Health professionals must be prepared to address the health risks and impacts of climate change
Between 2030 and 2050, climate change is expected to cause about 250 000 additional deaths per year.1 This does not include deaths from pollution, mental illness, extreme weather events and resultant migration and conflict, all of which carry significant morbidity and mortality risks. The medical profession has a responsibility to prepare practitioners and the health system for the escalating challenges of this health crisis.
Even though planetary health frameworks, consensus statements, and early teaching experience have begun to be reported,2,3,4,5,6,7,8,9,10 persistent barriers to the implementation of planetary health concepts, including the health impacts of climate change and the principles of sustainable health care, are evident within medical education.11,12 Consequently, the implementation of this content into predominantly biomedically focused curricula is frequently piecemeal, opportunistic, unidirectional and poorly related to clinical practice.13,14
Internationally, the emerging curriculum principles to address this challenge align with global health priorities. Specifically, addressing the socio‐economic and environmental determinants of health under the United Nations Sustainable Development Goals framework (https://sdgs.un.org/goals), indigenous eco‐health‐centric leadership, promotion of systems thinking and change, and experiential, practice‐based learning that cultivates interprofessional teamwork, advocacy and leadership development.3,4,5,6,7,9,10,15 A 2019 interactive perspective provides a useful open access resource in this direction.16 More recently, Emory University students and staff reported their experience in the incorporation of climate content into selected aspects of the pre‐clinical curriculum.17
In Australia, Medical Deans of Australia and New Zealand (MDANZ) established a Climate Change and Health Working Group, which has proposed graduate outcome statements and learning objectives that incorporate the environment as a health determinant, health care sustainability, and the health effects of climate change.18,19 At the time of publication, the Australian Medical Council is reviewing the accreditation standards of primary medical programs and has released updates to the National Framework for Prevocational Medical Training, strengthening a top‐down national approach to producing climate‐aware and prepared practitioners.
There are many steps between developing new accreditation standards and actual delivery to learners. The three key strategies are: i) integrate climate change as a cross‐cutting core theme, ii) facilitate educators and students sharing knowledge and teaching one another in this emerging field, and iii) relate learning to clinical practice.11 An intermediate step is to link existing organ systems focused preclinical studies with the impacts of climate change on the health of individual patients.
Codevelopment of a planetary health–organ system map
In response to these challenges, students and faculty volunteers, all members of the Doctors for the Environment Australia at the University of Melbourne, collaborated to form the Planetary Health Curriculum Taskforce. This group was driven by student advocacy seeking to address a perceived gap in their curriculum. We contend that such cocreation is essential to accelerate the integration of such urgently needed curriculum content by adopting the highest level of pedagogical methods and to model the intergenerational collaboration required to address this “wicked” challenge.
We sought to achieve three objectives (Box 1) and conducted our work in three phases (Box 2). First, student focus groups from all years of the medical school identified planetary health learning opportunities within the existing curriculum structure.
Second, we did a structured literature review, via two student and faculty workshops, to map climate change and health literature content and themes to the classical organ systems framework of first year medicine (Box 3). We incorporated the principles of sustainable health care, such as environmental footprint assessment and valuing the health cobenefits of decarbonisation, as well as the opportunities for medical students to learn applied skills and behaviour. Engagement with the First Nations health team helped us to incorporate Indigenous‐led content, an identified area for further action by Australian and New Zealand public health and medical educators.12
Phase three consisted of expert peer review by seven specialist, generalist and public health clinicians with teaching and research experience in climate change and health. Each clinician was allocated two organ system blocks and instructed to review and edit content for clinical relevance, strength of evidence, and quality of writing.
The final synthesis, inclusion of images, figures and executive summaries were completed by the Curriculum Taskforce student members, with design support from Doctors for the Environment Australia. The outcome was an infographic‐rich curriculum resource, a planetary health–organ system map,20 which is being used as a resource in first year medical teaching.
A guide for climate change integration at all levels of medical education
Our systematic, student and faculty codeveloped process and clinical focus are an example to others seeking successful integration of planetary health into their curricula. Central to our approach was the application of the three selected models (Box 3). This process identified and explored the multidirectional relationships between broad public and planetary health content and person‐centred biophysiological mechanisms. We achieved this by connecting literature content using Model 1 headings (eg, cardiovascular organ system) and Model 2 (relevant social determinants of health) and Model 3 content (relevant major consequences of climate change). As an example, Box 4 shows a mechanism for heatwave‐associated acute myocardial infarction from the planetary health–organ system map.
There is clear recognition by peak Australian medical bodies of the importance of climate change and our professions’ role not just in preparing practitioners, but in advocating for climate‐conscious health care and broader mitigation policies.21,22 This has led to an emergent discussion about planetary health at all levels of Australian medical education. Our methodology and output may assist medical educators in addressing the challenges of integrating climate change education into their own teaching.11
For example, as this approach enables students to share their knowledge and experiences with teachers outside of formal classroom boundaries, it may support the evident lack of medical educators proficient in planetary health teaching. Empowering students as leaders and partners in learning and developing education material is known to improve their effectiveness as learners and confidence in teaching.23 It also explicitly promotes higher order relational and extended abstract reasoning by students (Blooms’ revised taxonomy levels 4–6) — the ultimate task of any curriculum.24 Despite not being formally evaluated, we observed that the students involved in this project achieved the Association for Medical Education in Europe (AMEE) planetary health and education for sustainable health care consensus statement aims of “knowledge, skills, values, competence and confidence”.9 Our mapping output also addresses the need for learning resources that are centralised, accessible and frequently peer reviewed.
Our focus on clinical relevance helped narrow the scope of literature and developed the curriculum resource towards use in practice. This strategy connected theory with patient care in a way that ensured concepts could be translated into clinical skills. Even though it was designed for one context, the organ systems structure and clinical relevance also allow learning points to be drawn from this resource for prevocational, vocational and continuing professional development teaching.
Our approach also aligns with recent understanding that planetary health is a theme akin to ethics or leadership that should spiral through the core curriculum.11 In this context, biomedical planetary health learning primes students for subsequent clinical training.
Our initial successes, including deriving a climate change‐themed tutorial from the map and precipitating a review of planetary health curriculum opportunities within the Doctor of Medicine (MD) program redesign, parallel those of the Emory student–staff collaboration.17 The process of expanding the map to cover more of the MD curriculum, regular peer review of emerging evidence and increasing interprofessional collaboration is ongoing and has garnered formal support through seed grant funding.25 We encourage the formal recognition of planetary health as core to any medical curriculum, with dedicated resourcing from the top‐down and codesign from the bottom‐up. We recognise and value the concurrent higher level advocacy of the MDANZ Climate Change and Health Working Group in supporting our grassroots project,18,19 as well as allyship from our interprofessional and First Nations health colleagues.25
A remaining challenge, given the assessment‐driven nature of medicine, is the development of “assessment for learning” inclusive of planetary health. We have not reviewed the assessment blueprint of the University of Melbourne MD program. However, we propose this as a valuable exercise, as assessment often strongly correlates with students’ prioritisation of content.26
Ultimately, the role of medical professionals in providing leadership, advocating for sustainable health care and adopting evidence‐based strategies for the management of planetary health‐related risks has been widely acknowledged.9,21,22 Our methodology to generate the planetary health–organ system map presents a model for engaging learners through codevelopment of a novel learning resource. Our infographic‐rich map also provides an example of systematic integration with existing curricula and an opportunity for strengthening planetary health leadership in medical education.
Box 1 – Methods used to meet project objectives
|
Primary objectives |
Methods |
||||||||||||||
|
|
|||||||||||||||
|
Identify current first‐year curriculum alignment with existing Graduate Student Outcomes |
|
||||||||||||||
|
Exemplify the integration of planetary health as a cross‐cutting theme with particular focus on the mechanistic impacts of climate change on patients and practice; identify and embed shared learning objectives |
|
||||||||||||||
|
Specify opportunities to integrate principles of sustainable health care |
|
||||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 2 – Project phases and outline of creating a planetary health–organ system map
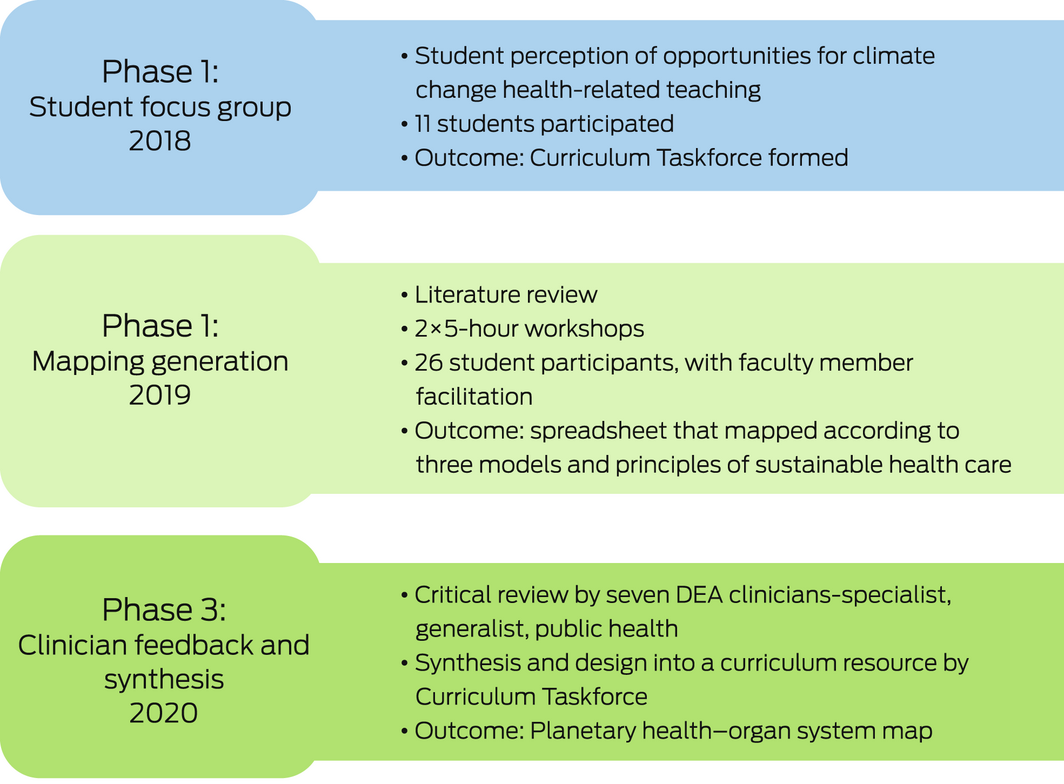
DEA = Doctors for the Environment Australia.
Box 3 – The three models used to map the literature on human health and the health of the planet
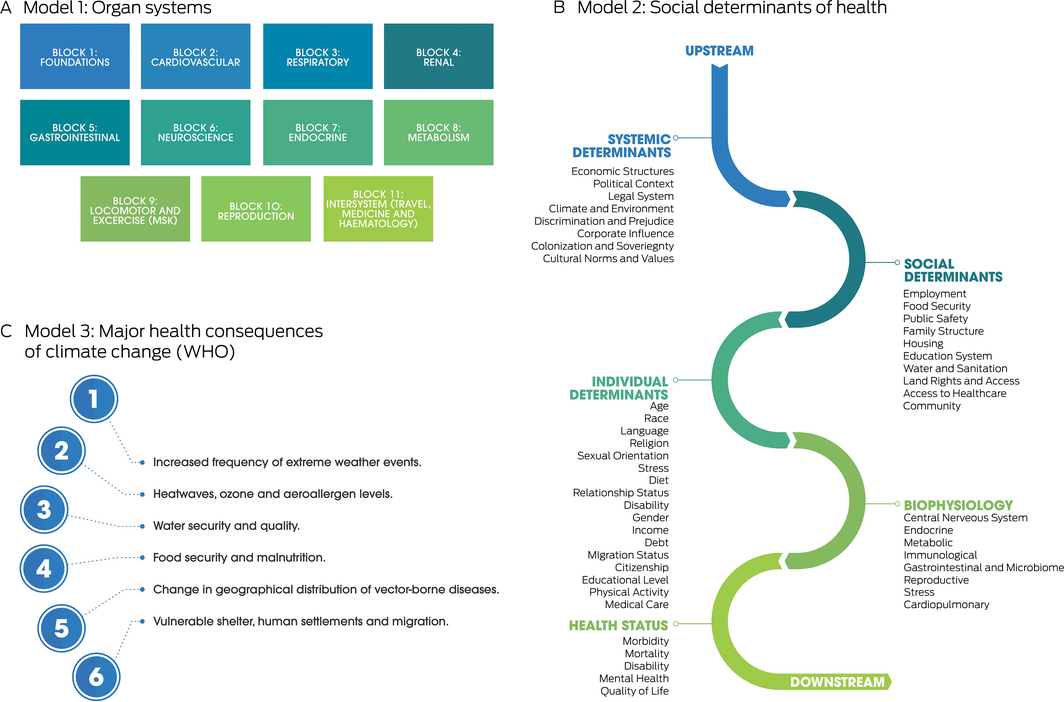
WHO = World Health Organization. Source: Reproduced with permission from Burch et al.20
Box 4 – Example mechanism for heatwave‐associated acute myocardial infarction from the planetary health–organ system map
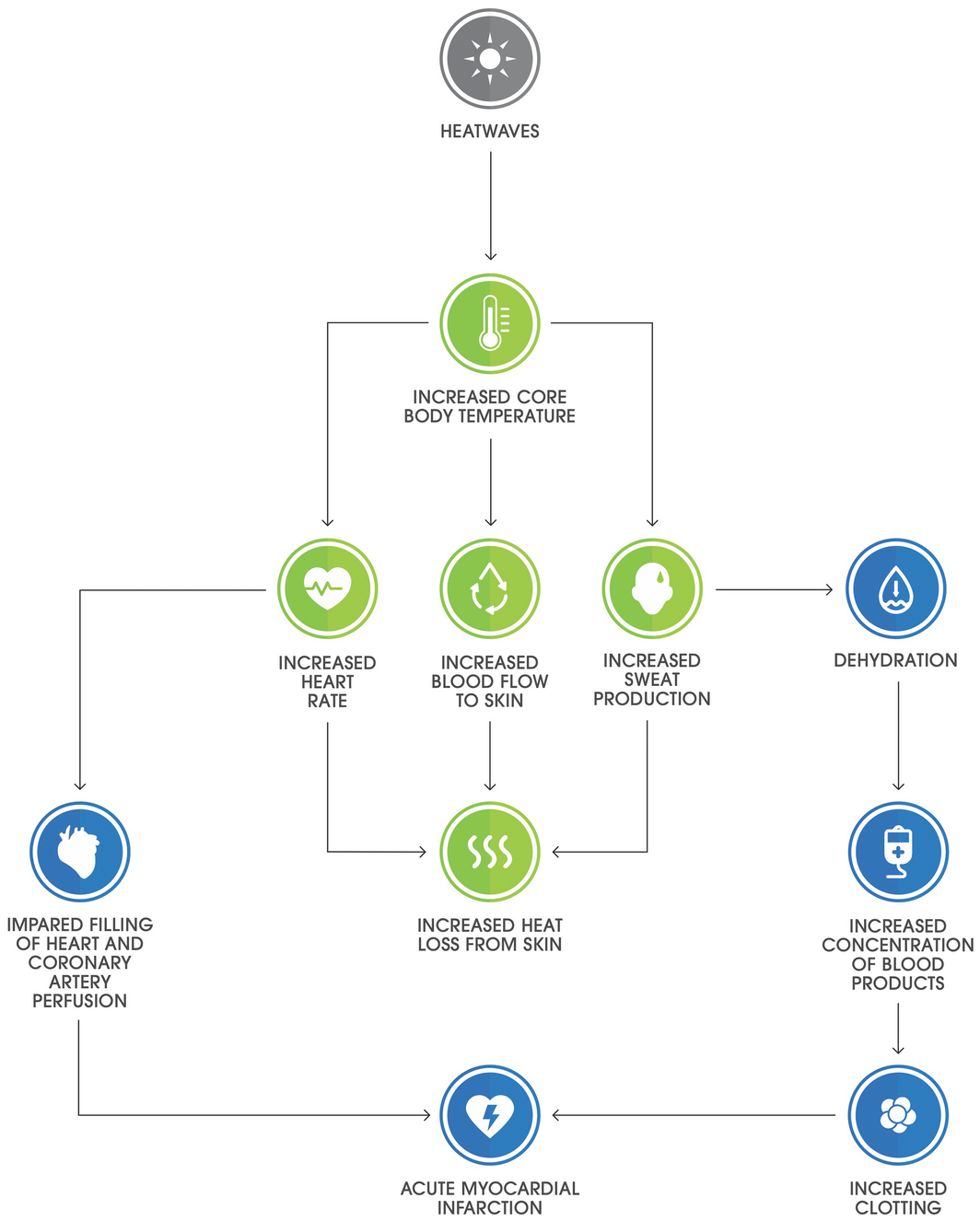
Source: Reproduced with permission from Burch et al.20
Provenance: Not commissioned; externally peer reviewed.
- 1. Romanello M, McGushin A, Di Napoli C, et al. The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future. Lancet 2021; 398: 1619‐1662.
- 2. Brand G, Collins J, Bedi G, et al. “I teach it because it is the biggest threat to health”: integrating sustainable healthcare into health professions education. Med Teach 2021; 43: 325‐333.
- 3. Gomez J, Goshua A, Pokrajac N, et al. Teaching medical students about the impacts of climate change on human health. J Clim Chang Health 2021; 3: 100020.
- 4. Guzmán CAF, Aguirre AA, Astle B, et al. A framework to guide planetary health education. Lancet Planet Health 2021; 5: e253‐e255.
- 5. Hackett F, Got T, Kitching GT, et al. Training Canadian doctors for the health challenges of climate change. Lancet Planet Health 2020; 4: e2‐e3.
- 6. Hansen M, Rohn S, Moglan E, et al. Promoting climate change issues in medical education: Lessons from a student‐driven advocacy project in a Canadian Medical school. J Clim Chang Health 2021; 3: 100026.
- 7. Maxwell J, Blashki G. Teaching about climate change in medical education: an opportunity. J Public Health Res 2016; 5: 673.
- 8. Medical students and faculty from 74 medical schools in the US, UK, Ireland, Canada, Germany, Malaysia, and Japan. 2021–2022 Summary report and international health student initiative. https://phreportcard.org/wp‐content/uploads/2022/04/2022‐PHRC‐Summary‐Report_FINAL.pdf (viewed Sept 2022).
- 9. Shaw E, Walpole S, McLean M, et al. AMEE Consensus Statement: Planetary health and education for sustainable healthcare. Med Teach 2021; 43: 272‐286.
- 10. Walpole SC, Mortimer F. Evaluation of a collaborative project to develop sustainable healthcare education in eight UK medical schools. Public Health 2017; 150: 134‐148.
- 11. Tun S. Fulfilling a new obligation: teaching and learning of sustainable healthcare in the medical education curriculum. Med Teach 2019; 41: 1168‐1177.
- 12. Lal A, Walsh EI, Wetherell A, Slimings C. Climate change in public health and medical curricula in Australia and New Zealand: a mixed methods study of educator perceptions of barriers and areas for further action. Environ Educ Res 2022; 7: 1070‐1087.
- 13. Bell EJ. Climate change: what competencies and which medical education and training approaches? BMC Med Educ 2010; 10: 31.
- 14. Sharma M, Pinto AD, Kumagai AK. Teaching the social determinants of health: a path to equity or a road to nowhere? Acad Med 2018; 93: 25‐30.
- 15. Schwerdtle N, Horton G, Kent F, et al. Education for sustainable healthcare: a transdisciplinary approach to transversal environmental threats. Med Teach 2020; 42: 1102‐1106.
- 16. Salas RN, Solomon CG. The climate crisis — health and care delivery. N Engl J Med 2019; 381: e13.
- 17. Rabin BM, Laney EB, Philipsborn RP. The unique role of medical students in catalyzing climate change education. J Med Educ Curric Dev 2020; 7: 2382120520957653.
- 18. Madden DL, Horton GL, McLean M. Preparing Australasian medical students for environmentally sustainable health care. Med J Aust 2022; 216: 225‐229. https://www.mja.com.au/journal/2022/216/5/preparing‐australasian‐medical‐students‐environmentally‐sustainable‐health‐care
- 19. Madden DL, McLean M, Horton GL. Preparing medical graduates for the health effects of climate change: an Australasian collaboration. Med J Aust 2018; 208: 291‐292. https://www.mja.com.au/journal/2018/208/7/preparing‐medical‐graduates‐health‐effects‐climate‐change‐australasian
- 20. Burch H, Watson B, Simpson G, et al. Mapping climate change and health into the medical curriculum: co‐development of a “planetary health–organ system map” for graduate medical education. Melbourne: Doctors for the Environment Australia, 2021. https://dea.org.au/wp‐content/uploads/2022/03/Mapping‐Climate‐Change‐FINAL‐v3‐compressed.pdf (viewed Apr 2021).
- 21. Australian Medical Association, Doctors for the Environment Australia. Joint statement — medical professionals call for emissions reduction in healthcare 2021 [media release]. 17 March 2021 https://www.dea.org.au/wp‐content/uploads/2021/03/170321‐Joint‐statement‐Medical‐Professionals‐call‐for‐emissions‐reduction‐in‐health‐care.pdf (viewed Apr 2021).
- 22. Council of Presidents of Medical Colleges. Managing and responding to climate risks in healthcare. Canberra: CPMC, 2018. https://cpmc.edu.au/communique/managing‐and‐responding‐to‐climate‐risks‐in‐healthcare (viewed Apr 2021).
- 23. Yeung C, Friesen F, Farr S, et al. Development and implementation of a longitudinal students as teachers program: participant satisfaction and implications for medical student teaching and learning. BMC Med Educ 2017; 17: 28.
- 24. Anderson LW, Krathwohl DR. A taxonomy for learning, teaching, and assessing: a revision of Bloom’s taxonomy of educational objectives. New York: Addison Wesley Longman, 2001.
- 25. Remedios L, Winkel KD. Education for sustainable healthcare: setting the educational agenda for our future. Focus on Health Professional Education: A Multi‐disciplinary Journal 2022; 23: i‐v.
- 26. Ferris HA, O’Flynn D, Flynn O. Assessment in medical education; what are we trying to achieve? Int J High Educ 2015; 4.






Open access
Open access publishing facilitated by The University of Melbourne, as part of the Wiley ‐ The University of Melbourne agreement via the Council of Australian University Librarians.
We thank the members of Doctors for the Environment Australia (DEA) for their clinical and research expertise, and the organisation for its graphic support to produce our final curriculum mapping resource.
No relevant disclosures.