (viewed Nov 2022).
- 4. Miles J, Gramenz E. Queensland COVID‐19 testing data getting “weaker every day”, will impact hospital services. ABC News (Australia), 7 Jan 2022. https://www.abc.net.au/news/2022‐01‐07/qld‐coronavirus‐covid19‐testing‐and‐cases/100736334 (viewed Nov 2022).
- 5. Liu B, Spokes P, He W, Kaldor J. High risk groups for severe COVID‐19 in a whole of population cohort in Australia. BMC Inf Dis 2021; 21: 685.
- 6. Australian Institute of Health and Welfare. The first year of COVID‐19 in Australia: direct and indirect health effects (AIHW cat. no. PHE 287). 10 Sept 2021. https://www.aihw.gov.au/reports/burden‐of‐disease/the‐first‐year‐of‐covid‐19‐in‐australia/summary (viewed Nov 2022).
- 7. Hashan MR, Smoll N, King C, et al. Epidemiology and clinical features of COVID‐19 outbreaks in aged care facilities: a systematic review and meta‐analysis. EClinicalMedicine 2021; 33: 100771.
- 8. Usher K, Durkin J, Gyamfi N, et al. Preparedness for viral respiratory infection pandemic in residential aged care facilities: a review of the literature to inform post‐COVID‐19 response. J Clin Nurs 2021; doi: https://doi.org/10.1111/jocn.15863 [online ahead of print].
- 9. Royal Commission into Aged Care Quality and Safety. Aged care and COVID‐19: a special report. 1 Oct 2020. https://agedcare.royalcommission.gov.au/publications/aged‐care‐and‐covid‐19‐special‐report (viewed Nov 2022).
- 10. COVID‐19 National Incident Room Surveillance Team. COVID‐19 Australia: epidemiology report 58. Reporting period ending 13 February 2022. Commun Dis Intell (2018) 2022; 46.
- 11. Queensland Health. The health of Queenslanders 2020. Hospital and health service profiles from the 2020 Chief Health Officer report: Metro South HHS. 22 Sept 2021. https://public.tableau.com/views/populationprofile/Page1?%3Aembed=y&%3Adisplay=no&%3AshowShareOptions=false&%3AshowVizHome=no (viewed Nov 2022).
- 12. Bhattacharyya RP, Hanage WP. Challenges in inferring intrinsic severity of the SARS‐CoV‐2 Omicron variant. N Engl J Med 2022; 386: e14.
- 13. Jassat W, Abdul Karim SS, Mudara C, et al. Clinical severity of COVID‐19 in patients admitted to hospital during the omicron wave in South Africa: a retrospective observational study. Lancet Glob Health 2022; 10: e961‐e969.
- 14. Tennant E, Fletcher S, Kakar S, et al. Factors associated with adverse outcomes during influenza outbreaks in aged care facilities. Aust N Z J Public Health 2020; 44: 65‐72.
- 15. Merritt TD, Dalton CB, Kakar SR, et al. Influenza outbreaks in aged care facilities in New South Wales in 2017: impact and lessons for surveillance. Commun Dis Intell (2018) 2021; 45.
- 16. Burkett E, Scott I. CARE‐PACT: a new paradigm of care for acutely unwell residents in aged care facilities. Aust Fam Physician 2015; 44: 204‐209.
- 17. Roder C, Maggs C, McNamara BJ, et al. Area‐level social and economic factors and the local incidence of SARS‐CoV‐2 infections in Victoria during 2020. Med J Aust 2022; 216: 349‐356. https://www.mja.com.au/journal/2022/216/7/area‐level‐social‐and‐economic‐factors‐and‐local‐incidence‐sars‐cov‐2‐infections
- 18. Wu M, Wall EC, Carr EJ, et al. Three‐dose vaccination elicits neutralising antibodies against omicron [letter]. Lancet 2022; 399: 715‐717.
- 19. Tan SHX, Pung R, Wang LF, et al. Association of homologous and heterologous vaccine boosters with COVID‐19 incidence and severity in Singapore. JAMA 2022; 327: 1181‐1182.
- 20. Oo NM, Scott IA, Maggacis R, Rajakaruna N. Assessing concordance between patient preferences in advance care plans and in‐hospital care. Aust Health Rev 2019; 43: 425‐431.
- 21. Burgaña Agoües A, Serra Gallego M, Hernández Resa R, et al. Risk factors for COVID‐19 morbidity and mortality in institutionalised elderly people. Int J Environ Res Public Health 2021; 18: 10221.
- 22. Wang Q, Davis PB, Gurney ME, Xu R. COVID‐19 and dementia: analyses of risk, disparity, and outcomes from electronic health records in the US. Alzheimers Dement 2021; 17: 1297‐1306.
- 23. Australian Institute of Health and Welfare. Dementia in Australia (AIHW cat. no. DEM 3). 20 Sept 2021. https://www.aihw.gov.au/reports/dementia/dementia‐in‐australia‐2021‐summary/formats (viewed Nov 2022).
- 24. Holt‐Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta‐analytic review. PLoS Med 2010; 7: e1000316.
- 25. Alves VP, Casemiro FG, de Araujo BG, et al. Factors associated with mortality among elderly people in the COVID‐19 pandemic (SARS‐CoV‐2): a systematic review and meta‐analysis. Int J Environ Res Public Health 2021; 18: 8008.
- 26. Peckham H, de Gruijter NM, Raine C, et al. Male sex identified by global COVID‐19 meta‐analysis as a risk factor for death and ITU admission. Nat Commun 2020; 11: 6317.
- 27. Gordon EH, Hubbard RE. Differences in frailty in older men and women. Med J Aust 2020; 212: 183‐188. https://www.mja.com.au/journal/2020/212/4/differences‐frailty‐older‐men‐and‐women
- 28. Holman N, Knighton P, Kar P, et al. Risk factors for COVID‐19‐related mortality in people with type 1 and type 2 diabetes in England: a population‐based cohort study. Lancet Diabetes Endocrinol 2020; 8: 823‐833.
- 29. Odriozola A, Ortega L, Martinez L, et al. Widespread sensory neuropathy in diabetic patients hospitalized with severe COVID‐19 infection. Diabetes Res Clin Pract 2021; 172: 108631.
- 30. Wang Y, Chen J, Chen W, et al. Does asthma increase the mortality of patients with COVID‐19? A systematic review and meta‐analysis. Int Arch Allergy Immunol 2021; 182: 76‐82.
- 31. Shi T, Pan J, Vasileiou E, et al; Public Health Scotland and the EAVE II Collaborators. Risk of serious COVID‐19 outcomes among adults with asthma in Scotland: a national incident cohort study. Lancet Resp Med 2022; 10: 347‐354.
- 32. Griesel M, Wagner C, Mikolajewska A, et al. Inhaled corticosteroids for the treatment of COVID‐19. Cochrane Database Syst Rev 2022; CD015125.






Abstract
Objective: To identify characteristics associated with the hospitalisation and death of people with COVID‐19 living in residential aged care facilities (RACFs).
Design: Retrospective cohort study.
Setting, participants: All confirmed (polymerase chain reaction testing) or probable SARS‐CoV‐2 infections (rapid antigen tests) in residents of the 86 RACFs in the Metro South Hospital and Health Service area (southeast Queensland), 13 December 2021 – 24 January 2022.
Main outcome measures: Hospitalisation within 14 days or death within 28 days of COVID‐19 diagnosis.
Results: Of 1071 RACF residents with COVID‐19, 151 were hospitalised within 14 days and 126 died within 28 days of diagnosis. Likelihood of death increased with age (per five years: adjusted odds ratio [aOR], 1.38; 95% confidence interval [CI], 1.21–1.57), but not that of hospitalisation. Men were more likely to be hospitalised (aOR, 1.7; 95% CI, 1.2–2.4) or die (aOR, 2.5; 95% CI, 1.7–3.6) than women. The likelihood of hospitalisation was greater for those with dementia (aOR, 1.9; 95% CI, 1.2–3.0), heart failure (aOR, 1.7; 95% CI, 1.1–2.7), chronic kidney disease (aOR, 1.7; 95% CI, 1.1–2.5), or asthma (aOR, 2.2; 95% CI, 1.2–3.8). The likelihood of death was greater for residents with dementia (aOR, 2.2; 95% CI, 1.3–3.7), diabetes mellitus (aOR, 1.9; 95% CI, 1.3–3.0), heart failure (aOR, 2.0; 95% CI, 1.1–3.3), or chronic lung disease (aOR, 1.7; 95% CI, 1.1–2.7). The likelihood of hospitalisation and death were each higher for residents who had received two or fewer vaccine doses than for those who had received three doses.
Conclusions: Most characteristics that influenced the likelihood of hospitalisation or death of RACF residents with COVID‐19 were non‐modifiable factors linked with frailty and general health status. Having received three COVID‐19 vaccine doses was associated with much lower likelihood of hospitalisation or death.