The known: Stroke‐related disability is greater for women than men, and their subsequent quality of life poorer. Investigations of sex differences in pre‐hospital emergency medical service care for people with stroke have yielded inconsistent results.
The new: Women subsequently admitted to hospital with stroke were more likely than men to arrive by ambulance, but less likely to receive stroke‐specific management during their journey. Among people under 70, women with stroke were more likely than men to be diagnosed by paramedics with conditions other than stroke.
The implications: Refining the assessment of symptoms in women in pre‐hospital emergency services care could improve patient outcomes.
Landmark trials of intravenous thrombolysis1 and endovascular thrombectomy2 have transformed acute stroke care in recent years. As the efficacy of these treatments is highly time‐dependent, rapid pre‐hospital assessment is critical for optimising outcomes, and emergency medical services play a major role in realising their potential benefits.
Differences in pre‐hospital activation of emergency medical services for men and women with stroke have been examined in several studies (Supporting Information, table 1). Some investigators found no sex differences,3 others that women were more likely to be transported to hospital by ambulance,4 or that the mean time between symptom onset and presenting to hospital was longer for women than men.5 However, most studies were not population‐based and sample sizes were small. As many investigations were not designed to detect sex differences in pre‐hospital activation of emergency medical services, they did not consider important confounding factors, such as age.3,4,5
It is recognised that atypical clinical manifestations of stroke on initial presentation are more frequent in women.6 Further, a large United States study found that the proportion of missed stroke diagnoses was nearly seven times as large for patients aged 18–44 years presenting to emergency departments (4.0%) as for those aged 75 years or more (0.6%).7
In our population‐based study, we examined the pre‐hospital care and management provided by emergency medical services to people admitted to hospital in New South Wales with stroke diagnoses. We investigated whether pre‐hospital emergency medical services care was different for women and men, and whether any sex differences were influenced by age.
Methods
We analysed linked administrative data for women and men admitted to NSW hospitals during 1 July 2005 – 31 December 2018 with a principal diagnosis and one additional diagnosis code for stroke at separation (International Classification of Diseases, tenth revision, Australian modification [ICD‐10‐AM] codes I60–68, G45) and no previous admissions with a stroke diagnosis in any diagnosis field after 31 July 2001 (ie, lookback period of four years).
The NSW Admitted Patient Data Collection (APDC) includes hospital records from all NSW public and private hospitals and day procedure centres. APDC records include demographic data (age, sex, marital status, country of birth, Indigenous status, hospital region) and clinical code information (diagnoses during the episode of care).
NSW Ambulance data collections contain operational information from the computer‐aided dispatch system and information documented by paramedics in the patient health care record (PHCR) or electronic medical record (eMR). The PHCR database comprises electronic transcripts of paramedics’ paper case sheets, while eMR data are directly derived from electronic case sheets entered into the eMR system from devices in the ambulance. The eMR has been the preferred format since its staged introduction in 2010, but the PHCR is still used for some care episodes.
Study factors
The NSW Ambulance eMR (but not the PHCR) captures the documented assessments of patients by paramedics. The assessments we considered in our study were cerebrovascular and cardiovascular conditions, as well as stroke mimics: acute coronary syndrome, acute myocardial infarction, acute pulmonary oedema, anxiety, arrhythmia, cardiac arrest, collapse, dizziness, emotional distress, faint, headache, hyperglycaemia, hypoglycaemia, hypertension, hypotension, hyperventilation, migraine, mobility problem, nausea, pain, psychiatric episode, seizure, stroke, subarachnoid haemorrhage, transient ischaemic attack, unconsciousness, vertigo, visual disturbance, vomiting, or weakness, as well as “no problem identified” or “unknown problem”. NSW Ambulance PHCR and eMR records include information on vital status (blood pressure, Glasgow Coma Scale score), management protocols applied,8,9 and treatment administered by paramedics. Protocols explored in this study were basic pre‐hospital care, cardiac arrest care, and stroke care; treatments included were oxygen therapy and ventilation.
According to the NSW Ambulance stroke care protocol, all patients with FAST warning signs (facial drooping, arm weakness, speech difficulties) should be transported to the highest level stroke care facility available within 90 minutes. During transport, paramedics regularly repeat and document physical examinations and physiological observations to identify trends, clinical deterioration, and response to treatment. Associated conditions (eg, hypo‐ or hyperglycaemia, altered level of consciousness) are treated as required. For people who meet hyperacute stroke treatment (eg, thrombolysis) criteria, paramedics complete a stroke process sheet, proceed to the hospital without delay, and notify the receiving hospital via the control centre. The minor variations to the protocol during 2005–2018 are summarised in Supporting Information, table 2.
Statistical analysis
We summarise patients’ demographic characteristics at hospitalisation as descriptive statistics, by sex. We summarise the assessments, applied protocols, and treatments during ambulance transport as descriptive statistics, by sex. We compared values for men and women as adjusted mean differences, or as adjusted odds ratios (aORs) with 95% confidence intervals (CIs) estimated in logistic regression models adjusted for age, marital status, country of birth, Indigenous status, hospital region, year of stroke onset, and stroke subtype. We also undertook a priori subgroup analyses by age group (under 70 years, 70 years or older), including an age*sex interaction term. Statistical analyses were conducted in SAS 9.4.
Ethics approval
This study was approved by the research ethics committees of NSW Population and Health Services (HREC/18/CIPHS/56), the Aboriginal Health and Medical Research Council of NSW (1503/19), and the Australian Institute of Health and Welfare (EO2018/2/431).
Results
Of 202 231 people hospitalised with a stroke diagnosis (mean age, 73 years; standard deviation [SD], 14 years; 98 599 women [51.0%]; 140 028 born in Australia [69.4%]), 101 357 were conveyed to hospital by ambulance (50.1%). The mean age of the women (75 years; SD, 14.7 years) was marginally higher than for men (71 years; SD, 13.7 years); other demographic and clinical differences were also small (Supporting Information, table 3).
Characteristics of patients who arrived by ambulance
A larger proportion of women than of men arrived at hospital by ambulance (52.4% v 47.9%; OR, 1.09; 95% CI, 1.07–1.11). A smaller proportion of women than of men who arrived by ambulance were aged 40–69 years (21.2% v 32.7%; aOR, 0.70; 95% CI, 0.64–0.76), but the proportion of women who arrived by ambulance aged 70 or more years was larger (76.9% v 65.2%; aOR, 1.29; 95% CI, 1.16–1.38) (Box 1). Mean systolic blood pressure (ambulance measures) was similar for women and men (adjusted: 149.0 mmHg; 95% CI, 147.4–150.6 mmHg v 146.8 mmHg; 95% CI, 145.2–148.4 mmHg), as were mean Glasgow Coma Scale scores (adjusted: 12.9; 95% CI, 12.7–13.0 v 13.2; 95% CI, 13.0–13.3) (Box 2). For patients with ambulance eMRs, time between the emergency call and emergency department admission was also similar for both sexes (Supporting Information, table 4).
Assessments of patients by ambulance paramedics
Socio‐demographic characteristics (including age and sex) and stroke subtype were similar for patients with eMR or PHCR records (Supporting Information, table 5). Paramedic assessment data were available for the 43 308 patients with ambulance eMRs (42.7% of those transported by ambulance). The likelihood of being assessed as having a stroke (aOR, 0.97; 95% CI, 0.93–1.01) or subarachnoid haemorrhage (aOR, 1.22; 95% CI, 0.73–2.03) was similar for women and men. Women were more likely than men to be assessed as having migraine (aOR, 3.61; 95% CI, 2.18–6.00), anxiety (aOR, 2.94; 95% CI, 2.06–4.20), unconsciousness (aOR, 1.48; 95% CI, 1.20–1.82), hypertension (aOR, 1.44; 95% CI, 1.23–1.69), nausea (aOR, 1.39; 95% CI, 1.08–1.78), or headache (aOR, 1.32; 95% CI, 1.17–1.49). Women were less likely than men to be assessed as having a transient ischaemic attack (aOR, 0.89; 95% CI, 0.83–0.96), dizziness (aOR, 0.80; 95% CI, 0.71–0.90), visual disturbance (aOR, 0.72; 95% CI, 0.58–0.92), acute coronary syndrome (aOR, 0.68; 95% CI, 0.53–0.89), a mobility problem (aOR, 0.60; 95% CI, 0.49–0.75), or hypotension (aOR, 0.60; 95% CI, 0.42–0.87) (Box 3).
Among patients under 70 years of age, women were less likely than men to be assessed as having a stroke (aOR, 0.89, 95% CI, 0.82–0.97); among those aged 70 years or more, women were more likely than men to be assessed as having hypertension (aOR, 1.86; 95% CI, 1.52–2.29) and less likely to be assessed as having dizziness (aOR, 0.74; 95% CI, 0.64–0.85). The likelihood of no problem being identified was not significantly different for women and men in either age group (Box 4).
Protocols applied and treatment administered by ambulance paramedics
Women were less likely than men to be managed according to the pre‐hospital stroke care protocol (aOR, 0.95; 95% CI, 0.92–0.97), but basic pre‐hospital care was similar for both sexes (aOR, 1.01; 95% CI, 0.99–1.04), as was the use of oxygen and ventilation (Box 5).
Discussion
Our large population‐based study, an analysis of data for people admitted to NSW hospitals with stroke during 2005–2018, examined sex differences in their management by emergency medical (ambulance) services. We found that women were more likely than men to arrive at hospital by ambulance, but less likely to receive stroke care management prior to hospital admission. Among patients under 70 years of age, women were less likely than men to be assessed by paramedics as having a stroke, but there was no significant difference for older patients.
About half of all patients admitted to hospital with stroke were transported by ambulance, and the proportion was larger for women (52.4% v 47.9%). Previous studies (Supporting Information, table 1) have found that the proportion of cases in which emergency medical services were activated for people with stroke ranged from 17% in Brazil10 to 82% in the United Kingdom.3 Sex differences in emergency medical service care have been reported for people with many illnesses and injuries,11,12 including stroke,3,4,5 but the conclusions drawn have been inconsistent, indicating the need for large population‐based studies to identify the reasons for these differences.
Among patients under 70 years of age, women later diagnosed with stroke were less likely than men to be assessed by paramedics as having stroke. Stroke is more frequently missed in women than in men; atypical clinical manifestations are more frequent in women, and implicit bias in evaluations by health care providers is also possible.6,13 We found that women subsequently diagnosed with stroke were more frequently assessed by paramedics as having stroke mimics (eg, headache or migraine, anxiety, unconsciousness) than men, contributing to delayed recognition and treatment of stroke, consistent with the findings of other studies.14,15,16,17
We found that the stroke care protocol was less likely to be invoked during ambulance transport for women than for men. Although the absolute difference was small (women, 49.5%; men, 51.4%), in‐hospital treatment may be delayed for a considerable number of women. Further, delayed initiation of effective treatment, such as reperfusion therapy,18 could have greater consequences for women because stroke outcomes are generally poorer for women than men,19 although women derive at least equivalent benefit from appropriate treatment.20 Awareness of these differences could have both clinical and financial consequences, given the costs of death and disability, including those of long term care.21 Similar sex‐related differences have been reported for myocardial infarction,22 and emergency department doctors are less likely to identify coronary artery disease as a cause of chest pain in women or to recommend diagnostic tests.23 Women are also less likely to report that their health care providers told them they were at risk for heart disease prior to an index myocardial infarction event, despite risk factor burdens similar to those of men.24
Limitations
The strength of our study was its whole‐of‐population analysis, permitting the generation of a comprehensive profile of pre‐hospital emergency medical service care for patients subsequently admitted with stroke. However, a range of stroke mimics were diagnosed by ambulance paramedics. While recognising the possible inaccuracy of specific ambulance reporting diagnoses, our intent was to present a descriptive profile and to assess differences in presentation times for people with stroke mimics. We could not link pre‐hospital care data with differences in mortality or morbidity data by sex. We could not assess symptoms presented by patients, reasons for the management chosen by paramedics, or management prior to the arrival of paramedics. Further, we had no data on potential confounders in the relationship between sex and emergency medical service management, such as risk factors for cardiovascular disease (eg, smoking, physical activity, body mass index, alcohol consumption), neurological severity at the time of the stroke, pre‐morbid dependence, and cardiovascular and cerebrovascular disease history. As information for 57% of people was documented only by PHCR, paramedic assessment, care protocol, and treatment information were missing for these patients, possibly causing selection bias.
Conclusion
Pre‐hospital emergency medical service care in NSW differs for women and men subsequently admitted to hospital with stroke. In particular, women are less likely to be managed with stroke‐specific protocols during ambulance transport to hospital. Paramedics should re‐consider their assessment of women during pre‐hospital emergency medical service care. Improving paramedic training in symptom recognition, particularly in women, may reduce time to treatment and improve outcomes for people with stroke.
Box 1 – Baseline characteristics by sex and arrivals by ambulance for patients admitted to New South Wales hospitals with a principal diagnosis of stroke, 2005–2018
|
Characteristics |
Did not arrive by ambulance |
Arrived by ambulance |
|
||||||||||||
|
Total |
Women |
Men |
Total |
Women |
Men |
OR (95% CI)* |
|||||||||
|
|
|||||||||||||||
|
All patients |
100 874 |
46 907 |
53 967 |
101 357 |
51 692 |
49 665 |
1.09 (1.07–1.11) |
||||||||
|
Age (years), mean (SD) |
70.4 (14.3) |
71.6 (15.0) |
69.3 (13.6) |
75 (14) |
78 (13.9) |
73 (13.6) |
|
||||||||
|
0–39 |
3392 (3.4%) |
1775 (3.8%) |
1617 (3.0%) |
2041 (2.0%) |
1004 (1.9%) |
1037 (2.1%) |
0.88 (0.79–0.98) |
||||||||
|
40–69 |
39 467 (39.1%) |
16 286 (34.7%) |
23 181 (43.0%) |
27 169 (26.8%) |
10 945 (21.2%) |
16 224 (32.7%) |
0.96 (0.93–0.99) |
||||||||
|
70 or more |
58 015 (57.5%) |
28 846 (61.5%) |
29 169 (54.1%) |
72 146 (71.2%) |
39 743 (76.9%) |
32 403 (65.2%) |
1.24 (1.21–1.27) |
||||||||
|
Country of birth |
|
|
|
|
|
|
|
||||||||
|
Australia |
70 350 (69.8%) |
33 409 (71.3%) |
36 941 (68.5%) |
69 678 (68.9%) |
36 390 (70.5%) |
33 288 (67.2%) |
1.18 (1.14–1.22) |
||||||||
|
Elsewhere |
30 383 (30.2%) |
13 436 (13.3%) |
16 947 (31.5%) |
31 487 (31.1%) |
15 205 (29.5%) |
16 282 (32.8%) |
1.21 (1.18–1.23) |
||||||||
|
Marital status |
|
|
|
|
|
|
|
||||||||
|
With partner |
57 977 (57.5%) |
20 893 (44.5%) |
37 084 (68.7%) |
50 277 (49.6%) |
18 492 (35.8%) |
31 785 (64.0%) |
1.03 (1.01–1.06) |
||||||||
|
Without partner |
40 334 (40.0%) |
24 747 (52.8%) |
15 587 (28.9%) |
49 088 (48.4%) |
32 184 (62.3%) |
16 904 (34.0%) |
1.20 (1.17–1.23) |
||||||||
|
Unknown |
2563 (2.5%) |
1267 (2.7%) |
1296 (2.4%) |
1992 (2.0%) |
1016 (2.0%) |
976 (2.0%) |
1.07 (0.95–1.20) |
||||||||
|
Indigenous status |
|
|
|
|
|
|
|
||||||||
|
Aboriginal or Torres Strait Islander |
1549 (1.5%) |
835 (1.8%) |
714 (1.3%) |
1547 (1.5%) |
774 (1.5%) |
773 (1.6%) |
0.86 (0.74–0.99) |
||||||||
|
Non‐Indigenous |
98 493 (97.7%) |
45 706 (97.5%) |
52 787 (97.9%) |
98 930 (97.6%) |
50 464 (97.7%) |
48 466 (97.6%) |
1.20 (1.18–1.22) |
||||||||
|
Did not respond |
788 (0.8%) |
343 (0.7%) |
445 (0.8%) |
853 (0.8%) |
433 (0.8%) |
420 (0.9%) |
1.34 (1.10–1.63) |
||||||||
|
Region |
|
|
|
|
|
|
|
||||||||
|
Urban |
68 472 (69.6%) |
32 138 (70.2%) |
36 334 (69.2%) |
70 550 (71.1%) |
36 366 (71.7%) |
34 184 (70.6%) |
1.20 (1.18–1.23) |
||||||||
|
Regional |
29341 (29.8%) |
215 (0.5%) |
288 (0.6%) |
28310 (28.6%) |
14234 (28.1%) |
14076 (29.1%) |
1.20 (1.16–1.24) |
||||||||
|
Remote |
503 (0.5%) |
13 436 (29.3%) |
15 905 (30.3%) |
305 (0.3%) |
143 (0.3%) |
162 (0.3%) |
1.19 (0.89–1.57) |
||||||||
|
Stroke subtype |
|
|
|
|
|
|
|
||||||||
|
Ischaemic stroke |
23 885 (23.7%) |
10 395 (22.2%) |
13 490 (25.0%) |
38 782 (38.3%) |
18 775 (36.3%) |
20 007 (40.3%) |
1.22 (1.18–1.26) |
||||||||
|
Intracerebral haemorrhage |
4653 (4.6%) |
2078 (4.4%) |
2575 (4.8%) |
10 981 (10.8%) |
5528 (10.7%) |
5453 (11.0%) |
1.26 (1.17–1.35) |
||||||||
|
Subarachnoid haemorrhage |
2141 (2.1%) |
1226 (2.6%) |
915 (1.7%) |
4343 (4.3%) |
2718 (5.3%) |
1625 (3.3%) |
1.25 (1.12–1.39) |
||||||||
|
Transient ischaemic stroke |
42 232 (41.9%) |
21 018 (44.8%) |
21 214 (39.3%) |
28 126 (27.8%) |
14718 (28.5%) |
13 408 (27.0%) |
1.11 (1.08–1.14) |
||||||||
|
Occlusion and stenosis of prevertebral arteries |
16 403 (16.3%) |
6661 (14.2%) |
9742 (18.1%) |
2503 (4.8%) |
2578 (5.2%) |
5081 (5.0%) |
1.42 (1.33–1.51) |
||||||||
|
Not determined |
11 560 (11.5%) |
5529 (11.8%) |
6031 (11.2%) |
14 044 (13.9%) |
7450 (14.4%) |
6594 (13.3%) |
1.23 (1.17–1.30) |
||||||||
|
|
|||||||||||||||
|
* Proportion transported to hospital by ambulance: women v men. |
|||||||||||||||
Box 2 – Emergency medical service clinical measures for patients subsequently admitted to NSW hospitals with principal diagnosis of stroke, 2005–2018*
|
Clinical measure* |
Univariable analysis |
Multivariable analysis† |
|||||||||||||
|
Women |
Men |
Mean difference (95% CI) |
Women |
Men |
Adjusted mean difference |
||||||||||
|
|
|||||||||||||||
|
All patients |
51 692 |
49 665 |
|
|
|
|
|||||||||
|
Systolic blood pressure (mmHg), mean (95% CI) |
152.7 (152.4–152.9) |
149.6 (149.3–149.9) |
3.05 (2.66–3.45) |
149.0 (147.4–150.6) |
146.8 (145.2–148.4) |
2.23 (1.83–2.63) |
|||||||||
|
Number of patients |
47 125 |
45 698 |
|
|
|
|
|||||||||
|
Diastolic blood pressure (mmHg), mean (95% CI) |
82.6 (82.3–82.8) |
83.1 (82.9–83.3) |
–0.55 (–0.86 to –0.24) |
82.1 (80.8–83.3) |
82.0 (80.8–83.3) |
0.05 (–0.27 to 0.37) |
|||||||||
|
Number of patients |
37 281 |
36 420 |
|
|
|
|
|||||||||
|
Glasgow Coma Scale, mean score (95% CI) |
13.5 (13.5–13.5) |
13.9 (13.9–13.9) |
–0.39 (–0.42 to –0.35) |
12.9 (12.7–13.0) |
13.2 (13.0–13.3) |
–0.30 (–0.33 to –0.27) |
|||||||||
|
Glasgow Coma Scale, median score (IQR) |
15 (14–15) |
15 (14–15) |
— |
— |
— |
— |
|||||||||
|
Number of patients |
47 105 |
45 402 |
|
|
|
|
|||||||||
|
|
|||||||||||||||
|
CI = confidence interval; IQR = interquartile range. * For patients with ambulance electronic medical records or paper‐based patient health care records. † Adjusted for age (continuous), marital status, country of birth, Indigenous status, hospital region, year of stroke onset, and stroke subtype. |
|||||||||||||||
Box 3 – Final emergency medical service (ambulance) assessments of people subsequently admitted to NSW hospitals with principal diagnosis of stroke, 2005–2018: adjusted multivariable analyses (patients with ambulance electronic medical records only)*
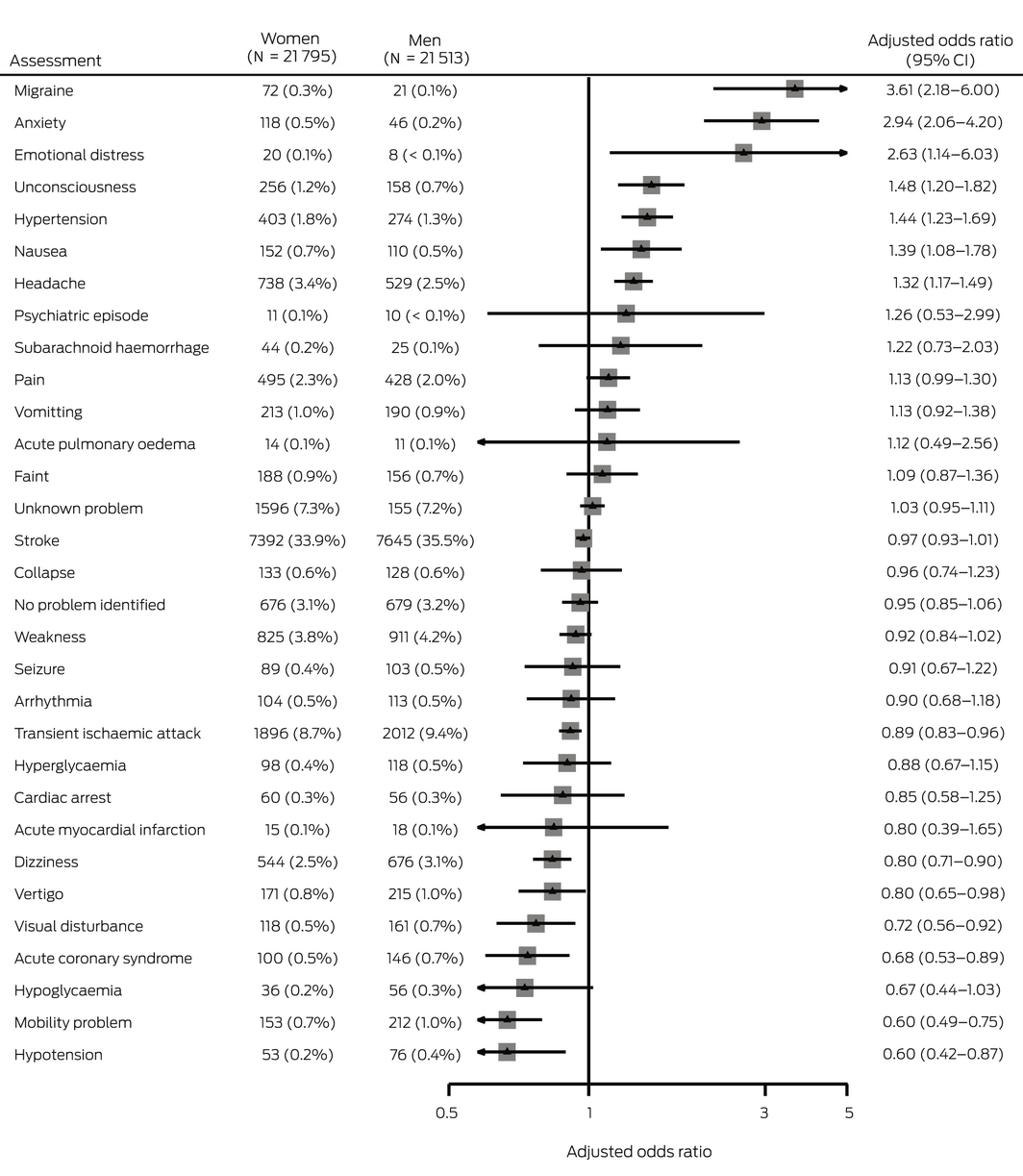
CI = confidence interval. * Adjusted for age (continuous), marital status, country of birth, Indigenous status, hospital region, year of stroke onset, and stroke subtype. Univariable analyses are included in the Supporting Information, table 6.
Box 4 – Final emergency medical service (ambulance) assessments of people subsequently admitted to NSW hospitals with principal diagnosis of stroke, 2005–2018: adjusted multivariable analyses (patients with ambulance electronic medical records only), by age group*
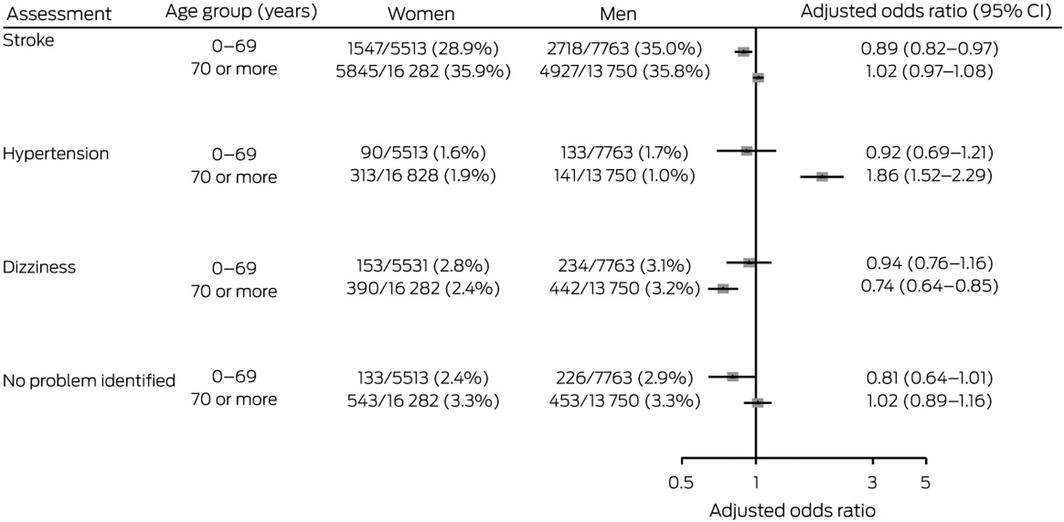
CI = confidence interval. * Adjusted for age (continuous), marital status, country of birth, Indigenous status, hospital region, year of stroke onset, and stroke subtype.
Box 5 – Management protocols and treatments administered by emergency medical service for people subsequently admitted to NSW hospitals with principal diagnosis of stroke, 2005–2018: adjusted multivariable analyses (all patients)*
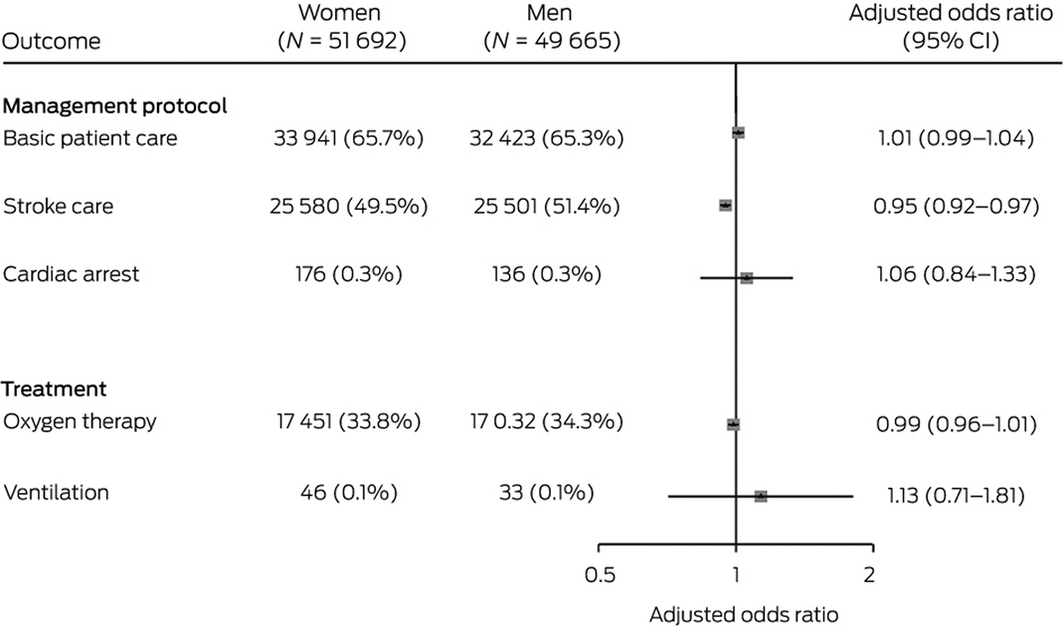
CI = confidence interval. * Adjusted for age (continuous), marital status, country of birth, Indigenous status, hospital region, year of stroke onset, and stroke subtype. Univariable analyses are included in the Supporting Information, table 7.
Received 1 July 2021, accepted 10 May 2022
- Xia Wang1
- Cheryl Carcel1
- Benjumin Hsu2
- Sultana Shajahan1
- Matthew Miller2
- Sanne Peters3
- Deborah A Randall2
- Alys Havard2
- Julie Redfern1,4
- Craig S Anderson1,5
- Louisa Jorm2
- Mark Woodward1
- 1 The George Institute for Global Health, University of New South Wales, Sydney, NSW
- 2 Centre for Big Data Research in Health, University of New South Wales, Sydney, NSW
- 3 The George Institute for Global Health, Oxford, United Kingdom
- 4 School of Health Sciences, Faculty of Medicine and Health, University of Sydney, NSW
- 5 Royal Prince Alfred Hospital, Sydney, NSW
Open access
Open access publishing facilitated by University of New South Wales, as part of the Wiley ‐ University of New South Wales agreement via the Council of Australian University Librarians.
This study was funded by a National Health and Medical Research Council (NHMRC) project grant (APP1147430). Xia Wang is supported by National Heart Foundation postdoctoral fellowship (102117), a New South Wales Health Commission investigator development grant, and an NHMRC Investigator grant (APP1195237). Cheryl Carcel is supported by a National Heart Foundation postdoctoral fellowship (102741), Julie Redfern by an NHMRC Career Development Fellowship (APP1143538), Alys Havard by an NSW Health Early‐Mid Career Fellowship, Craig Anderson by an NHMRC Investigator grant (APP1175861), and Mark Woodward by an NHMRC Investigator grant (APP1174120). We thank the staff at the Centre for Health Record Linkage, the NSW Admitted Patient Data Collection, and NSW Ambulance for their assistance with data linkage.
No relevant disclosures.
- 1. Emberson J, Lees KR, Lyden P, et al; Stroke Thrombolysis Trialists' Collaborative Group. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischemic stroke: a meta‐analysis of individual patient data from randomized trials. Lancet 2014; 384: 1929‐1935.
- 2. Saver JL, Goyal M, van der Lugt A, et al; HERMES Collaborators. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta‐analysis. JAMA 2016; 316: 1279‐1288.
- 3. Price CI, Rae V, Duckett J, et al. An observational study of patient characteristics associated with the mode of admission to acute stroke services in North East, England. PLoS One 2013; 8: e76997.
- 4. Reeves MJ, Fonarow GC, Zhao X, et al; Get With The Guidelines‐Stroke Steering Committee and Investigators. Quality of care in women with ischemic stroke in the GWTG program. Stroke 2009; 40: 1127‐1133.
- 5. Park SJ, Shin SD, Ro YS, et al. Gender differences in emergency stroke care and hospital outcome in acute ischemic stroke: a multicenter observational study. Am J Emerg Med 2013; 31: 178‐184.
- 6. Yu AYX, Penn AM, Lesperance ML, et al; SpecTRA Study Group. Sex differences in presentation and outcome after an acute transient or minor neurologic event. JAMA Neurol 2019; 76: 962‐968.
- 7. Newman‐Toker DE, Moy E, Valente E, et al. Missed diagnosis of stroke in the emergency department: a cross‐sectional analysis of a large population‐based sample. Diagnosis 2014; 1: 155‐166.
- 8. New South Wales Ambulance. NSW Ambulance protocols 2016, version 2.0.5. Updated 2 Sept 2021. https://apps.apple.com/au/app/nsw‐ambulance‐protocols/id1103576564 (viewed Oct 2021).
- 9. Ambulance Service of New South Wales. Protocols and pharmacology: 2014 amendment. Updated Jan 2014. http://www.australianparamedicalcollege.com.au/learning‐material/general‐information/ASNSW‐protocols‐pharmacology‐2014.pdf (viewed Oct 2021).
- 10. Kuster GW, Bueno Alves M, Cendoroglo Neto M, Silva GS. Determinants of emergency medical services use in a Brazilian population with acute ischemic stroke. J Stroke Cerebrovasc Dis 2013; 22: 244‐249.
- 11. Weiss SJ, Ernst AA, Phillips J, Hill B. Gender differences in state‐wide EMS transports. Am J Emerg Med 2000; 18: 666‐670.
- 12. Canto JG, Zalenski RJ, Ornato JP, et al; National Registry of Myocardial Infarction 2 Investigators. Use of emergency medical services in acute myocardial infarction and subsequent quality of care: observations from the National Registry of Myocardial Infarction 2. Circulation 2002; 106: 3018‐3023.
- 13. Tarnutzer AA, Lee SH, Robinson KA, et al. ED misdiagnosis of cerebrovascular events in the era of modern neuroimaging: a meta‐analysis. Neurology 2017; 88: 1468‐1477.
- 14. Gall SL, Donnan G, Dewey HM, et al Sex differences in presentation, severity, and management of stroke in a population‐based study. Neurology. 2010; 74: 975‐981.
- 15. Kropp P, Holzhausen M, Kolodny E, et al; Stroke in Young Fabry Patients (sifap) Investigators. Headache as a symptom at stroke onset in 4431 young ischaemic stroke patients. Results from the “Stroke in Young Fabry Patients (SIFAP1) study”. J Neural Transm 2013; 120: 1433‐1440.
- 16. Venkat A, Cappelen‐Smith C, Askar S, et al. Factors associated with stroke misdiagnosis in the emergency department: a retrospective case‐control study. Neuroepidemiology 2018; 51: 123‐127.
- 17. Zrelak PA. Sex‐based differences in symptom perception and care‐seeking behavior in acute stroke. Perm J 2018; 22: 18‐042.
- 18. Mainz J, Andersen G, Valentin JB, et al. Disentangling sex differences in use of reperfusion therapy in patients with acute ischemic stroke. Stroke 2020; 51: 2332‐2338.
- 19. Carcel C, Wang X, Sandset EC, et al. Sex differences in treatment and outcome after stroke: pooled analysis including 19 000 participants. Neurology 2019; 93: e2170‐e2180.
- 20. Bushnell C, Howard VJ, Lisabeth L, et al. Sex differences in the evaluation and treatment of acute ischaemic stroke. Lancet Neurol 2018; 17: 641‐650.
- 21. Synhaeve NE, Arntz RM, Maaijwee NAM, et al. Poor long‐term functional outcome after stroke among adults aged 18 to 50 years: follow‐up of transient ischemic attack and stroke patients and unelucidated risk factor evaluation (FUTURE) study. Stroke 2014; 45: 1157‐1160.
- 22. Hsu B, Carcel C, Wang X, et al. Sex differences in emergency medical services management of patients with myocardial infarction: analysis of routinely collected data for over 110 000 patients. Am Heart J 2021; 241: 87‐91.
- 23. Golden KE, Chang AM, Hollander JE. Sex preferences in cardiovascular testing: the contribution of the patient–physician discussion. Acad Emerg Med 2013; 20: 680‐688.
- 24. Leifheit‐Limson EC, D’Onofrio G, Daneshvar M, et al. Sex differences in cardiac risk factors, perceived risk, and health care provider discussion of risk and risk modification among young patients with acute myocardial infarction: the VIRGO Study. J Am Coll Cardiol 2015; 66: 1949‐1957.






Abstract
Objectives: To examine whether pre‐hospital emergency medical service care differs for women and men subsequently admitted to hospital with stroke.
Design, setting, participants: Population‐based cohort study; analysis of linked Admitted Patient Data Collection and NSW Ambulance data for people admitted to New South Wales hospitals with a principal diagnosis of stroke at separation, 1 July 2005 – 31 December 2018.
Main outcome measures: Emergency medical service assessments, protocols, and management for patients subsequently diagnosed with stroke, by sex.
Results: Of 202 231 people hospitalised with stroke (mean age, 73 [SD, 14] years; 98 599 women [51.0%]), 101 357 were conveyed to hospital by ambulance (50.1%). A larger proportion of women than men travelled by ambulance (52.4%v 47.9%; odds ratio [OR], 1.09; 95% CI, 1.07–1.11), but time between the emergency call and emergency department admission was similar for both sexes. The likelihood of being assessed as having a stroke (adjusted OR [aOR], 0.97; 95% CI, 0.93–1.01) or subarachnoid haemorrhage (aOR, 1.22; 95% CI, 0.73–2.03) was similar for women and men, but women under 70 years of age were less likely than men to be assessed as having a stroke (aOR, 0.89; 95% CI, 0.82–0.97). Women were more likely than men to be assessed by paramedics as having migraine, other headache, anxiety, unconsciousness, hypertension, or nausea. Women were less likely than men to be managed according to the NSW Ambulance pre‐hospital stroke care protocol (aOR, 0.95; 95% CI, 0.92–0.97), but the likelihood of basic pre‐hospital care was similar for both sexes (aOR, 1.01; 95% CI, 0.99–1.04).
Conclusion: Our large population‐based study identified sex differences in pre‐hospital management by emergency medical services of women and men admitted to hospital with stroke. Paramedics should receive training that improves the recognition of stroke symptoms in women.