Children are facing a “generation‐defining disruption”1 from the coronavirus disease 2019 (COVID‐19) pandemic. To date, the direct health impacts of the severe acute respiratory coronavirus 2 itself have been relatively minimal for children globally, even with the Delta variant.2,3,4,5 In Australia, infections have been relatively low compared with other countries because of our strict public health restrictions (Box 1). However, these restrictions are having immediate and likely longer term adverse consequences on children’s developmental potential,11,12,13,14,15 with the impacts likely to be more severe if we do not consider the necessary policy responses as we emerge from the pandemic.1,16,17,18 While there are also positive impacts, such as population‐level resilience and rapid improvements in telehealth,19,20 our review focuses primarily on potential adverse impacts. There is likely to be a disproportionate impact on children experiencing adversity (eg, socio‐economic disadvantage),18,21 and potential for the widening of existing disparities in child health and developmental outcomes.3,17,22,23
To understand how Australia might best respond to the needs of children, a community child health (also known internationally as social paediatrics) lens offers a useful framing for the complex issues that need to be considered. Community child health takes into account the child, family, community and system factors (including social determinants). It has a specific focus on the intersectionality between health, education and social care for achieving equitable child health and developmental outcomes and preventive care.21,24,25 Community child health as a paediatric subspecialty within the Royal Australasian College of Physicians has three pillars: developmental–behavioural paediatrics, child protection, and child population health.26
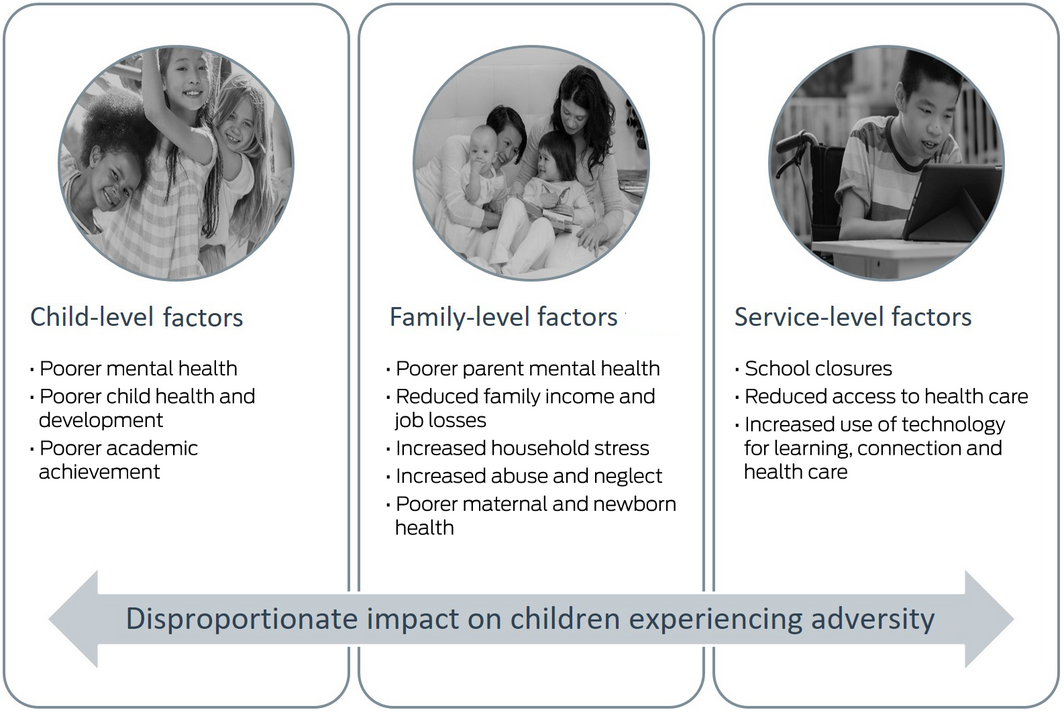
This narrative review synthesises the literature on the potential adverse indirect impacts of the COVID‐19 pandemic on children, using a community child health lens to organise our findings. Our literature search strategy (Box 2) consisted of two parts: (i) previous pandemics, epidemics and natural disasters; and (ii) the current COVID‐19 pandemic. We identified 11 impact areas, under three broad lenses that align with community child health (Box 3). Given the broad remit of community child health, there may be additional adverse impacts yet to be reflected in the published research.
Child‐level factors
Poorer mental health
There appear to be serious negative impacts on children’s mental health during pandemics;28,29,30 however, longitudinal research investigating the longer term impacts is lacking.31 After the 2009 H1N1 influenza pandemic, 30% of children who experienced isolation (in the United States, Mexico and Canada) met the threshold for post‐traumatic stress disorder, increasing to nearly 86% for those whose parents met the threshold.32 Studies have shown the negative impact of COVID‐19 restrictions on children’s mental health.33,34,35,36,37 In Australia, mental health difficulties significantly increased for children who experienced a second lockdown (20–46% in high range; 2–13% in very high range) compared with a normative sample.38 There has been a rapid increase in demand for Kids Helpline, the Australian national youth helpline, with common reasons for contact including mental health (4.6% monthly increase) and suicidal ideation or self‐harm (5.7% monthly increase).39 Additionally, some children with existing mental health disorders have experienced an exacerbation of symptoms.40,41
Poorer child health and development
Pandemics are related to increased rates of improper nutrition and dramatic changes in children’s play.30 Sports centres and play spaces closed in many countries as part of COVID‐19 restrictions,42 resulting in reduced daily physical activity, increased screen time, increased snacking, and weight gain.14,33,43,44,45 In a longitudinal study of 14 countries (including Australia), children spent 55 minutes more per day in sedentary screen time, and 81 minutes less per weekday outdoors during COVID‐19 restrictions.46 The risks for children with additional health care needs (eg, developmental and behavioural issues) are even greater, with limited access to health care, school and support services, including early intervention.14,25,41,42,47,48,49,50 Missed routine child health checks may lead to lower rates of children being identified as experiencing developmental delays.14 Alternately, there is evidence of improvements in childhood asthma outcomes,51 decreased incidence of influenza52,53 and enterovirus and norovirus infections,54 and possible reductions in preterm birth rates.55,56
Poorer academic achievement
Following the Victorian Black Saturday bushfires in 2009, expected gains in reading and numeracy scores were reduced for primary school students in schools with higher bushfire impact.57 Almost half of the Australian student population risks having their learning severely compromised due to COVID‐19‐related school closures, either because they are an early years student or are experiencing adversity.58,59 Families may lack the resources and time needed to support their children’s learning, particularly parents with lower levels of educational attainment.58 Student engagement is more significantly compromised among children experiencing adversity, and it is predicted that re‐engagement in the school context will be diminished, with poorer academic outcomes.15,48,58,59,60,61 The estimated achievement gap between disadvantaged and advantaged students grows at triple the rate during remote learning compared with on‐site learning,61 with the value of gross domestic product lost from one‐third of a year of remote learning estimated to be US$871 billion in Australia.62 Recent data suggest that children born during the pandemic may already be demonstrating reduced cognitive performance.63
Family‐level factors that affect children
Poorer parent mental health
Mental health needs are rarely prioritised during pandemics, with limited access to trained mental health professionals.64 Following the 2009 H1N1 influenza pandemic, 25% of parents who were required to isolate met criteria for post‐traumatic stress disorder symptoms.32 During COVID‐19 restrictions, parents experienced poorer mental health, particularly those with pre‐existing health problems, with a child with additional health care needs, or experiencing socio‐economic disadvantage.65,66 In Australia, 46% of parents reported a negative impact on their mental health,33 while parent mental distress tripled from 8% before COVID‐19 to 24% during the pandemic.67 Lifeline Australia reported its highest volume of calls in its 58‐year history in the first week of August 2021, while much of Australia was in lockdown.68
Reduced family income and job losses
Previous pandemics and epidemics have been associated with increased job losses and poverty, with harsher economic impacts for families experiencing adversity.30 In Australia, many families experienced job losses or reduced household income during COVID‐19 restrictions.33,69,70 Deteriorating economic circumstances have resulted in higher rates of newly disadvantaged families and increased levels of persistent disadvantage.16,58 For parents experiencing unemployment and financial instability, the added burden of assuming the role of educator within the household may be difficult,15 with economic pressure related to higher parental stress and harsher parenting.71
Increased household stress
Increased family conflict and negative impacts on parent–child relationships were evident during previous pandemics.30 Marital dissatisfaction and divorce increases following natural disasters, due to increased stress and mental health difficulties, and disrupted external social support.71 During COVID‐19 restrictions, increases in caregiver stress are likely to decrease caregiving capacity.16 In Australia, parents reported increased strain on parent–child relationships.40 Many families have struggled to support their children’s remote learning needs and other child care demands, while also balancing employment demands (including working from home requirements) or unemployment and financial instability.14,15,72
Increased abuse and neglect
The risk of child abuse and neglect increases during pandemics, due to increased stress and isolation for families and reduced access to support.30,73 COVID‐19 restrictions (eg, school closures74 and job losses75) are expected to have led to increased levels of family violence and child maltreatment.13,14,16,76 The risk is greater among children experiencing adversity,77 with reduced access to child protection services74 and restricted child welfare visits.14,25,60 A marked increase in the incidence of abuse‐related head injuries among children was reported at the start of the COVID‐19 pandemic.78 Reports to child maltreatment hotlines decreased substantially, likely largely due to decreased contact between children and both education personnel and health services.76,79 In the US, criminal charges pertaining to child abuse or neglect were also lower than forecasted in the first months of the pandemic.80 However, Australian data indicated that notifications made to child protection services increased once restrictions eased73 and children were able to leave their home environment, potentially due to a combination of more face‐to‐face health appointments, schools reopening, and mandatory reporting laws for education personnel.
Poorer maternal and newborn health
In utero exposure to pandemics and natural disasters via maternal stress may have long term negative effects on educational attainment, lifelong earnings, and mental health problems.16 Pregnant and postnatal women have reported increased anxiety and depression during COVID‐19 restrictions.81,82 New callers to the Perinatal Anxiety and Depression Australia helpline doubled during March–October 2020, as did duration of call times.83 Many new parents were isolated from family and friends,84 with limited access to face‐to‐face health services,85 often leading to inadequate infant weight gain and increased hospital admissions.86 Higher risk groups, such as new parents with a baby in a neonatal intensive care unit, may have particularly high rates of mental health problems.84,87
Service‐level factors that affect children
School closures
By April 2020, remote learning had been implemented around the world.88 School closures affected about 86% of the global student population,89 including around 4 million Australian students.15 Early childhood education and care services also closed in many countries,90,91 including parts of Australia (Box 1). Many families withdrew their children from both formal and informal child care,92 including grandparent care.93 School closures have been associated with a loss of access to school‐facilitated health care, including free lunches and mental health care.11,17,23,43 These impacts disproportionately affect children experiencing adversity.30,94,95 US estimates have suggested public primary school closures could be associated with an estimated 13.8 million years of life lost due to decreased long term educational attainment.96
Reduced access to health care
Health care infrastructure can quickly become overwhelmed during pandemics.97,98 During the COVID‐19 pandemic, access to essential child health services has been limited at times in Australia, with some specialists unable to take on new patients, despite large waiting lists.19 Developmental–behavioural paediatric service delivery primarily moved to telehealth.99 This brought additional challenges for patients with complex needs. For instance, only 30% of parents of children with neurodevelopmental disabilities reported that telehealth worked well for their child.49 Referrals to child mental health services reduced substantially, before an unprecedented rise that placed increased demand on already overstretched services.100 In early 2020, fewer services were provided to children, from Headspace primary youth mental health services in Victoria101 to the Child Dental Benefits Schedule.102 Alternately, there was no decrease in the proportion of young Australian children fully immunised in 2020.103 Paediatric emergency department visits decreased,104,105 partly due to lower rates of infections and injuries.104 However, 31% of unwell or injured Australian children delayed or avoided accessing health care, primarily because of parental fear of exposure to COVID‐19.33 Conversely, there has been a substantial increase in paediatric mental health presentations to emergency departments.105
Increased use of technology for learning, connection and health care
Technological solutions have been important approaches for addressing the effects of the COVID‐19 pandemic,48 for instance through the rapid advancement of telehealth. Yet evidence for the efficacy of telehealth and the impacts of remote learning remain unclear.99,101 Schools have used technology to move the education curriculum to a remote learning environment; however, many children do not have the necessary skills or self‐confidence to use technology for learning, particularly younger children and those experiencing adversity.15 In 2013, it was estimated that only 68% of children living in Australia’s most disadvantaged communities had access to the internet at home.106 Technology has also been used to facilitate social interactions between children in an attempt to alleviate loneliness and maintain a sense of connectedness.13,48 Connection to extended family and the wider community has also largely been limited to being facilitated by technology. Although yet unknown, this may have both hindered local social connections (with less supervision of children and supports for families) but strengthened other connections for families living far apart. Telehealth services rapidly expanded as they became an essential aspect of children’s health and developmental care,12 while also trying to ensure that existing inequities in access to care were not exacerbated.47,107 In Australia, 27% of children accessed telehealth in 2020, with the majority of parents reporting finding it convenient for their family.108
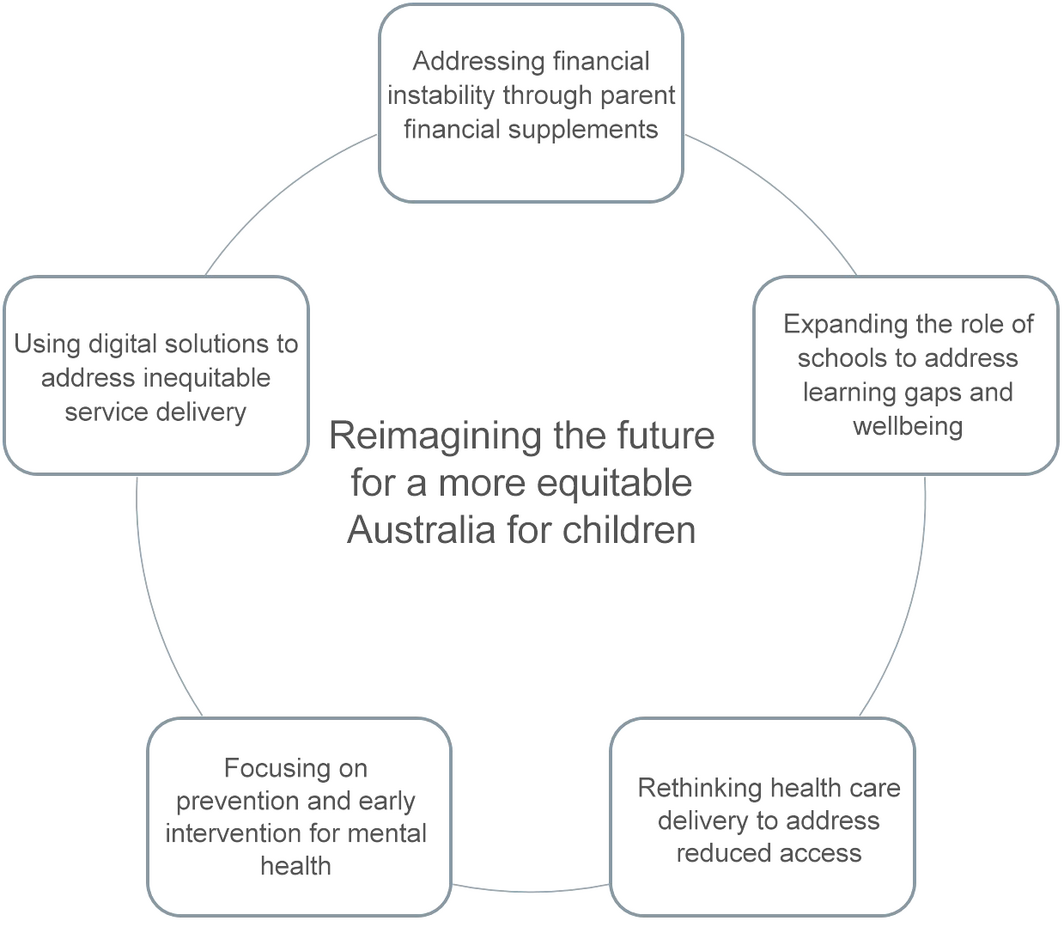
Strategies for the future
This narrative review brings together vast and burgeoning research that shines a spotlight on the potential indirect adverse impacts of the COVID‐19 pandemic on children, and on the possible widening of existing health disparities that must not be ignored.3,17,21,22,23 Without proper planning, evaluation and policy commitment, the inequitable and likely long‐lasting impacts of COVID‐19 restrictions will be inevitable.
Taking into account the opportunity created by the pandemic disruptors and rapid technological advances, we propose five potential strategy areas that underpin community child health, with a focus on both upstream and downstream determinants of health, highlighting the need to work across sectors (Box 4). They are not designed to be all encompassing, but rather point to areas of immediate policy relevance and likely impact based on the findings of this review. Because of the complexity of child development and the multifactorial nature of adversity and ensuing inequities, these five strategy areas will be most effective if considered both within place‐based system change that embeds thoughtful co‐design, implementation and evaluation, and at whole system levels such as state and national policy (where many are already considered but not yet implemented or coordinated). Place‐based approaches in particular, given the current state and federal policy interest (eg, Stronger Places, Stronger People),109,110 provide a timely option for the co‐implementation of all of these strategies. This could best meet more acute community need while also building the efficacy and resilience of communities for future crises.
Addressing financial instability through parent financial supplements
International trials show the benefit of conditional and non‐conditional cash transfers for children’s developmental outcomes.111,112 The newly expanded US child tax credit113,114 is direct recognition that parents of young children will be affected by a combination of job losses, home schooling and poorer mental health due to the COVID‐19 pandemic. There is an opportunity to converge what we know about the importance of early childhood development with the importance of social determinants and develop a parent financial supplement that recognises the importance of early childhood; is of sufficient scale to offset the potential damage of COVID‐19 restrictions; and takes an approach that invests in the future of Australian children. In Australia, the advent of JobKeeper (a wage supplement for eligible businesses to retain their workforce)115 and the increase to JobSeeker (unemployment benefit) supplements were so impactful that by September 2020, the estimated number of people living in poverty reduced by around 32%.116 It is perhaps timely to review Australia’s Family Tax Benefit117 system to meet the needs of the 68% of families with children under 5 years of age who are experiencing financial stress.70
Expanding the role of schools to address learning gaps and wellbeing
COVID‐19 restrictions made it clear that children need to be at school to both learn and be well.61 The Learning through COVID‐19 project, undertaken by the Institute for Social Science Research at the University of Queensland, highlights four action areas to address worsening educational disadvantage in Australia: student mental health; the future roles of teachers and communities; digital equity; and protections for vulnerable students.118 As such, there is the need for more systematic attention to and investments in children’s health and wellbeing at school.119 For example, the Victorian Framework for Improving Student Outcomes120 now explicitly places children’s learning and wellbeing as central to school improvement. Schools could be articulated as public health universal platforms, with a focus on promotion, prevention and equity in both learning and wellbeing (including accountability metrics119), noting the connection with the years before school (eg, preschool).
Rethinking health care delivery to address reduced access
Access to routine child health services has been limited at times in Australia during the COVID‐19 pandemic.19 There is a plethora of interest in a more integrated approach to health care, including co‐location and hubs in policies like the Royal Commission into Victoria’s Mental Health System,121 the National Children’s Mental Health and Wellbeing Strategy,122 and the National Action Plan for the Health of Children and Young People.123 Integrated service hubs provide the opportunity to bring together health and social care to best meet the needs of the population, especially in geographic areas where families are experiencing adversity. These policies, which include a focus on the first 2000 days of life,124 could facilitate practitioners working together to ensure that services are co‐designed and respond to the needs of children and their families, use evidence‐based care, and fund evaluation to determine if care is making a difference.125
Focusing on prevention and early intervention for mental health
Growing evidence for the impact of COVID‐19 restrictions on mental health is alarming, given an already high prevalence of childhood mental health disorders that are unequally distributed.126 Governments are contributing large amounts of funding for mental health services, with pre‐pandemic processes such as the Productivity Commission report on mental health127 and the Royal Commission into Victoria’s Mental Health System121 pointing to an already fragmented and inadequate system. While this is a pivotal time to address acute need, reform should be anchored in prevention and early intervention. Government reforms in areas such as primary health care,128 mental health121,127 and community health129 provide the opportunity for funding model reforms across universal and primary health services to re‐orient service, program and workforce delivery to prevention and early intervention. As detailed in the National Children’s Mental Health and Wellbeing Strategy,122 there should be a focus on empowering families and using community‐based approaches; the important role of education settings; and embedding a culture of evaluation into mental health supports. There must also be a focus on reducing inequities.130
Using digital solutions to address inequitable service delivery
There is the potential to use existing digital solutions to integrate digital navigation and digital interventions. The Australian government‐funded Raising Children Network website received over 43.5 million page views in 2020 (an increase of 30% from the previous year), with a particular peak in COVID‐19 advice.131 Digital technologies can be designed to help deliver equitable, high quality care across Australia and potentially to create a digital overlay to our currently fragmented services through digital navigation and therapies. With the right training,123 and guidelines to drive excellent care,132 this could revolutionise the way we reach families and deliver the services they need, creating a more accessible and efficient service delivery system.
Conclusion
The indirect impacts of COVID‐19 and related policy responses will likely have broad, long‐lasting implications for children. History shows us that children already experiencing adversity lose out the most,22 with the potential for widening health inequities.119 The international body of literature emerging from the COVID‐19 pandemic suggests that now is the time to not only repair the past, but to start to re‐imagine the future for a more equitable Australia for children. The COVID‐19 pandemic has highlighted that it is possible to make transformational changes that could deliver on community child health aspirations. We have the opportunity to build a better and more equitable Australia, for the children of today and the adults of the future.17
Box 1 – Summary of two of the strictest periods of COVID‐19 public health restrictions in Australia
|
|
Australia‐wide Stage 3 restrictions |
Melbourne* Stage 4 restrictions |
|||||||||||||
|
|
|||||||||||||||
|
Physical distancing† |
Recommendations in place |
Recommendations in place |
|||||||||||||
|
Leaving home |
Only four reasons to leave home: food and supplies; exercise, medical care or compassionate reasons; and work and education, if necessary |
Only four reasons to leave home: food and supplies; exercise, medical care or compassionate reasons; and work and education, if necessary |
|||||||||||||
|
|
|
Exercise limited to maximum of one hour per day, within 5 km from home, with a maximum of one other person |
|||||||||||||
|
|
|
Shopping limited to one person per household per day, within 5 km from home |
|||||||||||||
|
|
|
Curfew from 8 pm to 5 am |
|||||||||||||
|
|
|
Face coverings compulsory at all times for adults and children over 12 years of age |
|||||||||||||
|
Schools |
Schools closed (except for vulnerable children and children of permitted workers) and remote learning commenced |
Schools closed (except for vulnerable children and children of permitted workers) and remote learning commenced |
|||||||||||||
|
|
|
Kindergartens and childcare centres closed (except for vulnerable children and children of permitted workers) |
|||||||||||||
|
Non‐essential services |
Closed (eg, restaurants and cafes, indoor play centres, public swimming pools, libraries, community centres) |
Closed (eg, retail stores, restaurants and cafes, indoor play centres, public swimming pools, libraries, community centres) |
|||||||||||||
|
Outdoor recreation |
Closed (eg, playgrounds, skate parks) |
Closed (eg, playgrounds, skate parks) |
|||||||||||||
|
Hospital visitors |
Restricted (eg, birthing suites, maternity wards, newborn intensive care units, special care nurseries) |
Restricted (eg, birth centres, maternity wards, newborn intensive care units, special care nurseries) |
|||||||||||||
|
Private gatherings |
Not allowed |
Not allowed |
|||||||||||||
|
Public gatherings |
Restricted to two people |
Not allowed |
|||||||||||||
|
Weddings |
Capped at five people |
Not allowed |
|||||||||||||
|
Funerals |
Capped at ten people |
Capped at ten people |
|||||||||||||
|
Home quarantine |
Anyone classified as a close contact of a COVID‐19 case required to quarantine at home for 14 days |
Anyone classified as a close contact of a COVID‐19 case required to quarantine at home for 14 days |
|||||||||||||
|
|
|||||||||||||||
|
COVID‐19 = coronavirus disease 2019. * In Melbourne, a second wave of the COVID‐19 pandemic resulted in a return to Stage 3 restrictions in July 2020 before entering a new Stage 4 lockdown, the longest and strictest lockdown in Australia to date. From September 2020, a slow return to normal COVID‐19 restrictions began. † Physical distancing is a term used to describe the Australian Government’s recommendations around keeping a distance of 1.5 m from others, not shaking hands or hugging, and avoiding crowds and mass gatherings.10 This recommendation has been in place for the duration of the COVID‐19 pandemic. |
|||||||||||||||
Box 2 – Search strategy using the PubMed database
|
Search strategy |
Date range |
Search terms |
Initial search |
Exclusion criteria |
|||||||||||
|
|
|||||||||||||||
|
Previous pandemics, epidemics and natural disasters |
Articles before 31 Dec 2019 |
(“pandemic” or “epidemic” or “natural disaster”); “child”; and (“social” or “emotional” or “mental” or “physical” or “academic”) |
2426 articles |
|
|||||||||||
|
Current COVID‐19 pandemic |
Articles before 15 Oct 2021 |
(“COVID‐19” or “coronavirus” or “SARS‐CoV‐2”); “child”; and (“social” or “emotional” or “mental” or “physical” or “academic”)* |
3686 articles |
|
|||||||||||
|
|
|||||||||||||||
|
COVID‐19 = coronavirus disease 2019; SARS‐CoV‐2 = severe acute respiratory coronavirus 2. * Given the rapid and emerging nature of this research,27 we included opinion pieces such as journal perspectives, editorials and reviews, as well as original research. |
|||||||||||||||
- Sharon Goldfeld1,2
- Elodie O'Connor1
- Valerie Sung1,2
- Gehan Roberts1,2
- Melissa Wake1,2
- Sue West1
- Harriet Hiscock1,2
- 1 Centre for Community Child Health, Murdoch Children’s Research Institute, The Royal Children's Hospital Melbourne, Melbourne, VIC
- 2 University of Melbourne, Melbourne, VIC
Sharon Goldfeld is supported by National Health and Medical Research Council (NHMRC) Practitioner Fellowship 1155290. Valerie Sung is supported by a Melbourne Children’s Clinician Scientist Fellowship 2021. Melissa Wake is supported by NHMRC Principal Research Fellowship 1160906. Harriet Hiscock is supported by NHMRC Practitioner Fellowship 1136222. We thank Jacqueline Ding for her contribution to the literature review.
No relevant disclosures.
- 1. McGorry P. Mental health and COVID‐19: are we really all in this together? Med J Aust 2020; 213: 454–455. https://www.mja.com.au/journal/2020/213/10/mental‐health‐and‐covid‐19‐are‐we‐really‐all‐together
- 2. Shen K‐L, Yang Y‐H, Jiang R‐M, et al. Updated diagnosis, treatment and prevention of COVID‐19 in children: experts’ consensus statement (condensed version of the second edition). World J Pediatr 2020; 16: 232–239.
- 3. Rajmil L, Hjern A, Boran P, et al. Impact of lockdown and school closure on children’s health and well‐being during the first wave of COVID‐19: a narrative review. BMJ Paediatr Open 2021; 5: e001043.
- 4. Ibrahim LF, Tham D, Chong V, et al. The characteristics of SARS‐CoV‐2‐positive children who presented to Australian hospitals during 2020: a PREDICT network study. Med J Aust 2021; 215: 217–221. https://www.mja.com.au/journal/2021/215/5/characteristics‐sars‐cov‐2‐positive‐children‐who‐presented‐australian‐hospitals
- 5. McLaws ML. COVID‐19 in children: time for a new strategy. Med J Aust 2021; 215: 212–213. https://www.mja.com.au/journal/2021/215/5/covid‐19‐children‐time‐new‐strategy
- 6. Sakzewski E. Australia is moving to stage 2 restrictions to curb the coronavirus outbreak. Here’s what’s included. ABC News 2020; 25 Mar. https://www.abc.net.au/news/2020‐03‐25/what‐is‐open‐or‐closed‐in‐australia‐now‐because‐of‐coronavirus/12087894 (viewed Nov 2021).
- 7. ABC News. Victoria in stage 3 coronavirus shutdown restrictions as cases climb to 821. ABC News 2020; 30 Mar. https://www.abc.net.au/news/2020‐03‐30/victoria‐stage‐3‐coronavirus‐restrictions‐as‐cases‐rise/12101632 (viewed Nov 2021).
- 8. Victoria State Government Department of Health and Human Services. Premier’s statement on changes to Melbourne’s restrictions. 2 Aug 2020. https://www.dhhs.vic.gov.au/updates/coronavirus‐covid‐19/premiers‐statement‐changes‐melbournes‐restrictions‐2‐august‐2020 (viewed May 2021).
- 9. Victoria State Government. Summary of restrictions — move to stage 4 6pm 2 August 2020. http://www.jaclynsymes.com.au/wp‐content/uploads/2020/08/Corona‐20200802.pdf (viewed Aug 2021).
- 10. Australian Government Department of Health. Physical distancing for coronavirus (COVID‐19). https://www.health.gov.au/news/health‐alerts/novel‐coronavirus‐2019‐ncov‐health‐alert/how‐to‐protect‐yourself‐and‐others‐from‐coronavirus‐covid‐19/physical‐distancing‐for‐coronavirus‐covid‐19 (viewed May 2021).
- 11. Generation coronavirus? [editorial]. Lancet 2020; 395: 1949.
- 12. Ye J. Pediatric Mental and behavioral health in the period of quarantine and social distancing with COVID‐19. JMIR Pediatr Parent 2020; 3: e19867.
- 13. Galea S, Merchant RM, Lurie N. The mental health consequences of COVID‐19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med 2020; 180: 817–818.
- 14. Chanchlani N, Buchanan F, Gill P. Addressing the indirect effects of COVID‐19 on the health of children and young people. CMAJ 2020; 192: E921–E927.
- 15. Drane C, Vernon L, O’Shea S. The impact of ‘learning at home’ on the educational outcomes of vulnerable children in Australia during the COVID‐19 pandemic. Perth: National Centre for Student Equity in Higher Education, Curtin University, 2020. https://www.ncsehe.edu.au/wp‐content/uploads/2020/04/NCSEHE_V2_Final_literaturereview‐learningathome‐covid19‐final_30042020.pdf (viewed Apr 2020).
- 16. Yoshikawa H, Wuermli A, Britto P, et al. Effects of the global coronavirus disease‐2019 pandemic on early childhood development: Short‐ and long‐term risks and mitigating program and policy actions. J Pediatr 2020; 223: 188–193.
- 17. Whitehead M, Taylor‐Robinson D, Barr B. Poverty, health, and covid‐19. BMJ 2021; 372: n376.
- 18. Roubinov D, Bush NR, Boyce WT. How a pandemic could advance the science of early adversity. JAMA Pediatr 2020; 174: 1131–1132.
- 19. Eapen V, Hiscock H, Williams K. Adaptive innovations to provide services to children with developmental disabilities during the COVID‐19 pandemic. J Paediatr Child Health 2021; 57: 9–11.
- 20. Aknin L, De Neve J, Dunn E, et al. Mental health during the first year of the COVID‐19 pandemic: a review and recommendations for moving forward [preprint]. PsyArXiv 2021; https://doi.org/10.31234/osf.io/zw93g (viewed Nov 2021).
- 21. Hefferon C, Taylor C, Bennett D, et al. Priorities for the child public health response to the COVID‐19 pandemic recovery in England. Arch Dis Childhood 2021; 106: 533–538.
- 22. Sinha I, Bennett D, Taylor‐Robinson DC. Children are being sidelined by COVID‐19. BMJ 2020; 369: m2061.
- 23. Van Lancker W, Parolin Z. COVID‐19, school closures, and child poverty: a social crisis in the making. Lancet Public Health 2020; 5: e243–e244.
- 24. Spencer N, Colomer C, Alperstein G, et al. Social paediatrics. J Epidemiol Community Health 2005; 59: 106–108.
- 25. Suleman S, Ratnani Y, Stockley K, et al. Supporting children and youth during the COVID‐19 pandemic and beyond: A rights‐centred approach. Paediatr Child Health 2020; 25: 333–336.
- 26. O’Keeffe M. Clinical competence in developmental‐behavioural paediatrics: raising the bar. J Paediatr Child Health 2014; 50: 3–10.
- 27. University of Melbourne Department of Paediatrics. COVID‐19 kids research evidence update. 20 Dec 2020. https://medicine.unimelb.edu.au/school‐structure/paediatrics/news‐and‐events/covid‐19_kids_research_evidence_update (viewed Dec 2020).
- 28. Berger E, Jamshidi N, Reupert A, et al. Review: the mental health implications for children and adolescents impacted by infectious outbreaks ‐ a systematic review. Child Adolesc Ment Health 2021; 26: 157–166.
- 29. Meherali S, Punjani N, Louie‐Poon S, et al. Mental health of children and adolescents amidst COVID‐19 and past pandemics: a rapid systematic review. Int J Environ Res Public Health 2021; 18: 3432.
- 30. Merrill K, William T, Joyce KM, et al. Potential psychosocial impact of COVID‐19 on children: a scoping review of pandemics & epidemics. J Global Health Rep 2021; 4: e2020106.
- 31. Fong V, Iarocci G. Child and family outcomes following pandemics: a systematic review and recommendations on COVID‐19 policies. J Pediatric Psychol 2020; 45: 1124–1143.
- 32. Sprang G, Silman M. Posttraumatic stress disorder in parents and youth after health‐related disasters. Disaster Med Public Health Prep 2013; 7: 105–110.
- 33. Royal Children’s Hospital National Child Health Poll. COVID‐19 pandemic: effects on the lives of Australian children and families. Melbourne: RCH, 2020. https://www.rchpoll.org.au/polls/covid‐19‐pandemic‐effects‐on‐the‐lives‐of‐australian‐children‐and‐families/ (viewed Oct 2020).
- 34. Commission for Children and Young People. Impact of COVID‐19 on children and young people: mental health. Melbourne: CCYP, 2020. https://ccyp.vic.gov.au/assets/COVID‐Engagement/CCYP‐Mental‐Health‐Snapshot‐web.pdf (viewed Sept 2020).
- 35. Racine N, Cooke JE, Eirich R, et al. Child and adolescent mental illness during COVID‐19: a rapid review. Psychiatry Res 2020; 292: 113307.
- 36. Bignardi G, Dalmaijer ES, Anwyl‐Irvine AL, et al. Longitudinal increases in childhood depression symptoms during the COVID‐19 lockdown. Arch Dis Childhood 2021; 106: 791–797.
- 37. Singh S, Roy D, Sinha K, et al. Impact of COVID‐19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res 2020; 293: 113429.
- 38. De Young A, Paterson R, March S, et al. COVID‐19 unmasked. Report 2: Impact of the second wave in Australia on the mental health of young children and parents. Brisbane: Queensland Centre for Perinatal and Infant Mental Health, Children’s Health Queensland Hospital and Health Service, 2021. https://www.childrens.health.qld.gov.au/wp‐content/uploads/PDF/COVID‐19/COVID19‐Unmasked‐Survey‐Progress‐Report‐02.pdf (viewed July 2021).
- 39. Batchelor S, Stoyanov S, Pirkis J, Kõlves K. Use of Kids Helpline by children and young people in Australia during the COVID‐19 pandemic. J Adolesc Health 2021; 68: 1067–1074.
- 40. Evans S, Mikocka‐Walus A, Klas A, et al. From “it has stopped our lives” to “spending more time together has strengthened bonds”: the varied experiences of Australian families during COVID‐19. Front Psychol 2020; 11: 588667.
- 41. Sciberras E, Patel P, Stokes MA, et al. Physical health, media use, and mental health in children and adolescents with ADHD during the COVID‐19 pandemic in Australia. J Atten Disord 2020; 1087054720978549.
- 42. Yarımkaya E, Esentürk OK. Promoting physical activity for children with autism spectrum disorders during Coronavirus outbreak: benefits, strategies, and examples. Int J Dev Disabil 2020; https://doi.org/10.1080/20473869.2020.1756115.
- 43. Pandemic school closures: risks and opportunities [editorial]. Lancet Child Adolesc Health 2020; 4: 341.
- 44. Carroll N, Sadowski A, Laila A, et al. The impact of COVID‐19 on health behavior, stress, financial and food security among middle to high income Canadian families with young children. Nutrients 2020; 12: 1–14.
- 45. Lanza K, Durand CP, Alcazar M, et al. School parks as a community health resource: use of joint‐use parks by children before and during COVID‐19 pandemic. Int J Environ Res Public Health 2021; 18: 9237.
- 46. Okely AD, Kariippanon KE, Guan H, et al. Global effect of COVID‐19 pandemic on physical activity, sedentary behaviour and sleep among 3‐ to 5‐year‐old children: a longitudinal study of 14 countries. BMC Public Health 2021; 21: 940.
- 47. Provenzi L, Borgatti R. Potentials of telerehabilitation for families of children with special health care needs during the coronavirus disease 2019 emergency. JAMA Pediatrics 2021; 175: 105–106.
- 48. Goldschmidt K. The COVID‐19 pandemic: technology use to support the wellbeing of children. J Pediatr Nurs 2020; 53: 88–90.
- 49. Masi A, Mendoza Diaz A, Tully L, et al. Impact of the COVID‐19 pandemic on the well‐being of children with neurodevelopmental disabilities and their parents. J Paediatr Child Health 2021; 57: 631–636.
- 50. Theis N, Campbell N, De Leeuw J, et al. The effects of COVID‐19 restrictions on physical activity and mental health of children and young adults with physical and/or intellectual disabilities. Disabil Health J 2021; 14: 101064.
- 51. Papadopoulos NG, Mathioudakis AG, Custovic A, et al. Childhood asthma outcomes during the COVID‐19 pandemic: findings from the PeARL multinational cohort. Allergy 2021; 76: 1765–1775.
- 52. Olsen S, Azziz‐Baumgartner E, Budd A, et al. Decreased influenza activity during the COVID‐19 pandemic — United States, Australia, Chile, and South Africa, 2020. MMWR Morb Mortal Wkly Rep 2020; 69: 1305–1309.
- 53. Australian Government Department of Health. Australian Influenza Surveillance Report ‐ 2020 national influenza season summary. Canberra: Commonwealth of Australia, 2020. https://www1.health.gov.au/internet/main/publishing.nsf/Content/ozflu‐surveil‐season‐summary‐2020.htm (viewed Aug 2021).
- 54. Bruggink LD, Garcia‐Clapes A, Tran T, et al. Decreased incidence of enterovirus and norovirus infections during the COVID‐19 pandemic, Victoria, Australia, 2020. Commun Dis Intell (2018) 2021; 45: https://doi.org/10.33321/cdi.2021.45.5.
- 55. Goldenberg RL, McClure EM. Have Coronavirus disease 2019 (COVID‐19) community lockdowns reduced preterm birth rates? Obstet Gynecol 2021; 137: 399–402.
- 56. Matheson A, McGannon CJ, Malhotra A, et al. Prematurity rates during the coronavirus disease 2019 (COVID‐19) pandemic lockdown in Melbourne, Australia. Obstet Gynecol 2021; 137: 405–407.
- 57. Gibbs L, Nursey J, Cook J, et al. Delayed disaster impacts on academic performance of primary school children. Child Dev 2019; 90: 1402–1412.
- 58. Brown N, te Riele K, Shelley B, Woodroffe J. Learning at home during COVID‐19: effects on vulnerable young Australians. Hobart: Peter Underwood Centre for Educational Attainment, University of Tasmania; 2020. https://www.utas.edu.au/__data/assets/pdf_file/0008/1324268/Learning‐at‐home‐during‐COVID‐19‐updated.pdf (viewed Apr 2020).
- 59. Lamb S. Impact of learning from home on educational outcomes for disadvantaged children. Melbourne: Victoria University, 2020. https://www.vu.edu.au/sites/default/files/impact‐of‐learning‐from‐home‐federal‐government‐brief‐mitchell‐institute.pdf (viewed Apr 2020).
- 60. Clinton J. Supporting vulnerable children in the face of a pandemic. Melbourne: Centre for Program Evaluation, University of Melbourne, 2020.
- 61. Sonnemann J, Goss P. COVID catch‐up: helping disadvantaged students close the equity gap. Melbourne: Grattan Institute, 2020.
- 62. Hanushek E, Woessman L. The economic impacts of learning losses. Paris: OECD Publishing, 2020.
- 63. Deoni SC, Beauchemin J, Volpe A, et al. Impact of the COVID‐19 pandemic on early child cognitive development: initial findings in a longitudinal observational study of child health [preprint]. medRxiv 2021; 2021.08.10.21261846.
- 64. Decosimo CA, Hanson J, Quinn M, et al. Playing to live: outcome evaluation of a community‐based psychosocial expressive arts program for children during the Liberian Ebola epidemic. Glob Ment Health (Camb) 2019; 6: e3.
- 65. Davidson B, Schmidt E, Mallar C, et al. Risk and resilience of well‐being in caregivers of young children in response to the COVID‐19 pandemic. Transl Behav Med 2021; 11: 305–311.
- 66. Westrupp EM, Stokes MA, Fuller‐Tyszkiewicz M, et al. Subjective wellbeing in parents during the COVID‐19 pandemic in Australia. J Psychosom Res 2021; 145: 110482.
- 67. Broadway B, Payne AA, Salamanca N. Coping with COVID‐19: rethinking Australia. Melbourne: Melbourne Institute: Applied Economic & Social Research. University of Melbourne, 2020. https://melbourneinstitute.unimelb.edu.au/__data/assets/pdf_file/0004/3562906/Coping‐with‐COVID‐19‐Rethinking‐Australia.pdf (viewed Aug 2021).
- 68. Lifeline Australia. More Australians than ever seeking crisis support [media release]. 4 Aug 2021. https://www.lifeline.org.au/resources/news‐and‐media‐releases/media‐releases/ (viewed Aug 2021).
- 69. Baxter J, Warren D. Employment and work–family balance in 2020 (Families in Australia Report No. 2). Melbourne: Australian Institute of Family Studies, 2021. https://aifs.gov.au/publications/employment‐work‐family‐balance‐2020 (viewed July 2021).
- 70. Gamara A, Goldfeld S, Mallett S, et al. Which families are feeling the pinch of the pandemic the most? (Access Research Insights No. 14/21). Melbourne: Melbourne Institute, 2021. https://blogs.rch.org.au/ccch/files/2021/11/2110‐ResearchInsight‐1421pdf.pdf (viewed Oct 2021).
- 71. Prime H, Wade M, Browne D. Risk and resilience in family well‐being during the COVID‐19 Pandemic. Am Psychol 2020; 75: 631–643.
- 72. Spinelli M, Lionetti F, Pastore M, Fasolo M. Parents’ stress and children’s psychological problems in families facing the COVID‐19 outbreak in Italy. Front Psychol 2020; 11: 1713.
- 73. Australian Institute of Health and Welfare. Child protection in the time of COVID‐19 (Cat. No. CWS 76). Canberra: AIHW, 2021. https://www.aihw.gov.au/getmedia/720b3a97‐d76d‐4122‐80ca‐6c1818285baa/aihw‐cws‐76‐child‐protection‐in‐the‐time‐of‐covid19.pdf.aspx?inline=true (viewed July 2021).
- 74. Commission for Children and Young People. Impact of COVID‐19 on children and young people: safety. Melbourne: CCYP, 2020. https://ccyp.vic.gov.au/assets/COVID‐Engagement/CCYP‐Safety‐Snapshot‐web.pdf (viewed Sept 2020).
- 75. Lawson M, Piel MH, Simon M. Child maltreatment during the COVID‐19 pandemic: consequences of parental job loss on psychological and physical abuse towards children. Child Abuse Neglect 2020; 110: 104709.
- 76. Bhatia A, Fabbri C, Cerna‐Turoff I, et al. COVID‐19 response measures and violence against children. Bull World Health Organ 2020; 98: 583–583A.
- 77. Greeley CS. Child maltreatment prevention in the era of coronavirus disease 2019. JAMA Pediatr 2020; 174: e202776.
- 78. Sidpra J, Abomeli D, Hameed B, et al. Rise in the incidence of abusive head trauma during the COVID‐19 pandemic. Arch Dis Childhood 2021; 106: e14.
- 79. Katz I, Katz C, Andresen S, et al. Child maltreatment reports and Child Protection Service responses during COVID‐19: knowledge exchange among Australia, Brazil, Canada, Colombia, Germany, Israel, and South Africa. Child Abuse Negl 2021; 116: 105078.
- 80. Whelan J, Hartwell M, Chesher T, et al. Deviations in criminal filings of child abuse and neglect during COVID‐19 from forecasted models: an analysis of the state of Oklahoma, USA. Child Abuse Negl 2021; 116: 104863.
- 81. Bradfield Z, Wynter K, Hauck Y, et al. Experiences of receiving and providing maternity care during the COVID‐19 pandemic in Australia: a five‐cohort cross‐sectional comparison. PLoS One 2021; 16: e0248488.
- 82. Ahmad M, Vismara L. The psychological impact of COVID‐19 pandemic on women’s mental health during pregnancy: a rapid evidence review. Int J Environ Res Public Health 2021; 18: 7112.
- 83. Polchleb C, Sung L. COVID‐19 and pandemic perinatal mental health in Australia. Aust J Gen Pract 2021; 50: https://doi.org/10.31128/AJGP‐COVID‐49.
- 84. Verweij EJ, M’hamdi HI, Steegers EAP, et al. Collateral damage of the COVID‐19 pandemic: a Dutch perinatal perspective. BMJ 2020; 369: m2326.
- 85. Adams C, Ridgway L, Hooker L. Maternal, child and family nursing in the time of COVID‐19: the Victorian Maternal and Child Health Service experience. Aust J Child Fam Health Nurs 2020; 17: 12–15.
- 86. Hull N, Kam RL, Gribble KD. Providing breastfeeding support during the COVID‐19 pandemic: concerns of mothers who contacted the Australian Breastfeeding Association [preprint]. medRxiv 2020; https://doi.org/10.1101/2020.07.18.20152256.
- 87. Hynan MT. Covid‐19 and the need for perinatal mental health professionals: now more than ever before. J Perinatol 2020; 40: 985–986.
- 88. Wang G, Zhang Y, Zhao J, et al. Mitigate the effects of home confinement on children during the COVID‐19 outbreak. Lancet 2020; 395: 945–947.
- 89. Prioritising children’s rights in the COVID‐19 response [editorial]. Lancet Child Adolesc Health 2020; 4: 479.
- 90. Link‐Gelles R, DellaGrotta A, Molina C, et al. Limited secondary transmission of SARS‐CoV‐2 in child care programs — Rhode Island, June 1–July 31, 2020. MMWR Morb Mortal Wkly Rep 2020; 69: 1170–1172.
- 91. McCoy DC, Cuartas J, Behrman J, et al. Global estimates of the implications of COVID‐19‐related preprimary school closures for children’s instructional access, development, learning, and economic wellbeing. Child Dev 2021; 92: e883–e899.
- 92. Baxter J. Report no. 3: Child care in 2020. Melbourne: Australian Institute of Family Studies, 2021. https://aifs.gov.au/sites/default/files/publication‐documents/2105_3_fias_child_care_in_2020.pdf (viewed July 2021).
- 93. Carroll M, Budinski M, Warren D, et al. Report no. 1: Connection to family, friends and community. Melbourne: Australian Institute of Family Studies; 2021. https://aifs.gov.au/sites/default/files/publication‐documents/2105_1_fias_connection‐to‐family‐friends‐community.pdf (viewed July 2021).
- 94. Berkman BE. Mitigating pandemic influenza: the ethics of implementing a school closure policy. J Public Health Manag Pract 2008; 14: 372–378.
- 95. Koirala A, Goldfeld S, Bowen AC, et al. Lessons learnt during the COVID‐19 pandemic: why Australian schools should be prioritised to stay open. J Paediatr Child Health 2021; 57: 1362–1369.
- 96. Christakis DA, Van Cleve W, Zimmerman FJ. Estimation of US children’s educational attainment and years of life lost associated with primary school closures during the coronavirus disease 2019 pandemic. JAMA Netw Open 2020; 3: e2028786.
- 97. Cordova‐Villalobos JA, Macias AE, Hernandez‐Avila M, et al. The 2009 pandemic in Mexico: experience and lessons regarding national preparedness policies for seasonal and epidemic influenza. Gac Med Mex 2017; 153: 102–110.
- 98. Jester BJ, Uyeki TM, Patel A, et al. 100 years of medical countermeasures and pandemic influenza preparedness. Am J Public Health 2018; 108: 1469–1472.
- 99. Ros‐DeMarize R, Chung P, Stewart R. Pediatric behavioral telehealth in the age of COVID‐19: brief evidence review and practice considerations. Curr Probl Pediatr Adolesc Health Care 2021; 51: 100949.
- 100. McNicholas F, Kelleher I, Hedderman E, et al. Referral patterns for specialist child and adolescent mental health services in the Republic of Ireland during the COVID‐19 pandemic compared with 2019 and 2018. BJPsych Open 2021; 7: e91.
- 101. Nicholas J, Bell IH, Thompson A, et al. Implementation lessons from the transition to telehealth during COVID‐19: a survey of clinicians and young people from youth mental health services. Psychiatry Res 2021; 299: 113848.
- 102. Hopcraft M, Farmer G. Impact of COVID‐19 on the provision of paediatric dental care: analysis of the Australian Child Dental Benefits Schedule. Community Dent Oral Epidemiol 2021; 49: 369–376.
- 103. Australian Government Department of Health. Immunisation coverage rates for all children. https://www.health.gov.au/health‐topics/immunisation/childhood‐immunisation‐coverage/immunisation‐coverage‐rates‐for‐all‐children (viewed July 2021).
- 104. Lazzerini M, Barbi E, Apicella A, et al. Delayed access or provision of care in Italy resulting from fear of COVID‐19. Lancet Child Adolesc Health 2020; 4: e10–e11.
- 105. Cheek JA, Craig SS, West A, et al. Emergency department utilisation by vulnerable paediatric populations during the COVID‐19 pandemic. Emerg Med Australas 2020; 32: 870–871.
- 106. Graham A, Sahlberg P. Schools are moving online, but not all children start out digitally equal. The Conversation 2020; 26 Mar. https://theconversation.com/schools‐are‐moving‐online‐but‐not‐all‐children‐start‐out‐digitally‐equal‐134650 (viewed Aug 2021).
- 107. Golberstein E, Wen H, Miller BF. Coronavirus disease 2019 (COVID‐19) and mental health for children and adolescents. JAMA Pediatr 2020; 174: 819–820.
- 108. Royal Children’s Hospital National Child Health Poll. Telehealth for kids: experiences of Australian parents. Melbourne: RCH, 2021. https://www.rchpoll.org.au/polls/telehealth‐for‐kids‐experiences‐of‐australian‐parents/ (viewed July 2021).
- 109. Australian Government Department of Social Services. Stronger Places, Stronger People. https://www.dss.gov.au/families‐and‐children‐programs‐services/stronger‐places‐stronger‐people (viewed Aug 2021).
- 110. Victorian Government Department of Premier and Cabinet. A framework for place‐based approaches. https://www.vic.gov.au/framework‐place‐based‐approaches/ (viewed Aug 2021).
- 111. Siddiqi A, Rajaram A, Miller SP. Do cash transfer programmes yield better health in the first year of life? A systematic review linking low‐income/middle‐income and high‐income contexts. Arch Dis Child 2018; 103: 920–926.
- 112. Cooper K, Stewart K. Does household income affect children’s outcomes? A systematic review of the evidence. Child Indicators Res 2021; 14: 981–1005.
- 113. The White House. Fact sheet: Biden‐Harris administration distributes first monthly payments of the expanded child tax credit. https://www.whitehouse.gov/briefing‐room/statements‐releases/2021/07/15/fact‐sheet‐biden‐harris‐administration‐distributes‐first‐monthly‐payments‐of‐the‐expanded‐child‐tax‐credit/ (viewed July 2021).
- 114. Emba C. Opinion: Biden’s child tax credit should be obvious. Yet the result is revolutionary. Washington Post 2021; 19 July. https://www.washingtonpost.com/opinions/2021/07/19/bidens‐child‐tax‐credit‐should‐be‐obvious‐yet‐result‐is‐revolutionary/ (viewed July 2021).
- 115. Cassells R, Duncan A. JobKeepers and JobSeekers: how many workers will lose and how many will gain? Bankwest Curtin Economics Centre Research Brief COVID‐19 No. 3. Perth: Curtin University, 2020. https://bcec.edu.au/assets/2020/03/BCEC‐COVID19‐Brief‐3‐Job‐Seekers‐and‐Keepers_FINAL‐1.pdf (viewed July 2021).
- 116. Phillips B, Gray M, Biddle N. COVID‐19 JobKeeper and JobSeeker impacts on poverty and housing stress under current and alternative economic and policy scenarios. Canberra: Australian National University Centre for Social Research and Methods, 2020. https://csrm.cass.anu.edu.au/sites/default/files/docs/2020/8/Impact_of_Covid19_JobKeeper_and_Jobeeker_measures_on_Poverty_and_Financial_Stress_FINAL.pdf (viewed Aug 2021).
- 117. Australian Government Department of Social Services. Family Tax Benefit. https://www.dss.gov.au/families‐and‐children/benefits‐payments/family‐tax‐benefit (viewed Oct 2021).
- 118. McDaid L, Cleary A, Robinson M, et al. Pillar 3 report: What can be done to maximise educational outcomes for children and young people experiencing disadvantage? Brisbane: University of Queensland, 2021. https://issr.uq.edu.au/files/21397/Ramsay%20Pillar%203_Final.pdf (viewed June 2021).
- 119. Friel S, Baum F, Goldfeld S, et al. How Australia improved health equity through action on the social determinants of health. Med J Aust 2021; 214 (8 Suppl): S7–S11. https://onlinelibrary.wiley.com/doi/full/https://doi.org/10.5694/mja2.51020
- 120. Victorian Department of Education. Framework for improving student outcomes (FISO 2.0). 2021 https://www2.education.vic.gov.au/pal/fiso/policy (viewed Oct 2021).
- 121. Royal Commission into Victoria’s Mental Health System. Final report: summary and recommendations. Melbourne: State of Victoria, 2021. https://finalreport.rcvmhs.vic.gov.au/wp‐content/uploads/2021/02/RCVMHS_FinalReport_ExecSummary_Accessible.pdf (viewed June 2021).
- 122. Australian Government National Mental Health Commission. National Children’s Mental Health and Wellbeing Strategy. https://www.mentalhealthcommission.gov.au/Mental‐health‐Reform/Childrens‐Mental‐Health‐and‐Wellbeing‐Strategy (viewed June 2021).
- 123. Australian Government Department of Health. National Action Plan for the Health of Children and Young People 2020–2030. Canberra: Commonwealth of Australia, 2019. https://www1.health.gov.au/internet/main/publishing.nsf/Content/4815673E283EC1B6CA2584000082EA7D/$File/FINAL%20National%20Action%20Plan%20for%20the%20Health%20of%20Children%20and%20Young%20People%202020‐2030.pdf (viewed Nov 2021).
- 124. Primary Health Reform Steering Group. Draft recommendations from the Primary Health Reform Steering Group: discussion paper to inform the development of the Primary Health Reform Steering Group recommendations on the Australian Government’s Primary Health Care 10 Year Plan. Canberra: Australian Government Department of Health, 2021 https://www.health.gov.au/sites/default/files/documents/2021/08/draft‐recommendations‐from‐the‐primary‐health‐reform‐steering‐group.pdf (viewed Nov 2021).
- 125. Yonek J, Lee CM, Harrison A, et al. Key components of effective pediatric integrated mental health care models: a systematic review. JAMA Pediatr 2020; 174: 487–98.
- 126. Australian Institute of Health and Welfare. Australia’s children (Cat. No. CWS 69). Canberra: AIHW. 2020. https://www.aihw.gov.au/getmedia/6af928d6‐692e‐4449‐b915‐cf2ca946982f/aihw‐cws‐69‐print‐report.pdf.aspx?inline=true (viewed Nov 2021).
- 127. Productivity Commission. Mental health (Report No. 95). Canberra: Commonwealth of Australia, 2020. https://www.pc.gov.au/inquiries/completed/mental‐health/report/mental‐health.pdf (viewed June 2021).
- 128. Australian Government Department of Health. Consultation draft — Primary Health Care 10 Year Plan. https://consultations.health.gov.au/primary‐care‐mental‐health‐division/draft‐primary‐health‐care‐10‐year‐plan/ (viewed Oct 2021).
- 129. Victorian Department of Health. Community health reform plan. https://www2.health.vic.gov.au/about/publications/policiesandguidelines/community‐health‐reform‐plan (viewed Oct 2021).
- 130. Royal Australasian College of Physicians. Inequities in child health: position statement. Sydney: RACP, 2018. https://www.racp.edu.au/docs/default‐source/advocacy‐library/racp‐inequities‐in‐child‐health‐position‐statement.pdf?sfvrsn=6ceb0b1a_6 (viewed Nov 2021).
- 131. Graham A, Sahlberg P. Growing Up Digital Australia: phase 2 technical report. Sydney: Gonski Institute for Education, UNSW, 2021.
- 132. World Health Organization. How to plan and conduct telehealth consultations with children and adolescents, and their families. Geneva: WHO. In press.





Summary