Patients with single high sensitivity cardiac troponin I (hs‐cTnI) measurements below specified threshold values are deemed to be at low risk of acute myocardial infarction (AMI).1,2,3,4,5 The accuracy of single hs‐cTnI measurements has not been investigated in Aboriginal and Torres Strait Islander people. The National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand guidelines note that Aboriginal and Torres Strait Islander patients should generally not be treated as being at low risk.6
We evaluated the accuracy of single hs‐cTnI measurements for excluding AMI in Aboriginals and Torres Strait Islanders in a planned analysis of data collected during the observational IMPACT study, which examined the assessment of potential acute coronary syndrome (ACS) in this population. We collected data for adults (18 years or older) who visited the Cairns Hospital emergency department during the 2019 calendar year and were evaluated for ACS. Patients were recruited consecutively on weekdays (8 am – 5 pm). Further details, including on cultural safety, are included in the . The Far North Queensland Human Research Ethics Committee approved the study (HREC/17/QCH/42–1139).
All participants received standard care, including electrocardiography and hs‐cTnI assessments at presentation and 2–3 hours later (hs‐cTn I assay [Beckman Coulter]; limit of detection, 2.3 ng/L), as well as appropriate imaging for coronary artery disease. Thirty days later, research nurses followed up patients by telephone and reviewed medical records for cardiac events, cardiac investigations, and contact with health care providers. The primary endpoint was index type 1 myocardial infarction (T1MI), including non‐ST‐elevation myocardial infarction (NSTEMI), or cardiac death prior to discharge. Secondary outcomes were index AMI (types 1 and 2 MI), and 30‐day major adverse cardiac events (MACE: T1MI, revascularisation, cardiovascular death within 30 days of presentation). Test sensitivity and negative predictive value (NPV) were calculated with exact binomial 95% confidence intervals (CIs), for each hs‐cTnI value below the 99th percentile (18 ng/L).
A total of 110 Aboriginal and Torres Strait Islander people were included in our study (); 58 were men (53%). Fifteen people (14%) had hs‐cTnI values of 2 ng/L or less, none of whom reached the primary or secondary endpoints. Test sensitivity was 100% (95% CI, 93–100%) and the NPV 100% (95% CI, 78–100%) (Box 1). Sensitivity and NPV were also 100% with the cTnI cut‐off recommended by the European Society for Cardiology (4 ng/L);8 this cut‐off excluded AMI for 30 people (27%), none of whom reached the primary or secondary endpoints. Diagnostic accuracy was similar for patients who presented to the emergency department and those who had been transferred from other facilities (data not shown).
Our findings support using single low level hs‐cTnI values to exclude AMI in Aboriginal and Torres Strait Islander people; applying either presentation cut‐off value (2 or 4 ng/L) enabled early exclusion without missing any cases of AMI or MACE. Large proportions of participants reported risk factors for cardiovascular disease, including smoking (66%), diabetes (48%), hypertension (56%), and family history of coronary artery disease (57%) (Box 2). A low hs‐cTnI value may safely exclude AMI, but Aboriginal and Torres Strait Islander people may benefit from referral to culturally appropriate medical services for cardiac risk factor management.
Our study was limited by the small sample size and its restriction to a single centre. Despite 100% sensitivity and NPV, the lower bounds of the 95% CIs with a 2 ng/L cut‐off indicated a considerable degree of uncertainty. Exclusion algorithms should be implemented in the context of the individual’s clinical history. It is unclear how doing so would have affected diagnostic accuracy.
A single low level hs‐cTnI value can be used for early rule‐out of AMI in Aboriginal and Torres Strait Islander patients. Our study advances understanding of ACS assessment by ensuring that our evidence base reflects the diversity of people in our health care system.
Box 1 – Receiver operating characteristic curve for using single low level high sensitivity cardiac troponin I values in the emergency department to exclude acute myocardial infarction in Aboriginal and Torres Strait Islander people
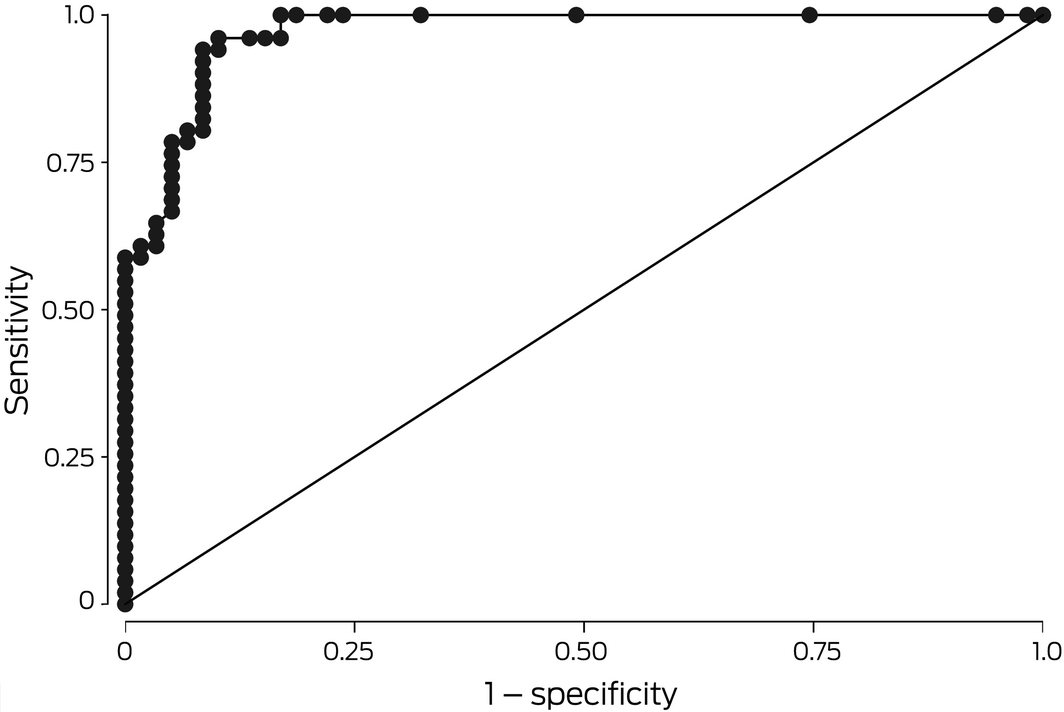
Area under the receiver operating characteristic curve = 0.9699.
Box 2 – Characteristics of 110 Aboriginal and Torres Strait Islander people who were evaluated for acute coronary syndrome in the Cairns Hospital emergency department during 2019
|
Characteristic |
|
||||||||||||||
|
|
|||||||||||||||
|
Indigenous status |
|
||||||||||||||
|
Aboriginal |
91 (83%) |
||||||||||||||
|
Torres Strait Islander |
15 (14%) |
||||||||||||||
|
Aboriginal and Torres Strait Islander |
4 (4%) |
||||||||||||||
|
Age (years), mean (SD) |
50.5 (10.9) |
||||||||||||||
|
People who experienced index acute myocardial infarction |
54.6 (8.8) |
||||||||||||||
|
People who did not experience index acute myocardial infarction |
46.4 (11.2) |
||||||||||||||
|
Sex (men) |
58 (53%) |
||||||||||||||
|
Time from symptom onset to presentation (hours), median (IQR) |
5.7 (2.5–12.1) |
||||||||||||||
|
Presentation within one hour of symptom onset |
8 (7%) |
||||||||||||||
|
Time from presentation to first troponin test (hours), median (IQR) |
0.4 (0.3–0.8) |
||||||||||||||
|
Transfers from other facilities |
47 (43%) |
||||||||||||||
|
Cardiovascular risk factors |
|
||||||||||||||
|
Hypertension |
62 (56%) |
||||||||||||||
|
Dyslipidaemia |
50 (46%) |
||||||||||||||
|
Diabetes |
53 (48%) |
||||||||||||||
|
Family history of coronary artery disease |
63 (57%) |
||||||||||||||
|
Current or recent smoking |
72 (66%) |
||||||||||||||
|
Cardiovascular history |
|
||||||||||||||
|
Previous myocardial infarction |
31 (28%) |
||||||||||||||
|
Previous angina |
22 (20%) |
||||||||||||||
|
Previous coronary artery bypass graft |
10 (9.1%) |
||||||||||||||
|
Previous angioplasty |
17 (16%) |
||||||||||||||
|
Previous stroke or transient ischaemic attack |
3 (3%) |
||||||||||||||
|
Previous congestive heart failure |
6 (6%) |
||||||||||||||
|
Index acute myocardial infarctions |
52 (47%) |
||||||||||||||
|
Type 1 during index presentation |
50 (46%) |
||||||||||||||
|
Type 2 during index presentation |
2 (2%) |
||||||||||||||
|
Angiography within 30 days |
68 (62%) |
||||||||||||||
|
Emergency or urgent revascularisation during index presentation |
47 (43%) |
||||||||||||||
|
Outcomes by 30 days |
|
||||||||||||||
|
Died |
1 (1%) |
||||||||||||||
|
Type 1 myocardial infarction |
51 (46%) |
||||||||||||||
|
Type 2 myocardial infarction |
2 (2%) |
||||||||||||||
|
Emergency revascularisation |
10 (9.1%) |
||||||||||||||
|
Major adverse cardiac events |
56 (51%) |
||||||||||||||
|
|
|||||||||||||||
|
IQR = interquartile range; SD = standard deviation. |
|||||||||||||||
Received 29 November 2021, accepted 19 April 2022
- 1. Body R, Mueller C, Giannitsis E, et al; TRAPID‐AMI Investigators. The use of very low concentrations of high‐sensitivity troponin T to rule out acute myocardial infarction using a single blood test. Acad Emerg Med 2016; 23: 1004‐1013.
- 2. Pickering JW, Than M, Cullen L, et al. Rapid rule‐out of acute myocardial infarction with a single high‐sensitivity cardiac troponin T measurement below the limit of detection: a collaborative meta‐analysis. Ann Intern Med 2017; 166: 715‐724.
- 3. Sandoval Y, Smith SW, Love SA, et al. Single high‐sensitivity cardiac troponin I to rule out acute myocardial infarction. Am J Med 2017; 130: 1076‐1083.
- 4. Greenslade JH, Cho E, Van Hise C, et al. Evaluating rapid rule‐out of acute myocardial infarction using a high‐sensitivity cardiac troponin I assay at presentation. Clin Chem 2018; 64: 820‐829.
- 5. Chapman AR, Lee KK, McAllister DA, et al. Association of high‐sensitivity cardiac troponin I concentration with cardiac outcomes in patients with suspected acute coronary syndrome. JAMA 2017; 318: 1913‐1924.
- 6. Chew DP, Scott IA, Cullen L, et al; NHFA/CSANZ ACS Guideline 2016 Executive Working Group. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: Australian clinical guidelines for the management of acute coronary syndromes 2016. Heart Lung Circ 2016; 25: 895‐951.
- 7. Cullen L, Stephensen L, Greenslade J, et al. Emergency department assessment of suspected acute coronary syndrome using the IMPACT pathway in Aboriginal and Torres Strait Islander people. Heart Lung Circ 2022; https://doi.org/10.1016/j.hlc.2022.02.010 [online ahead of print].
- 8. Roffi M, Patrono C, Collet JP, et al; ESC Scientific Document Group. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST‐segment elevation: Task Force for the management of Acute Coronary Syndromes in Patients Presenting without Persistent ST‐Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 2016; 37: 267‐315.





Jaimi Greenslade is supported by an Advance Queensland Fellowship. Funding for this investigation (data collection and study coordination, health economics analysis, community engagement activities) was provided by the Australian Centre for Health Services Innovation (AusHSI) and the Medical Research Future Fund (MRFF), administered by Brisbane Diamantina Health Partners.
Louise Ann Cullen has received institutional grants and consulting fees and honoraria from Beckman Coulter and Abbott Diagnostics. These grants were unrelated to the reported investigation.