The known: During the first two years of the pandemic, Australian children with COVID-19 were generally less unwell than adults with the disease.
The new: A total of 1193 children and adolescents with SARS-CoV-2 infections presented to nineteen participating hospitals across Australia during 2020–2021. Medical interventions were not required during 795 of 1181 emergency department visits (67%). The 384 admissions to hospital of 341 children (25 under one month of age) included 23 to intensive care; two children died.
The implications: Most children with COVID-19 can be cared for adequately in primary care, relieving the demand for emergency department services.
The first case of coronavirus disease 2019 (COVID-19) in Australia was reported in late January 2020.1 During the first year of the pandemic, most cases were in Victoria.2 With the re-opening of interstate borders in late 2020, case numbers rose in other states but remained markedly higher in Victoria.3 In 2021, the Delta variant of the causative virus, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), became dominant; it was more infectious than the original pandemic strain and caused more severe disease in children. In Victoria, the October 2021 peak in COVID-19 case numbers was higher than the peaks of March and July of 2020.4 It was followed in December 2021 by the rise of the Omicron variant, more infectious than previous strains but causing milder illness.
It was increasingly evident in the course of the pandemic that children with COVID-19 are generally less unwell than adults with the disease.5,6 In Australia, very few children have died of COVID-19, and most deaths were of children with other serious medical conditions. Most experience mild symptoms similar to those of other viral illnesses and can be cared for at home.7 Minimising the number of children with COVID-19 who present to hospitals would both relieve the hospitals, particularly emergency departments (EDs) operating at capacity, and ease the impact of the pandemic on health care workers.8,9
We undertook a multicentre study of the clinical characteristics and short term outcomes for children with COVID-19 who presented to Australian hospitals during the first two years of the pandemic.
Methods
We conducted a multicentre retrospective study of children and adolescents (under 18 years of age) who presented to Paediatric Emergency Departments International Collaborative (PREDICT; https://www.predict.org.au) research network hospitals and for whom positive SARS-CoV-2 test results were recorded during 1 February 2020 – 31 December 2021.
All thirty research-active PREDICT hospitals were invited to participate. We aimed to recruit at least one hospital from each Australian state and territory, including a tertiary hospital in each state, and to include as many active research sites in Victoria as possible (given its high case numbers). Hospitals that responded and could complete regulatory requirements and data extraction participated in our study.
Study procedure
Investigators at each participating hospital extracted from the hospital administrative system a list of children who were positive for SARS-CoV-2 or were diagnosed with COVID-19, and undertook retrospective chart reviews to confirm their eligibility for the study. Data were extracted for children who presented to an ED or who were admitted as inpatients. As only aggregated data were available for children admitted to hospital-in-the-home or virtual care programs, and differences between hospitals in these models of care make comparisons difficult, they were not included in our analysis. The total number of ED presentations during 2019 by people under 18 years of age was also obtained from hospital records.
The de-identified medical records data extracted included demographic characteristics, presenting symptoms and medical history, epidemiological risk factors (overseas travel, contact with people with confirmed SARS-CoV-2 infections), other medical conditions, clinical examination findings, pathology laboratory results, imaging findings, and clinical outcomes, including subsequent hospital presentations, intensive care unit admissions, and death. The data were entered into standardised case report forms in a secure REDCap database hosted by the Murdoch Children's Research Institute, Melbourne.10 Prior to data entry, data abstracters were trained to ensure consistency across participating hospitals, and study materials were piloted; site investigators and data entry personnel entered data for three dummy cases into a test database, the first and second authors checked their accuracy and consistency, and further training was provided if required.
Definitions
SARS-CoV-2 infection status was determined by polymerase chain reaction (PCR) or rapid antigen testing (RAT) of nasal or throat swabs, by serum antibody tests, or was reported by the child or their guardian to a hospital clinician based on testing prior to hospital presentation.
Respiratory support was defined as high flow nasal cannula support, continuous positive airway pressure, or intubation and ventilation. Cardiovascular support was defined as infusion of inotropic or vasoactive agents. Hospital medical intervention was defined as respiratory or cardiovascular support, hydration support via the intravenous or nasogastric routes, antibiotic or antiviral therapy, and other COVID-19-specific treatments, including biologic, anticoagulant, and steroid drugs.
Repeat presentations were defined as presentations with COVID-19 within 14 days of the initial presentation.
Statistical analysis
We summarise data for continuous variables as medians with interquartile ranges (IQRs) or numbers and proportions. We calculated the ratio of COVID-19-related emergency department presentations by children during 2020 and 2021 to the total number of emergency department presentations by people under 18 years of age during 2019 (ie, relative to non-pandemic ED activity). We assessed associations between demographic and clinical factors and hospital admission and medical intervention in univariate and multivariable logistic regression analyses; we report odds ratios (ORs) with 95% confidence intervals (CIs). All demographic variables and clinical features at presentation included in univariate analyses were considered for inclusion in the multivariable model; we report the most parsimonious multivariable model, determined by risk factor inclusion and likelihood ratio tests. Data analyses were undertaken in Stata IC 16.0.
Ethics approval
The Royal Children's Hospital, Melbourne, human research ethics committee provided central ethics approval (HREC63071/RCHM-2020); institutional governance approval was provided by each participating hospital.
Results
Nineteen Australian hospitals, including seven major paediatric tertiary centres, provided data for our analysis: eight in Victoria, three in New South Wales, three in Queensland, and one each in Western Australia, South Australia, the Australian Capital Territory, the Northern Territory, and Tasmania. The three hospitals with the highest COVID-19-related ED and hospital attendance, both in absolute numbers and (for ED attendance) relative to 2019 ED presentation numbers, were in Victoria (Box 1; Box 2). In the fifteen hospitals that could provide the information (all except Austin Hospital, Canberra Hospital, the Royal Darwin and Palmerston Hospital, and the Sunshine Coast University Hospital), a total of 410 326 samples from people under 18 years of age were tested for SARS-CoV-2 during 2020–2021, of which 11 720 were PCR-positive (2.9%).
A total of 1193 SARS-CoV-2-positive children (including 527 girls, 44%) presented to the nineteen participating hospitals during 2020–2021, of whom 1087 had PCR-based test results (91%), twelve had RAT results (1%), and the test type was uncertain (ie, external test results reported by parents or guardians) for 94 (8%). The first positive case was dated 3 February 2020. The 1283 hospital presentations by these children included 90 repeat presentations (7%); there were 125 hospital presentations (107 children) in 2020 and 1158 presentations (1086 children) in 2021. The median age of the children was 3.8 years (IQR, 0.8–11.4 years; range, two days to 17.9 years); 39 were infants less than one month old. Sixty-three children were Aboriginal or Torres Strait Islander people (5%); the Indigenous status of 55 children was unknown (5%).
Epidemiological risk factors
A total of 751 children (63%) had had contact with people who had confirmed SARS-CoV-2 infections, 286 (24%) had no known contact with SARS-CoV-2, and this information was not available for 156 children (13%). Of those with known contact, the infected person was a household member in 583 cases (78%) and people at their schools or childcare centre in 55 cases (7%). Forty-three children (4%) had received one or more COVID-19 vaccine doses.
Clinical characteristics
Symptoms consistent with a viral illness were evident at the time of 1244 presentations (97%). The most frequent symptoms were fever (1207 presentations, 94%), cough (589, 46%), and stuffy or runny nose (479, 37%); children had headache at 116 presentations (9%) and 90 had diarrhoea (7%). Breathing difficulties were reported for 226 presentations (18%), but abnormal lower respiratory tract signs were documented for only 114 (9%); relevant information was not available for 29 presentations (2%). A total of 293 children (25%) had other medical conditions, including asthma (86, 7%), premature birth (68, 6%), cerebral palsy (35, 3%), cardiac disease (25, 2%), immunosuppression (18, 2%), neurological disorders (15, 1%), renal disease (six, 0.5%), and diabetes (five, 0.4%).
Emergency department presentations
There were a total of 1181 ED presentations to the participating hospitals by 1098 children during 2020 and 2021; 77 had two presentations (7%), six had three or four (0.5%). A total of 755 presentations were to Victorian hospitals (64%), including 647 at the Royal Children's, Sunshine, and Northern Hospitals (55%) (Box 1). The median ED length of stay was 3.1 hours (IQR, 1.7–5.0 hours); 437 presentations (37%) lasted four hours or longer. COVID-19 was suspected during 1038 presentations (88%) and was not initially suspected during 91 (8%); this information was not available for 52 presentations (4%). Children were discharged directly home following 764 presentations (65%); in 282 cases (24%) they were admitted to hospital (including sixteen to intensive care units), in 55 (5%) they were admitted to hospital-in-the-home care, and in 80 cases (7%) they were observed for several hours before being discharged home. Hospital medical interventions were not required during 795 ED presentations (67%); respiratory support was provided during 37 presentations (3%), a fluid bolus during 43 (4%), nasogastric hydration during 22 (2%), and cardiovascular support during three (0.3%). There were no deaths.
Children admitted to hospital
Of the 1283 hospital presentations, 384 (30%) involved admission to hospital (102 direct ward admissions, 282 from EDs) by 341 children (including 25 infants under one month of age). A total of 227 admissions were to Victorian hospitals (59%), including 195 to the Royal Children's, Sunshine, and Northern Hospitals (51%). Twenty-three children, including sixteen with pre-existing medical conditions, were admitted to intensive care units (6% of admissions). The median hospital length of stay was three days (IQR, 1–9 days). The primary reasons for the 261 hospital admissions that did not include any further hospital medical intervention (68%) were clinical concern for 70 children (27%), social reasons or parental anxiety in 61 cases (23%), a public health order (in Queensland or New South Wales) in 43 cases (16%), and medical problems related to another medical condition in 17 cases (7%); the reason was not documented for 70 cases (27%) (Supporting Information, table). A total of 123 children admitted as inpatients required additional medical interventions (32%); 55 received intravenous antibiotics (14% of all admitted children), 44 respiratory support (11%), 24 nasogastric hydration (6%), 21 COVID-19-specific medical treatments (5%), and five cardiovascular support (1%). Two children died in intensive care, one of whom had a pre-existing medical condition.
In univariate analyses, statistically significant risk factors for hospitalisation included being under three months of age (v one year to less than six years: OR, 2.6; 95% CI, 1.7–4.0) or having a pre-existing medical condition (OR, 2.5; 95% CI, 1.9–3.2), including premature birth (OR, 2.4; 95% CI, 1.4–3.8), immunosuppression (OR, 6.7; 95% CI, 2.4–18), cerebral palsy (OR, 4.4; 95% CI, 2.2–8.7), and heart disease (OR, 2.3; 95% CI, 1.1–5.1). In the multivariable analysis, none of these risk factors were statistically significant (Box 3). Headache (adjusted OR [aOR], 3.4; 95% CI, 1.5–8.5), difficulties with breathing (aOR, 3.4; 95% CI, 1.4–8.2), and cerebral palsy (aOR, 6.0; 95% CI, 1.2–30) were statistically significant predictors of medical intervention during hospital presentation (Box 4).
Discussion
In our study, the number of children with COVID-19 who presented to the nineteen participating Australian hospitals was ten times as high during 2021 as during 2020. Most presentations were to Victorian hospitals (64% of ED presentations, 59% of hospital admissions). The numbers of presentations to tertiary centres differed between states, but the two hospitals with the highest ratios of COVID-19-related presentations by children during 2021 and 2022 to ED presentations during 2019 were not tertiary paediatric hospitals (Sunshine Hospital, Northern Hospital Epping, both in Victoria), perhaps reflecting greater local transmission in their catchment areas. Higher level medical interventions were not required during most presentations to EDs (67%) and admissions to hospital (68%). Only a small proportion of children admitted to hospital (5%) received COVID-19-specific medications; under the National COVID-19 Taskforce guidelines, children were eligible for treatment with these agents only toward the end of the study period, as the risk of adverse events may not be outweighed by the very low likelihood of progression to severe disease.11
We found that 30% of children with COVID-19 who presented to participating hospitals during the first two years of the pandemic were admitted as inpatients. This was a larger proportion than reported by an international prospective study of SARS-CoV-2-positive children who had presented to EDs (hospital admission, 21%; intensive care unit admission, 13%); the study authors did not report the proportion who received hospital medical interventions.12 A NSW study of children with COVID-19 admitted to hospital (including ambulatory and virtual admissions) found that two-thirds of admissions were for social reasons.13 In our study, ward admissions without further interventions were motivated by social reasons or public health orders in at least 23% of cases, but 30% were the result of clinical or parental concern. Clinicians may have admitted some children for observation because of clinical uncertainty regarding the new virus and reduced access to usual primary care.
In our study, 58% of the children who presented to hospitals were under six years of age, including 25 infants less than one month old admitted to hospital (but none to intensive care). In a recent Swiss study, five of 73 hospitalised neonates with COVID-19 were admitted to intensive care with respiratory failure.14 In general, the possibility of rapid deterioration means that the threshold for admitting infants for observation or empiric intravenous antibiotic therapy is low. The bacteraemia and meningitis risks in younger SARS-CoV-2-positive infants are unknown, but none of the infants in our study developed these complications. Age did not influence the need for medical intervention, but symptoms such as headache, breathing difficulties, and pre-existing asthma, cerebral palsy, or immunosuppression were all statistically significant predictors.
We also found that hospital medical interventions were not required during 67% of ED presentations, which suggests that many children brought to EDs could have been managed in primary care. They may have visited EDs because children with respiratory symptoms had limited access to usual primary care during the pandemic, or because they were referred for in-person assessment after telehealth medical reviews.
We limited our analysis to ED presentations and hospital admissions, rather than including all children who were positive for SARS-CoV-2. Further, we did not include children who received ambulatory or virtual care, about whom we have reported elsewhere.3 Care systems vary considerably between states. Virtual care in NSW and hospital-in-the-home care in Victoria are classified as neither emergency nor hospital admission care, making data capture and comparisons with other care types difficult. The number of ED and hospital presentations in NSW might have been lower because virtual care was available for thousands of children in this state.
We found that COVID-19 cases during the first two years of the pandemic were largely concentrated in a few states, and within a few hospitals within those states. Presentations with other conditions also increased during this period as a direct or indirect consequence of the pandemic, including mental health problem15,16 and seasonal virus infections.17
Limitations
Pandemic-related limitations that hampered governance processes and research capacity prevented some interested hospitals from participating in this study. Similarly, the children we described were infected with SARS-CoV-2 strains that are no longer the dominant circulating variants; nevertheless, our findings remain broadly relevant to managing COVID-19 in children. We collected data retrospectively, following the guidelines for high quality medical records review18 by training study staff, clearly defining inclusion criteria, and using piloted study materials. We may have omitted data for children admitted to hospital with diagnoses other than COVID-19 and discharged before subsequent positive test results were available. Conversely, the test method yielding a positive result was unknown (because it was undertaken in the community) in 8% of the cases we included.
Conclusion
Our analysis of data from a national sample of nineteen Australian hospitals indicates that more than half the children with COVID-19 who visited EDs or were admitted to hospital during the first two years of the pandemic, which included the Delta wave, did not require any medical intervention. Given the still high number of SARS-CoV-2 infections in children and the milder disease course associated with the Omicron strain,19 a focus on service delivery in primary care for people with lower level respiratory problems is needed to ensure that hospitals can concentrate on people with more severe respiratory symptoms.
Box 1 – COVID-19-related hospital admissions and emergency department (ED) presentations for children and adolescents: nineteen participating PREDICT hospitals, 2020 and 2021
|
|
Hospital admissions |
ED presentations |
All ED presentations, 2019* |
2020/2021 ED presentations per 10 000 ED presentations in 2019† |
|||||||||||
|
Hospital |
2020 |
2021 |
2020 |
2021 |
|||||||||||
|
|
|||||||||||||||
|
Royal Children's Hospital, Vic‡ |
14 |
140 |
54 |
313 |
92 327 |
40 |
|||||||||
|
Sunshine Hospital, Vic |
8 |
14 |
42 |
111 |
26 413 |
58 |
|||||||||
|
Northern Hospital Epping, Vic |
1 |
18 |
7 |
120 |
24 089 |
53 |
|||||||||
|
The Children's Hospital at Westmead, NSW‡ |
0 |
36 |
3 |
97 |
64 000 |
16 |
|||||||||
|
John Hunter Hospital, NSW‡ |
0 |
19 |
0 |
90 |
22 817 |
39 |
|||||||||
|
Women's and Children's Hospital, SA‡ |
1 |
15 |
0 |
67 |
47 433 |
14 |
|||||||||
|
Auburn Hospital, NSW |
0 |
4 |
0 |
65 |
6063 |
39 |
|||||||||
|
Gold Coast University Hospital, Qld‡ |
5 |
47 |
1 |
16 |
31 390 |
5 |
|||||||||
|
Queensland Children's Hospital, Qld‡ |
1 |
11 |
3 |
51 |
73 163 |
7 |
|||||||||
|
Box Hill Hospital, Vic |
0 |
20 |
1 |
32 |
13 361 |
40 |
|||||||||
|
University Hospital Geelong, Vic |
0 |
7 |
0 |
30 |
18 698 |
16 |
|||||||||
|
Austin Hospital, Vic |
0 |
5 |
0 |
25 |
17 118 |
15 |
|||||||||
|
Canberra Hospital, ACT |
0 |
9 |
0 |
24 |
25 839 |
9 |
|||||||||
|
Angliss Hospital, Vic |
0 |
0 |
1 |
12 |
11 500 |
10 |
|||||||||
|
Maroondah Hospital, Vic |
0 |
0 |
0 |
7 |
12 018 |
6 |
|||||||||
|
Royal Darwin and Palmerston Hospital, NT |
1 |
7 |
0 |
4 |
19 102 |
2 |
|||||||||
|
Sunshine Coast University Hospital, Qld |
0 |
1 |
0 |
4 |
20 538 |
2 |
|||||||||
|
Perth Children's Hospital, WA‡ |
0 |
0 |
1 |
0 |
69 093 |
< 1 |
|||||||||
|
Royal Hobart Hospital, Tas |
0 |
0 |
0 |
0 |
14 258 |
0 |
|||||||||
|
|
|||||||||||||||
|
COVID-19 = coronavirus disease 2019; PREDICT = Paediatric Emergency Departments International Collaborative. * All presentations by people under 18 years of age. † Total number of ED presentations for COVID-19-related presentations during 2020 and 2021/total number of all ED presentations during 2019 × 10 000. ‡ Tertiary children's hospitals. |
|||||||||||||||
Box 2 – COVID-19-related hospital admissions and emergency department (ED) presentations by children and adolescents: nineteen participating PREDICT hospitals, 2020 and 2021
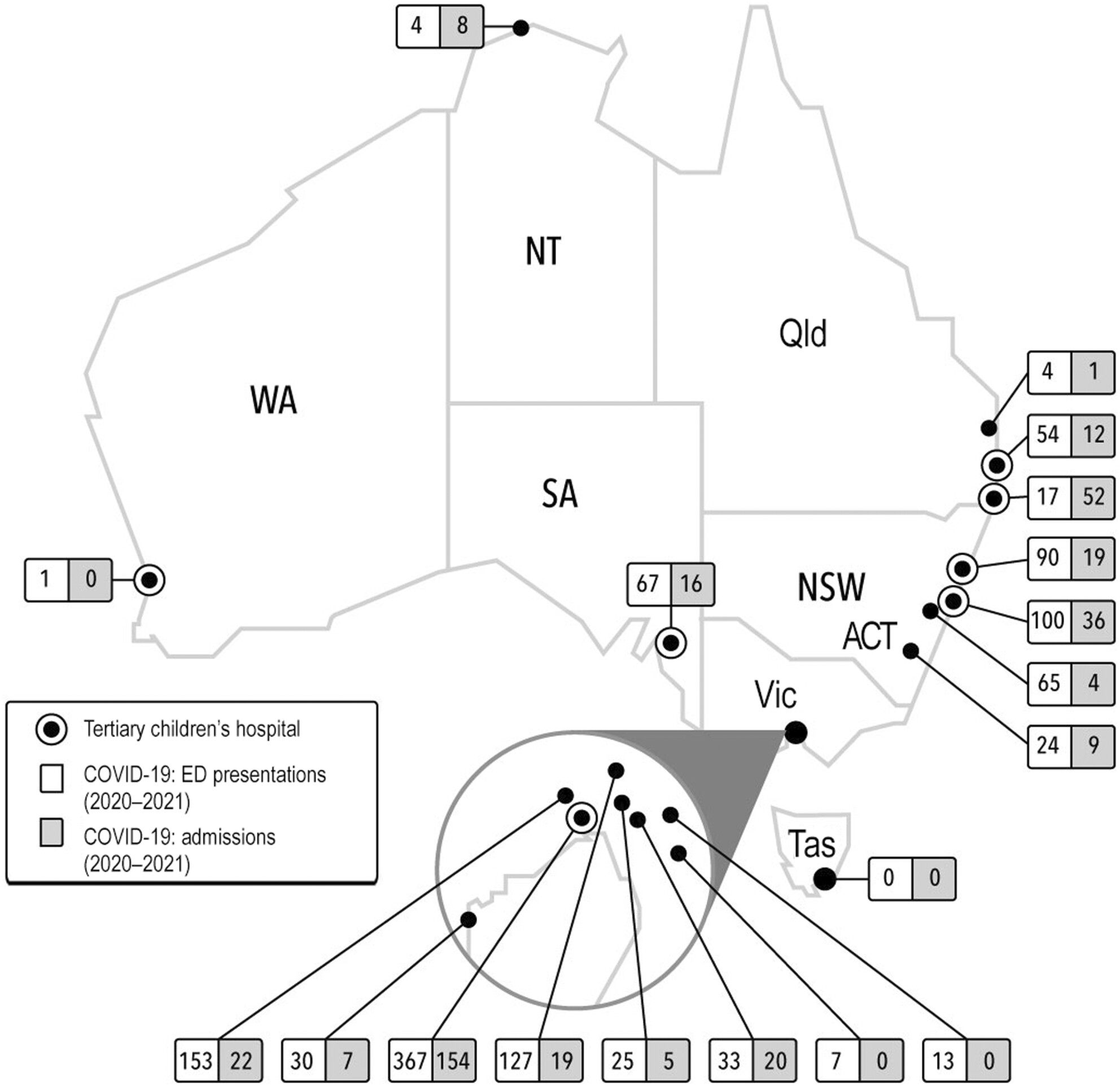
COVID-19 = coronavirus disease 2019.
Box 3 – Characteristics of 1193 SARS-CoV-2-positive children who presented to the nineteen participating PREDICT hospitals, 2020 and 2021, by hospitalisation status (hospitalised v not hospitalised)
|
Characteristic |
All children |
Hospitalised |
Not hospitalised |
Univariate analysis: odds ratio (95% CI) |
Multivariable analysis:* adjusted odds ratio (95% CI) |
||||||||||
|
|
|||||||||||||||
|
Number of children |
1193 |
341 (29%) |
852 (71%) |
|
|
||||||||||
|
Number of presentations |
1283 |
384 (30%) |
899 (70%) |
|
|
||||||||||
|
Sex (girls) |
527 (44%) |
132 (39%) |
395 (47%) |
0.7 (0.6–0.9) |
— |
||||||||||
|
Age |
|
|
|
|
|
||||||||||
|
Less than 3 months old |
118 (10%) |
57 (17%) |
61 (7%) |
2.6 (1.7–4.0) |
— |
||||||||||
|
3 months to less than one year |
223 (19%) |
43 (13%) |
180 (21%) |
0.7 (0.4–1.0) |
— |
||||||||||
|
One year to < 6 years |
353 (30%) |
93 (27%) |
260 (31%) |
1 |
— |
||||||||||
|
6 years to < 11 years |
182 (15%) |
48 (14%) |
134 (16%) |
1.0 (0.7–1.5) |
— |
||||||||||
|
11 years to < 15 years |
171 (14%) |
51 (15%) |
120 (14%) |
1.2 (0.8–1.8) |
— |
||||||||||
|
15 years to < 18 years |
146 (12%) |
49 (14%) |
97 (11%) |
1.4 (0.9–2.1) |
— |
||||||||||
|
Epidemiological risk factors |
|
|
|
|
|
||||||||||
|
Contact with SARS-CoV-2-positive person |
751/1037 (72%) |
244/298 (82%) |
507/739 (69%) |
2.0 (1.5–2.9) |
— |
||||||||||
|
Overseas travel in past 14 days |
36/1063 (3%) |
31/321 (10%) |
5/742 (1%) |
15.8 (6.3–40) |
— |
||||||||||
|
Symptoms/signs at time of swab or subsequent hospital presentation |
|
|
|
|
|
||||||||||
|
Fever (reported or measured) |
1137/1190 (96%) |
331/340 (97%) |
806/850 (95%) |
0.9 (0.7–1.2) |
— |
||||||||||
|
Stuffy/runny nose |
479/987 (49%) |
118/252 (47%) |
361/735 (49%) |
0.9 (0.7–1.2) |
— |
||||||||||
|
Cough |
589/1029 (57%) |
146/258 (57%) |
443/771 (57%) |
1.0 (0.7–1.3) |
— |
||||||||||
|
Sore throat |
202/657 (31%) |
38/174 (22%) |
164/483 (34%) |
0.5 (0.4–0.8) |
— |
||||||||||
|
Headache |
116/318 (36%) |
19/131 (15%) |
97/187 (52%) |
0.2 (0.1–0.3) |
0.2 (0.1–0.4) |
||||||||||
|
Diarrhoea |
90/292 (31%) |
23/135 (17%) |
67/157 (43%) |
0.3 (0.2–0.5) |
— |
||||||||||
|
Difficulty breathing |
226/837 (27%) |
78/222 (35%) |
148/615 (24%) |
1.7 (1.2–2.4) |
0.8 (0.3–2.2) |
||||||||||
|
Pre-existing medical conditions |
|
|
|
|
|
||||||||||
|
Any condition |
293/1161 (25%) |
129/339 (38%) |
164/822 (20%) |
2.5 (1.9–3.2) |
2.8 (0.9–8.6) |
||||||||||
|
Asthma |
86/1115 (8%) |
27/320 (8%) |
59/795 (7%) |
1.1 (0.7–1.8) |
0.4 (0.1–1.9) |
||||||||||
|
Premature birth |
68/1082 (6%) |
32/301 (10%) |
36/772 (5%) |
2.4 (1.4–3.8) |
3.1 (0.4–24) |
||||||||||
|
Immunosuppression/malignancy |
18/1079 (2%) |
13/311 (4%) |
5/768 (1%) |
6.7 (2.4–18) |
— |
||||||||||
|
Cerebral palsy |
35/1083 (3%) |
22/315 (7%) |
13/768 (2%) |
4.4 (2.2–8.7) |
— |
||||||||||
|
Heart disease |
25/1083 (2%) |
12/311 (4%) |
13/772 (2%) |
2.3 (1.1–5.1) |
— |
||||||||||
|
Diabetes mellitus |
6/1055 (0.5%) |
4/302 (1%) |
2/753 (0.3%) |
0.7 (0.3–1.8) |
— |
||||||||||
|
|
|||||||||||||||
|
CI = confidence interval; PREDICT = Paediatric Emergency Departments International Collaborative; SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2. * The model with the best fit is reported here; that is, excluding variables that did not improve model fit. The reference category in each case is the absence of a condition, except for age (reference: one year to less than six years). |
|||||||||||||||
Box 4 – Characteristics of 1193 SARS-CoV-2-positive children who presented to the nineteen participating PREDICT hospitals, 2020 and 2021, by hospital intervention status (medical intervention required v not required)
|
Characteristic |
Hospital medical intervention |
No hospital medical intervention |
Univariate analysis: odds ratio (95% CI) |
Multivariable analysis:* adjusted odds ratio (95% CI) |
|||||||||||
|
|
|||||||||||||||
|
Number of children |
1193 |
344 (29%) |
849 (71%) |
|
|
||||||||||
|
Number of presentations |
1283 |
370 (29%) |
913 (71%) |
|
|
||||||||||
|
Sex (girls) |
527 (44%) |
152 (44%) |
375 (44%) |
1.0 (0.8–1.3) |
— |
||||||||||
|
Age |
|
|
|
|
|
||||||||||
|
Less than 3 months old |
118 (10%) |
29 (8%) |
89 (10%) |
0.8 (0.5–1.2) |
— |
||||||||||
|
3 months to less than one year |
223 (19%) |
56 (16%) |
167 (20%) |
0.8 (0.5–1.1) |
— |
||||||||||
|
One year to < 6 years |
353 (29%) |
107 (31%) |
246 (29%) |
1 |
— |
||||||||||
|
6 years to < 11 years |
182 (15%) |
48 (14%) |
134 (16%) |
0.8 (0.6–1.2) |
— |
||||||||||
|
11 years to < 15 years |
171 (14%) |
56 (16%) |
115 (14%) |
1.1 (0.8–1.7) |
— |
||||||||||
|
15 years to < 18 years |
146 (12%) |
48 (14%) |
98 (12%) |
1.1 (0.7–1.7) |
— |
||||||||||
|
Epidemiological risk factors |
|
|
|
|
|
||||||||||
|
Contact with SARS-CoV-2-positive person |
751/1037 (72%) |
196/299 (66%) |
555/738 (75%) |
0.6 (0.5–0.8) |
— |
||||||||||
|
Overseas travel in past 14 days |
36/1063 (3%) |
2/310 (0.7%) |
34/753 (5%) |
0.1 (0.0–0.6) |
— |
||||||||||
|
Symptoms/signs at time of swab or subsequent hospital presentation |
|
|
|
|
|
||||||||||
|
Fever (reported or measured) |
1137/1190 (96%) |
328/343 (96%) |
809/847 (96%) |
1.0 (0.6–1.9) |
— |
||||||||||
|
Stuffy/runny nose |
479/987 (49%) |
151/301 (50%) |
328/686 (48%) |
1.1 (0.8–1.4) |
— |
||||||||||
|
Cough |
589/1029 (57%) |
194/317 (61%) |
395/712 (55%) |
1.3 (1.0–1.7) |
— |
||||||||||
|
Sore throat |
202/657 (31%) |
66/228 (29%) |
136/429 (32%) |
0.9 (0.6–1.2) |
— |
||||||||||
|
Headache |
116/318 (36%) |
40/67 (60%) |
76/251 (30%) |
3.4 (2.0–5.9) |
3.4 (1.5–8.5) |
||||||||||
|
Diarrhoea |
90/292 (31%) |
26/53 (49%) |
64/239 (27%) |
0.3 (0.2–0.5) |
— |
||||||||||
|
Difficulty breathing |
226/837 (27%) |
97/294 (33%) |
129/543 (24%) |
1.5 (1.2–2.2) |
3.4 (1.4–8.2) |
||||||||||
|
Pre-existing medical conditions |
|
|
|
|
|
||||||||||
|
Any condition |
296/1166 (25%) |
107/337 (32%) |
189/829 (23%) |
1.6 (1.2–2.1) |
0.7 (0.3–1.7) |
||||||||||
|
Asthma |
86/1115 (8%) |
35/314 (11%) |
51/801 (6%) |
1.8 (1.2–2.9) |
— |
||||||||||
|
Prematurity |
68/1082 (6%) |
23/304 (8%) |
45/778 (6%) |
1.3 (0.8–2.2) |
— |
||||||||||
|
Immunosuppression/malignancy |
18/1079 (2%) |
10/303 (3%) |
8/776 (1%) |
3.3 (1.3–8.1) |
— |
||||||||||
|
Cerebral palsy |
35/1083 (3%) |
16/305 (5%) |
19/778 (2%) |
2.2 (1.1–4.3) |
6.0 (1.2–30) |
||||||||||
|
Heart disease |
25/1083 (2%) |
11/303 (4%) |
14/780 (2%) |
2.1 (0.9–4.5) |
— |
||||||||||
|
Diabetes mellitus |
6/1100 (0.5%) |
3/311 (1%) |
3/789 (0.4%) |
1.6 (0.7–3.5) |
— |
||||||||||
|
|
|||||||||||||||
|
CI = confidence interval; PREDICT = Paediatric Emergency Departments International Collaborative; SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2. * The model with the best fit is reported here; that is, excluding variables that did not improve model fit. The reference category in each case is the absence of a condition, except for age (reference: one year to less than six years). |
|||||||||||||||
Received 9 September 2022, accepted 16 March 2023
- Laila Ibrahim1,2
- Catherine Wilson2,3
- Doris Tham2,4
- Mark Corden5
- Shefali Jani6,7
- Michael Zhang3,8
- Amit Kochar9
- Ker Fern Tan10,11
- Shane George12,13
- Natalie T Phillips13,14
- Paul Buntine15,16
- Karen Robins‐Browne17
- Vimuthi Chong18
- Thomas Georgeson19
- Anna Lithgow20
- Sarah Davidson21
- Sharon O'Brien22,23
- Viet Tran24,25
- Franz E Babl2,26
- 1 Royal Children's Hospital, Melbourne, Melbourne, VIC
- 2 Murdoch Children's Research Institute, Melbourne, VIC
- 3 PREDICT Research Network, Melbourne, VIC
- 4 Western Health, Melbourne, VIC
- 5 Northern Hospital Epping, Melbourne, VIC
- 6 The Children's Hospital at Westmead, Sydney, NSW
- 7 The Children's Hospital at Westmead Clinical School, the University of Sydney, Sydney, NSW
- 8 John Hunter Hospital, Newcastle, NSW
- 9 Women's and Children's Hospital, Adelaide, SA
- 10 Auburn Hospital, Sydney, NSW
- 11 University of Notre Dame, Sydney, NSW
- 12 Gold Coast University Hospital, Gold Coast, QLD
- 13 Child Health Research Centre, the University of Queensland, Brisbane, QLD
- 14 Queensland Children's Hospital, Brisbane, QLD
- 15 Eastern Health, Melbourne, VIC
- 16 Eastern Health Clinical School, Monash University, Melbourne, VIC
- 17 University Hospital Geelong, Geelong, VIC
- 18 Austin Hospital, Melbourne, VIC
- 19 Canberra Hospital, Canberra, ACT
- 20 Royal Darwin and Palmerston Hospital, Darwin, NT
- 21 Sunshine Coast University Hospital, Sunshine Coast, QLD
- 22 Perth Children's Hospital, Perth, WA
- 23 Curtin University, Perth, WA
- 24 Royal Hobart Hospital, Hobart, TAS
- 25 Tasmanian School of Medicine, University of Tasmania, Hobart, TAS
- 26 The University of Melbourne, Melbourne, VIC
Open access:
Open access publishing facilitated by The University of Melbourne, as part of the Wiley – The University of Melbourne agreement via the Council of Australian University Librarians.
We acknowledge the support of the National Health and Medical Research Council (NHMRC) through a Centre of Research Excellence grant for Paediatric Emergency Medicine (1171228), which also supported Catherine Wilson, who coordinated the study and data collection across the PREDICT network. Franz Babl is supported by an NHMRC Practitioner Fellowship (1124468), which partially supported his role as a senior author and principal investigator for this study.
We also acknowledge the assistance of the hospital staff who assisted with data retrieval: Katrina Pandey and James Gaston (Sunshine Hospital, Western Health); Deepali Thosar (the Children's Hospital at Westmead); Giles Barrington (Royal Hobart Health Service); Amelia Skaczkowski (Royal Darwin Hospital); Jo Miller, Ethan Fernandes, Andrew McGlinchy, Ye Yang Tham, and Olivia Slifirski (Eastern Health: Box Hill, Maroondah, and Angliss hospitals); Gaby Nieva and Lara Caruso (Adelaide Women's and Children's Hospital); Angus Jones and Alyce Callaghan (Queensland Children's Hospital); and Nitaa Eapen, Yilin Liu, Karen Lu, Violet Sattari Bahri, Michael Wojno, Haoyue Zhang, and Zahra Ataie‐Ashtiani (Royal Children's Hospital).
No relevant disclosures.
- 1. 2019‐nCoV National Incident Room Surveillance Team. 2019‐nCoV acute respiratory disease, Australia: epidemiology report 1 (reporting week 26 January – 1 February 2020). Commun Dis Intell (2018) 2020; 44.
- 2. Ibrahim LF, Tosif S, McNab S, et al. SARS‐CoV‐2 testing and outcomes in the first 30 days after the first case of COVID‐19 at an Australian children's hospital. Emerg Med Australas 2020; 32: 801‐808.
- 3. Ibrahim LF, Tham D, Chong V, et al. The characteristics of SARS‐CoV‐2‐positive children who presented to Australian hospitals during 2020: a PREDICT network study. Med J Aust 2021; 215: 217‐221. https://www.mja.com.au/journal/2021/215/5/characteristics‐sars‐cov‐2‐positive‐children‐who‐presented‐australian‐hospitals
- 4. COVID‐19 National Incident Room Surveillance Team. COVID‐19 Australia: epidemiology report 56: reporting period ending 5 December 2021. Commun Dis Intell (2018) 2021; 45.
- 5. Zimmermann P, Curtis N. Why is COVID‐19 less severe in children? A review of the proposed mechanisms underlying the age‐related difference in severity of SARS‐CoV‐2 infections. Arch Dis Child 2021; 106: 429‐439.
- 6. Neeland MR, Bannister S, Clifford V, et al. Innate cell profiles during the acute and convalescent phase of SARS‐CoV‐2 infection in children. Nat Commun 2021; 12: 1084.
- 7. Zimmermann P, Pittet LF, Finn A, et al. Should children be vaccinated against COVID‐19? Arch Dis Child 2022; 107: e1.
- 8. Mediavilla R, Fernández‐Jiménez E, Martinez‐Morata I, et al. Sustained negative mental health outcomes among healthcare workers over the first year of the COVID‐19 pandemic: a prospective cohort study. Int J Public Health 2022; 67: 1604553.
- 9. Hoang KTA, Morris RW, Naehrig DN, Glozier N. The comparative mental health of Australian doctors before and during COVID‐19: a population‐based approach. Aust N Z J Psychiatry 2022; 57: 511‐519.
- 10. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap): a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42: 377‐381.
- 11. Fraile Navarro D, Tendal B, Tingay D, et al. Clinical care of children and adolescents with COVID‐19: recommendations from the National COVID‐19 Clinical Evidence Taskforce. Med J Aust 2022; 216: 255‐263. https://www.mja.com.au/journal/2022/216/5/clinical‐care‐children‐and‐adolescents‐covid‐19‐recommendations‐national‐covid
- 12. Funk AL, Florin TA, Kuppermann N, et al; Pediatric Emergency Research Network‐COVID‐19 Study Team. Outcomes of SARS‐CoV‐2‐positive youths tested in emergency departments: the Global PERN‐COVID‐19 Study. JAMA Netw Open 2022; 5: e2142322.
- 13. Williams P, Koirala A, Saravanos GL, et al. COVID‐19 in New South Wales children during 2021: severity and clinical spectrum. Med J Aust 2022; 217: 303‐310. https://www.mja.com.au/journal/2022/217/6/covid‐19‐new‐south‐wales‐children‐during‐2021‐severity‐and‐clinical‐spectrum
- 14. Zimmermann P, Uka A, Buettcher M, et al; Swiss Paediatric Surveillance Unit. Neonates with SARS‐CoV‐2 infection: spectrum of disease from a prospective nationwide observational cohort study. Swiss Med Wkly 2022; 152: w30185.
- 15. Carison A, Babl FE, O'Donnell SM. Increased paediatric emergency mental health and suicidality presentations during COVID‐19 stay at home restrictions. Emerg Med Australas 2022; 34: 85‐91.
- 16. Hiscock H, Chu W, O'Reilly G, et al. Association between COVID‐19 restrictions and emergency department presentations for paediatric mental health in Victoria, Australia. Aust Health Rev 2022; 46: 529‐536.
- 17. Eden JS, Sikazwe C, Xie R, et al; Australian RSV study group. Off‐season RSV epidemics in Australia after easing of COVID‐19 restrictions. Nat Commun 2022; 13: 2884.
- 18. Kaji AH, Schriger D, Green S. Looking through the retrospectoscope: reducing bias in emergency medicine chart review studies. Ann Emerg Med 2014; 64: 292‐298.
- 19. Wolter N, Jassat W, Walaza S, et al. Early assessment of the clinical severity of the SARS‐CoV‐2 omicron variant in South Africa: a data linkage study. Lancet 2022; 399: 437‐446.






Abstract
Objectives: To examine the clinical characteristics and short term outcomes for children with severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infections who presented to Australian hospitals during 2020 and 2021.
Design, setting: Retrospective case review study in nineteen hospitals of the Paediatric Research in Emergency Departments International Collaborative (PREDICT) network from all Australian states and territories, including seven major paediatric tertiary centres and eight Victorian hospitals.
Participants: SARS‐CoV‐2‐positive people under 18 years of age who attended emergency departments or were admitted to hospital during 1 February 2020 – 31 December 2021.
Main outcome measures: Epidemiological and clinical characteristics, by hospital care type (emergency department [ED] or inpatient care).
Results: A total of 1193 SARS‐CoV‐2‐positive children and adolescents (527 girls, 44%) attended the participating hospitals (107 in 2020, 1086 in 2021). Their median age was 3.8 years (interquartile range [IQR], 0.8–11.4 years); 63 were Aboriginal or Torres Strait Islander people (5%). Other medical conditions were recorded for 293 children (25%), including asthma (86, 7%) and premature birth (68, 6%). Medical interventions were not required during 795 of 1181 ED presentations (67%); children were discharged directly home in 764 cases (65%) and admitted to hospital in 282 (24%; sixteen to intensive care units). The 384 admissions to hospital (including 102 direct admissions) of 341 children (25 infants under one month of age) included 23 to intensive care (6%); the median length of stay was three days (IQR, 1–9 days). Medical interventions were not required during 261 admissions (68%); 44 children received respiratory support (11%) and 21 COVID‐19‐specific treatments, including antiviral and biologic agents (5%). Being under three months of age (v one year to less than six years: odds ratio [OR], 2.6; 95% confidence interval [CI], 1.7–4.0) and pre‐existing medical conditions (OR, 2.5; 95% CI, 1.9–3.2) were the major predictors of hospital admission. Two children died, including one without a known pre‐existing medical condition.
Conclusion: During 2020 and 2021, most SARS‐CoV‐2‐positive children and adolescents who presented to participating hospitals could be managed as outpatients. Outcomes were generally good, including for those admitted to hospital.