Same‐day inguinal hernia repair was recognised as safe and cost‐effective 65 years ago.1 However, only 18 of 526 surgeons who billed Medibank during 2015–16 and 2016–17 for five or more repair procedures (3%) had discharged all their patients on the day of admission.2 As this rate did not reflect international guidelines, the Royal Australasian College of Surgeons (RACS) commissioned in 2017 a literature review with input from clinical experts, and recommended that 70–80% of inguinal hernia repairs in adults should be undertaken as same‐day procedures.3,4
We extracted hospitalisations (public and private) data from the Australian Institute of Health and Welfare principal diagnosis data cubes5 for patients with inguinal hernia as the principal diagnosis (International Classification of Diseases, 10th revision, code K40) during the period 1 July 2000 – 30 June 2019. We also compared changes in the proportions of same‐day procedures during 2004–05 to 2017–18 with changes in New Zealand and the United Kingdom (further details: Supporting Information, supplementary methods). Our study was granted exemption from formal ethics review by the University of Sydney Human Research Ethics Committee.
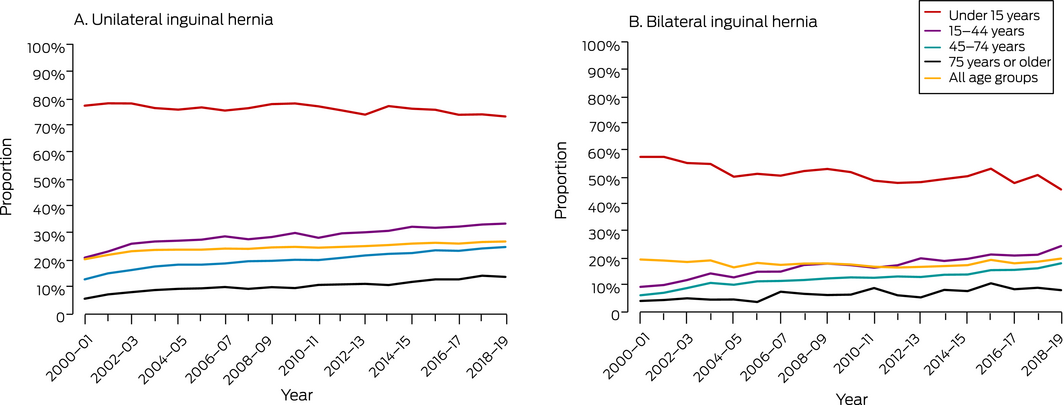
Of 875 111 hospitalisations for inguinal hernia repair (783 623 for male patients, 89.5%), 202 018 (23.1%; 95% confidence interval [CI], 23.0–23.2%) were same‐day procedures; the rates were higher for unilateral repairs (24.4%; 95% CI, 24.3–24.5%), female patients (28.6%; 95% CI, 28.3–28.9%), and patients under 15 years of age (69.5%; 95% CI, 69.2–69.9%) (Supporting Information, table 2). The overall same‐day inguinal hernia repair rate rose from 20.0% (95% CI, 19.6–20.3%) in 2000–01 to 25.1% (95% CI, 24.7–25.5%) in 2018–19; for unilateral repairs it increased from 20.1% (95% CI, 19.7–20.5%) to 26.7% (95% CI, 26.2–27.1%), but the rate was unchanged for bilateral repairs (2000–01: 19.2%; 95% CI, 18.2–20.2%; 2018–19: 19.6%; 95% CI, 18.8–20.3%). The rate declined with patient age, and exceeded 70% only for patients under 15 years of age who underwent unilateral repairs (Box 1).
The same‐day inguinal hernia repair rate rose from 22.4% (95% CI, 22.0–22.8%) in 2004–05 to 24.6% (95% CI, 24.2–25.0%) in 2017–18. By way of comparison, it increased in New Zealand from 42.7% (95% CI, 41.6–43.9%) to 46.5% (95% CI, 45.4–47.6%), and in the United Kingdom from 45.8% (95% CI, 45.5–46.2%) to 67.8% (95% CI, 67.5–68.2%). The mean rate for this period was substantially lower in Australia (23.3%; 95% CI, 23.2–23.4%) than in New Zealand (46.1%; 95% CI, 45.7–46.4%) or the United Kingdom (58.8%; 95% CI, 58.8–60.0%) (Box 2). In New Zealand, the same‐day rate was lower in private (41.8%; 95% CI, 41.2–42.3%) than in public hospitals (47.8%; 95% CI, 47.5–48.2%).
We found that 23.1% of inguinal hernia repair procedures in Australia during 2000–19 were same‐day procedures. The recent RACS 70–80% target3,4 was realised only for patients under 15 years of age who underwent unilateral repair. Same‐day rates were higher and have also risen in New Zealand and the United Kingdom, in contrast to the relatively stable, lower rate in Australia. The United Kingdom rise is partly explained by the fact that National Health Service hospitals have received £200–£250 (about $358–$447) for each same‐day inguinal hernia repair procedure since the 1990s.6 High rates in New Zealand suggest that barriers to same‐day procedures may be related more to variations in surgical practice than the health care setting (public or private hospital).
Inpatient stays for most people undergoing inguinal hernia repair in Australia may have several explanations. Patient‐reported outcomes following same‐day surgery are at least as good as those after overnight stays,3,7 but other factors may be barriers to routinely providing this option (Box 3).3,4,7 Increasing same‐day inguinal hernia repair rates will consequently involve a complex interplay of pre‐ and post‐operative decisions by hospitals, surgeons, and patients.
Box 1 – Same day inguinal hernia repair procedures as proportion of all procedures, Australia, 2000‒19, by laterality and age group
Box 2 – Same day procedures as proportion of all inguinal hernia repair procedures, Australia, New Zealand, and the United Kingdom, 2004‒18
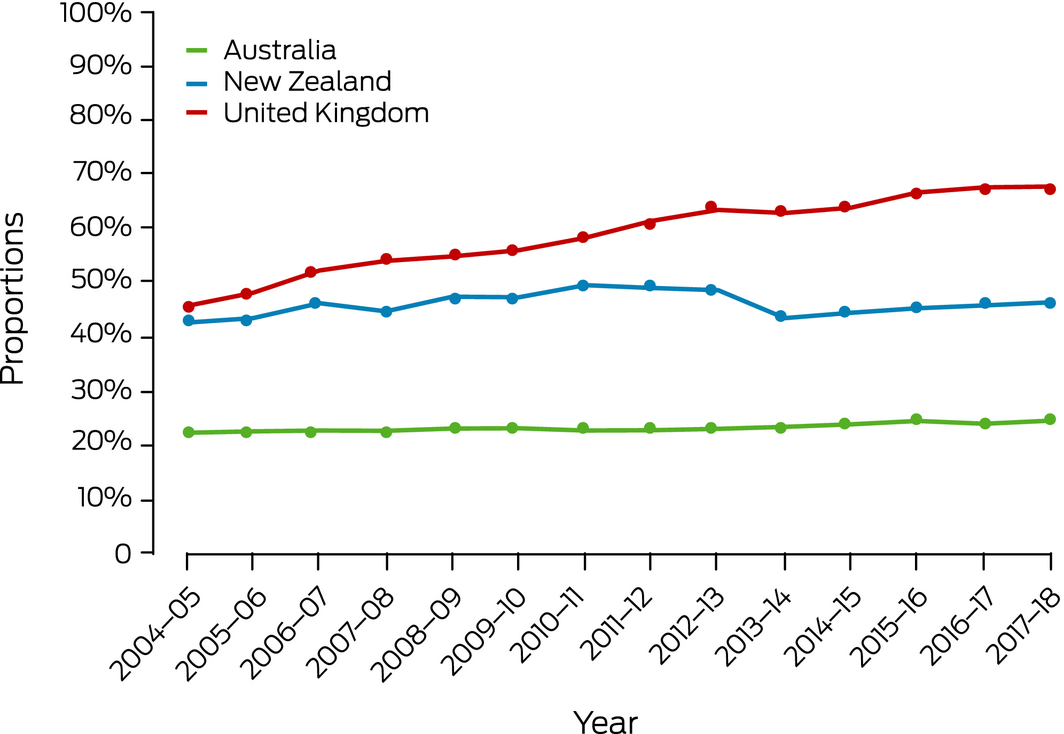
Sources: Australian Institute of Health and Welfare, New Zealand Government Ministry of Health, and United Kingdom National Health Service Digital Information (Supporting Information, supplementary methods).
Box 3 – Potential benefits of and perceived barriers to same‐day inguinal hernia repair procedures in Australia3,4,7
|
|
|||||||||||||||
|
Potential benefits |
|||||||||||||||
|
Out‐of‐pocket savings for patient |
|||||||||||||||
|
Lower risk of procedure cancellation because inpatient bed unavailable |
|||||||||||||||
|
Lower risk of hospital infections |
|||||||||||||||
|
Better patient‐rated outcomes |
|||||||||||||||
|
Better surgeon outcomes through standardised care |
|||||||||||||||
|
Improved patient flow and resource allocation |
|||||||||||||||
|
Reduced cost to health care system |
|||||||||||||||
|
Perceived barriers |
|||||||||||||||
|
Patient preference for overnight stay |
|||||||||||||||
|
Surgeon preference for overnight stay |
|||||||||||||||
|
Late scheduling on theatre lists |
|||||||||||||||
|
Distances between patient home and hospital |
|||||||||||||||
|
Inadequate outpatient or primary care support |
|||||||||||||||
|
Lack of adequate social support |
|||||||||||||||
|
Private hospital‐insurer financial arrangements |
|||||||||||||||
|
Lack of access to an appropriate day surgery facility |
|||||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Received 26 August 2021, accepted 3 December 2021
- 1. Farquharson EL. Early ambulation with special reference to herniorrhaphy as an outpatient procedure. Lancet 1955; 266: 517–519.
- 2. Royal Australasian College of Surgeons; Medibank. Surgical variance report 2017: general surgery. 2017. https://www.surgeons.org/‐/media/Project/RACS/surgeons‐org/files/reports‐guidelines‐publications/surgical‐variance‐reports/surgical‐variance‐report‐2017‐general‐surgery.pdf (viewed Dec 2021).
- 3. Royal Australasian College of Surgeons. Same‐day surgery for femoral, inguinal and umbilical hernia repair in adults. Final report. Feb 2017. https://www.surgeons.org/‐/media/Project/RACS/surgeons‐org/files/reports‐guidelines‐publications/surgical‐variance‐reports/2017‐04‐21_rpt_racs_mbp_hernia_repair.pdf (viewed Dec 2021).
- 4. Scarfe A, Duncan J, Ma N, et al. Day case hernia repair: weak evidence or practice gap? ANZ J Surg 2018; 88: 547–553.
- 5. Australian Institute of Health and Welfare. Principal diagnosis data cubes (Cat. no: WEB 216). Updated 7 Dec 2020. https://www.aihw.gov.au/reports/hospitals/principal‐diagnosis‐data‐cubes (viewed Mar 2021).
- 6. Skues M, Jackson I. Ten year performance of ambulatory surgery in England. Ambul Surg 2018; 24: 15–19.
- 7. Tam A, Phong J, Ma J, Strauss P. Inguinal hernia repair as day‐case surgery: a potentially underutilized practice. ANZ J Surg 2020; 90: 2159–2161.





This study formed part of Joanna Mills’ doctoral research at the Sydney Medical School, supported by a Research Training Program Scholarship provided by the Australian government. Thomas Hugh received project grant funding from the HCF Research Foundation. We acknowledge the Australian Institute of Health and Welfare for providing the hospital admissions data.
No relevant disclosures.