The known: In Australia, suicide was the leading cause of premature death of people aged 15–44 years in 2015.
The new: A brief, selective personality‐targeted intervention for 13‐year‐old high school students was associated with lower proportions of students reporting suicidal ideation three years later than of students who received a non‐selective intervention or usual school health education.
The implications: Selective personality‐targeted interventions can be effective approaches to targeting suicidal ideation in Australian school students.
Suicide prevention should be delivered early in life and be easily accessible to all in need. Many young people who experience suicidal thoughts do not seek help,5 highlighting the need for prevention outside primary care and mental health services. Preventive programs in schools could broadly reach young people, but a recent meta‐analysis found little evidence that they achieved sustained reductions in suicidal ideation and self‐harm. The authors highlighted the need for more rigorous studies.6
Targeting personality risk factors for psychopathology can efficiently modify unhelpful patterns of thinking and responses that contribute to mental ill‐health and suicide.7 Hopelessness (having negative beliefs about the future and low expectations of success) is strongly predictive of suicidal ideation and suicide,8 as is impulsivity (disinhibition, poor planning, difficulty with self‐control).9 Hopelessness and impulsivity are also implicated in depressive and substance use disorders, themselves risk factors for suicide.9
Preventure was developed as an intervention for reducing substance misuse, but treats it as one of many risky coping strategies.10 The program is delivered in schools to younger adolescents (13–15 years) with high scores for any of four personality traits associated with greater risk of mental and substance use disorders: hopelessness, anxiety sensitivity, impulsivity, and sensation seeking.7,8,9 Randomised controlled trials in the United Kingdom,7,10 Canada,11 and Australia12 undertaken by the authors and other groups have found that Preventure reduces alcohol use and problem drinking for up to three years.
Preventure applies elements of cognitive behavioural therapy effective in suicide prevention13 to encourage adolescents to engage in cognitive reappraisal and to develop adaptive strategies for coping with emotional distress. It can reduce the symptoms of depression, anxiety, and externalising psychopathology for up to three years.11 Its focus on personality‐specific cognitive distortions and identifying helpful strategies for coping with distress could also be helpful in reducing suicidal ideation.14 A preliminary United Kingdom study found that Preventure reduced suicidal ideation among adolescents for more than two years.15
In a post hoc analysis of data from a cluster randomised controlled trial of interventions for reducing alcohol misuse,16 we found that Preventure was more effective than usual school health education for reducing suicidal ideation in adolescents who had been bullied.14 In this article, we report a further post hoc analysis of data from this trial. We examined the efficacy of the selective, personality‐targeted Preventure intervention for reducing suicidal ideation in Australian adolescents, assessed up to three years after the intervention.
Methods
We analysed data collected during the Climate and Preventure (CAP) study, a four‐arm, cluster randomised controlled trial that compared the efficacy of two alcohol misuse prevention strategies (and their combination) during February 2012 – April 2015.12,16,17,18 The four arms were non‐selective (Climate Schools), selective (Preventure), and combined non‐selective and selective prevention interventions (Climate Schools and Preventure), as well as a control group (usual health education only). All students received usual health education, including drug and alcohol education required by the national curriculum. Climate Schools is an online, non‐selective drug and alcohol prevention program that consists of twelve 40‐minute lessons in cartoon storyline format; it is directed at risk factors specific to substance misuse, such as drug‐related attitudes and behaviours.19 Schools and students were not informed about the study hypotheses prior to participation, but the study was otherwise unblinded. To maximise retention, students received $10 gift cards for each survey they completed; those who completed all five surveys were entered into a draw for an iPad. We prospectively registered the CAP study (Australian and New Zealand Clinical Trials Registry, ACTRN12612000026820; 6 January 2012).
We have described recruitment for the CAP study elsewhere.12,16,17,18 In brief, 190 schools randomly selected from a list of all public and private secondary schools in Victoria and New South Wales were invited to participate in letters sent to the school principals in 2011. Twenty‐six schools agreed to participate and were block randomised to one of the four study groups. For our post hoc analysis, we combined the two RCT study arms including selective prevention as the intervention group (Preventure group) and the other two arms as the control group. As ethics guidelines prohibited assessing suicidal ideation in participating public schools, data for 1636 year 8 students in 17 non‐government schools (16 in New South Wales, one in Victoria) were included in our post hoc analysis (Box 1).
Procedures
During February–April 2012 (baseline), students completed the Substance Use Risk Profile Scale (SURPS), a 23‐item questionnaire that assesses four personality traits: hopelessness, anxiety sensitivity, impulsivity, and sensation seeking.20 The reliability and validity of SURPS is good, including in Australian adolescents.21 Students with scores more than one standard deviation above their school mean on any trait were deemed to be at elevated risk of mental health and substance use problems and allocated to the personality risk group for which their score was furthest from the mean (determined by z scores). Students whose personality trait scores indicated that they were not at elevated risk were allocated to the low risk group and were ineligible for the Preventure intervention. All students completed surveys at baseline, and follow‐up questionnaires were administered at six months, and one, two, and three years. We also collected data on the demographic characteristics of students (age, sex, country of birth).
Preventure
In post hoc intervention group schools, students allocated to a personality risk group had been invited to receive Preventure (with or without Climate Schools). As associations between personality risk subtypes and mental health and alcohol use patterns differ,11 students received the intervention in personality subtype‐based groups. Preventure included two 90‐minute small group sessions delivered one week apart during March – November 2012 by a clinical psychologist and co‐facilitator with a psychology honours degree or higher. The first session used psycho‐education to help students understand the characteristics of their personality style and to explore unhelpful coping behaviours specific to their personality risk group. They were then introduced to the cognitive behaviour model and invited to apply it to recent personal experiences, in order to understand how their thoughts and feelings shape their behaviour. The second session encouraged students to challenge personality‐specific thoughts that elicit problematic emotional and behavioural reactions. Despite not explicitly discussing suicide or self‐harm, similar strategies are effective in suicide prevention.13
Outcomes
Mental health symptoms (depression and anxiety subscales of the Brief Symptom Inventory) were defined in the CAP trial protocol as secondary outcomes.16,18 In our post hoc analysis, we examined responses to the suicidal ideation item of the CAP questionnaire, which asked how often participants had thoughts about ending their life during the preceding six months. This item was part of the depression subscale of the Brief Symptom Inventory, a scale with good test–retest reliability, internal consistency, convergent validity, and construct validity.22 The five‐point response scale ranged from “not at all” to “often”; unless the participants reported “not at all”, they were deemed to have experienced suicidal ideation. In our sample, the internal consistency over time of the suicidal ideation item was reasonable (Cronbach α = 0.73), and the threshold for experiencing suicidal ideation (ie, “ever”) is consistent with that used in population studies, such as the Australian National Survey of Mental Health and Wellbeing.23
Statistical analysis
We undertook intention‐to‐treat analyses in Stata 17 comparing the change over three years in the proportion of students in the two groups reporting suicidal ideation. We assessed the intervention effect over time in multilevel mixed logistic models, adjusted for nesting of students in schools and sex. Time was coded as a linear variable (baseline; six months; one, two, three years) and the best fitting random effects structure (Bayesian information criterion) included random intercepts at the individual and school levels and random slopes for the effect of time at the individual level (Supporting Information, table 1). All available data were included to estimate unbiased model parameters, and it was assumed that missing data were missing at random, as we found no evidence of systematic differences in missing data at follow‐up (data not shown). Full information maximum likelihood estimation was used in cases of missing data. The effect of the intervention on suicidal ideation was modelled with an intervention × time interaction term, using an independent covariance matrix selected using the Bayesian information criterion; we report odds ratios (ORs) for the intervention × time interaction, with 95% confidence intervals (CIs).
Ethics approval
The CAP study, including post hoc analyses, was approved by the human research ethics committees of the University of New South Wales (HC16881), the University of Sydney (HREC 2018/845), the Sydney Catholic Education Office (772), and the New South Wales Department of Education and Training (2011201). Parents or guardians provided consent for their children to participate in the study; students also provided consent.
Results
The baseline characteristics of the 17 schools and 1636 students are summarised in Box 2. In the post hoc intervention group, 342 students had attended at least one Preventure session (73%) and 317 (67%) two sessions. Across both post hoc analysis groups, 1569 students (96%) completed at least one follow‐up assessment, and 1474 (90%) at least two follow‐up assessments. Fifty‐one of 979 boys (5%) and 16 of 657 girls (2%) provided baseline data only. The proportions of control (25, 3%) and intervention group students (42, 5%) who did not complete follow‐up assessments were similar. Assessments were missed because students were absent from school, changed schools, or did not use identifying codes that enabled data linkage (data not shown).
Suicidal ideation: baseline assessment
At baseline (year 8), when most participants were 13 years old, 182 students in the control group (25%) and 185 in the intervention group (23%) reported suicidal ideation (Box 3). The proportion of students who had high scores for one or more personality risk factors who reported suicidal ideation (227 of 652, 35%) was higher than for students who did not (140 of 886, 16%; OR, 2.8; 95% CI, 2.2–3.6). In particular, the odds of suicidal ideation at baseline were higher for students with high scores for hopelessness (90 of 141, 64% v 277 of 1397, 20%; OR, 7.1; 95% CI, 5.0–10) or impulsivity (46 of 145, 32% v 321 of 1393, 23%; OR, 1.6; 95% CI, 1.1–2.2) than for students without high scores for these traits.
Suicidal ideation: three‐year assessment
At the three‐year follow‐up (year 11), when most students were 16 years old, 138 of 516 students in the control group (27%) and 98 of 571 students in the intervention group (17%) reported suicidal ideation. Across the three‐years of follow‐up, the annual reduction in the odds of suicidal ideation was greater for the intervention group than the control group (per year: OR, 0.80; 95% CI, 0.66–0.97; after adjusting for sex: adjusted OR, 0.82; 95% CI, 0.68–1.00).
Discussion
We found that Preventure, a brief, selective, personality‐targeted intervention (with or without a concurrent non‐selective intervention) was more effective than usual school health education (with or without a concurrent non‐selective intervention) for reducing the prevalence of reported suicidal ideation in adolescents between year 8 (baseline) and year 11 (three‐year follow‐up). Reporting of suicidal ideation by students in schools in which Preventure was offered declined, compared with the control group, by 20% per year across three years. Our hypothesis‐generating post hoc analysis suggests that the effectiveness of Preventure for reducing suicidal thoughts should be further investigated.
These findings add to the evidence that school‐based suicide prevention interventions for adolescents can be effective. One Australian study estimated that 6% of 12–15‐year‐old adolescents had seriously considered suicide during the preceding twelve months.25 The baseline prevalence of suicidal ideation was higher in our study (about 24%), but this included all who had suicide‐related thoughts, not just those who had seriously considered suicide.
Preventure achieves significant improvements in several domains of psychopathology with two brief (90‐minute) workshops.11,18 There are few evidence‐based interventions for dealing with suicidal thoughts,6 and no randomised controlled trials of other selective interventions have been reported. By targeting a subset of young people at particular risk of suicidal ideation, selective prevention typically requires fewer resources than less selective approaches. But as many young people do not seek help for suicidal thoughts, identifying and selectively intervening is challenging.5
Preventure offers a feasible approach to effectively targeting suicidal ideation, and our findings indicate that personality traits are modifiable risk factors. Further, we found longer term benefits of a school‐based intervention in preventing suicidal ideation, with a significant effect three years after the intervention, suggesting that targeting personality risk factors can achieve durable change of maladaptive thinking patterns throughout adolescence.
Among the barriers to implementing selective prevention strategies is the limited availability of qualified personnel, such as psychologists, particularly in rural areas. However, reporting of symptoms of depression, anxiety, and suicidal ideation by adolescents was reduced in a United Kingdom trial in which school teachers were trained to deliver Preventure.15
Limitations
First, as most people with suicidal ideation do not attempt suicide, suicidal ideation is not a direct measure of harm. However, it is associated with increased risk of attempting suicide;26 an analysis of World Mental Health survey data from 17 countries (2001–2003) found that 29% of people who reported suicidal ideation later attempted suicide.27 Second, the CAP trial was not powered to assess interactions between trial group and personality in post hoc subgroup analyses. Third, our analysis was restricted to non‐government schools because of ethics‐related restrictions on assessing suicidal ideation in government schools, and we tested the efficacy of Preventure in year 8 students only; further studies could include public schools and older adolescents. The representativeness of our post hoc groups was also affected by the differing sex distribution in our groups (33% boys in the control group, 83% in the intervention group; mitigated by adjusting the final model for sex), and the different proportions of the CAP study sample included in the post hoc analysis (control: 755 of 1103, 68%; intervention: 881 of 1087; 81%). One‐third of students in the intervention group did not receive Preventure in full, and 27% did not receive it at all. However, our intention‐to‐treat analysis was a strength; that is, students in the intervention group who did not receive the Preventure intervention, or did not receive it in full, were included in the analysis. Further, we did not take the severity of reported suicidal ideation into account. Finally, follow‐up concluded in 2015, and suicidal ideation in more recent times was not assessed. However, given reported changes in adolescent mental health since 2015,28 the need for a selective approach to reducing suicidality in young people has not declined.
Conclusion
Suicidal ideation in young people is a major personal and social problem. Preventure effectively modifies personality‐related risk factors for suicidal ideation in young adolescents, and its effects were evident three years after our brief intervention. Preventure is an effective and scalable school‐based intervention that can help reduce suicidal ideation in young people.
Data sharing
Considerations of participant privacy prohibit sharing of the study data.
Open access: Open access publishing facilitated by The University of Sydney, as part of the Wiley ‐ The University of Sydney agreement via the Council of Australian University Librarians.
Box 1 – Summary of participant flow through the Climate and Preventure (CAP) study: participants included in our post hoc analysis*
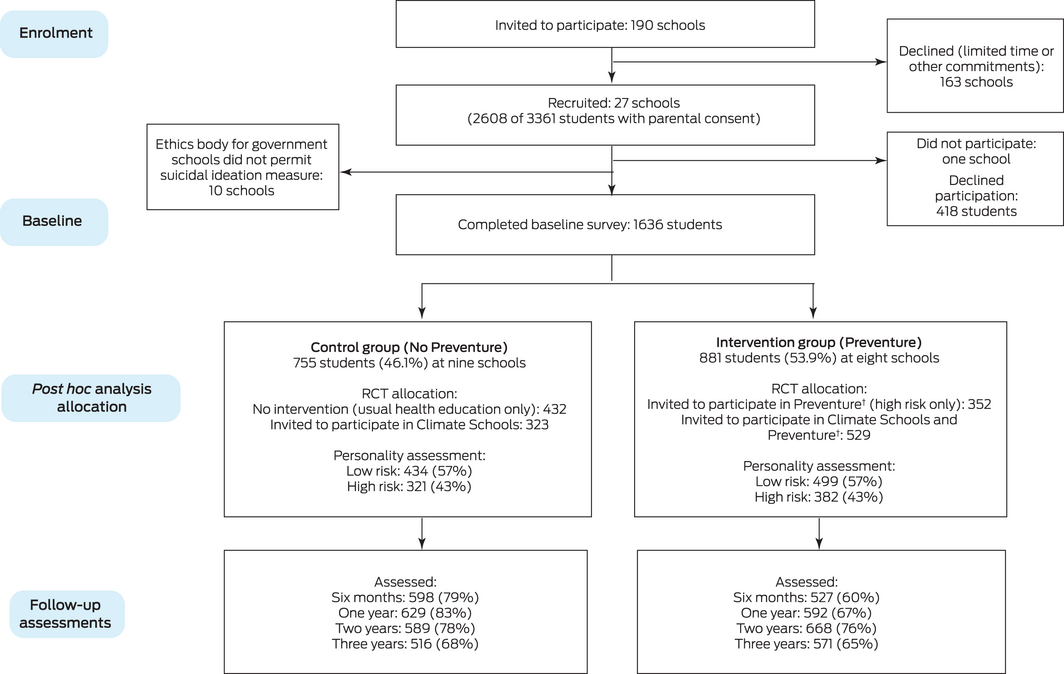
* The CONSORT diagram for the CAP randomised control trial during which the data were collected is included in the Supporting Information (figure).
† Only students with scores more than one standard deviation above their school mean on any personality trait and therefore deemed to be at elevated risk of mental health and substance use problems were invited to participate in Preventure. ◆
Box 2 – Baseline characteristics of the schools and year 8 students included in our post hoc analysis of suicidal ideation data collected during the Climate and Preventure (CAP) study
|
Characteristic |
Control group* |
Intervention group† |
|||||||||||||
|
|
|||||||||||||||
|
Schools |
9 |
8 |
|||||||||||||
|
Students per school, mean (SD) |
84 (48.3) |
110 (40.2) |
|||||||||||||
|
Location |
|
|
|||||||||||||
|
Metropolitan |
8 |
8 |
|||||||||||||
|
Rural |
1 |
0 |
|||||||||||||
|
Type of school |
|
|
|||||||||||||
|
Single sex |
7 |
7 |
|||||||||||||
|
Co‐educational |
2 |
1 |
|||||||||||||
|
Area socio‐economic status, quintile‡ |
|
|
|||||||||||||
|
1 (greatest disadvantage) |
0 |
1 |
|||||||||||||
|
2 |
3 |
0 |
|||||||||||||
|
3 |
0 |
0 |
|||||||||||||
|
4 |
0 |
2 |
|||||||||||||
|
5 (least disadvantage) |
6 |
5 |
|||||||||||||
|
Students |
755 |
881 |
|||||||||||||
|
Age (years), mean (SD) |
13.3 (0.5) |
13.2 (0.4) |
|||||||||||||
|
Sex |
|
|
|||||||||||||
|
Boys |
246 (33%) |
733 (83%) |
|||||||||||||
|
Girls |
509 (67%) |
148 (17%) |
|||||||||||||
|
Country of birth |
|
|
|||||||||||||
|
Australia |
671 (89%) |
771 (88%) |
|||||||||||||
|
Other: English‐speaking |
26 (3%) |
54 (6%) |
|||||||||||||
|
Other: not English‐speaking |
52 (7%) |
55 (6%) |
|||||||||||||
|
Missing data |
6 (1%) |
1 (< 1%) |
|||||||||||||
|
Allocated to personality risk group |
|
|
|||||||||||||
|
Yes |
321 (43%) |
382 (43%) |
|||||||||||||
|
No |
434 (57%) |
499 (57%) |
|||||||||||||
|
|
|||||||||||||||
|
SD = standard deviation. * The Climate Schools and usual health education only (control) arms of the Climate and Preventure (CAP) study.16 † The Preventure and Climate Schools and Preventure arms of the Climate and Preventure (CAP) study.16 ‡ Socio‐Economic Indexes for Areas Index of Relative Socio‐economic Disadvantage (IRSD).24 |
|||||||||||||||
Box 3 – Suicidal ideation reported by students in post hoc control and intervention groups at baseline (year 8) and in follow‐up assessments*
|
Assessment |
Control group |
Intervention group |
|||||||||||||
|
|
|||||||||||||||
|
Baseline† |
182/726 (25%) |
185/812 (23%) |
|||||||||||||
|
6 months |
143/598 (24%) |
94/527 (18%) |
|||||||||||||
|
1 year |
149/629 (24%) |
116/592 (20%) |
|||||||||||||
|
2 years |
156/589 (26%) |
131/668 (20%) |
|||||||||||||
|
3 years |
138/516 (27%) |
98/571 (17%) |
|||||||||||||
|
|
|||||||||||||||
|
* A breakdown by all four original study arms is included in the Supporting Information (table 2). † Ninety‐eight children (29 control [4%], 69 intervention [8%]) did not provide responses for the suicidal ideation item. |
|||||||||||||||
Received 6 October 2021, accepted 15 March 2022
- Lucinda R Grummitt1
- Jennifer Debenham1
- Erin Kelly1
- Emma L Barrett1
- Katrina Champion1
- Patricia Conrod2,3
- Maree Teesson1
- Nicola Newton1
- 1 The Matilda Centre for Research in Mental Health and Substance Use, University of Sydney, Sydney, NSW
- 2 University of Montreal, Montreal, Canada
- 3 Sainte Justine Hospital Research Centre, University of Montreal, Montreal, Canada
The Climate and Preventure (CAP) study was funded by the National Health and Medical Research Council (APP1004744). We acknowledge the schools, students, teachers, and research assistants who were involved in the study. We also acknowledge the assistance of the New South Wales Department of Education and Communities for access to their schools (reference, SERAP 2011201).
No relevant disclosures.
- 1. Australian Institute of Health and Welfare. Australian Burden of Disease Study: impact and causes of illness and death in Australia 2015 (Australian Burden of Disease series no. 19; Cat. no. BOD 22). Canberra: AIHW, 2019. https://www.aihw.gov.au/reports/burden‐of‐disease/burden‐disease‐study‐illness‐death‐2015 (viewed Sept 2021).
- 2. John A, Pirkis J, Gunnell D, et al. Trends in suicide during the COVID‐19 pandemic. BMJ 2020; 371: m4352.
- 3. Lifeline. More Australians than ever seeking crisis support [media release]. 4 Aug 2021. https://www.lifeline.org.au/media/yxab453i/20210804‐lifeline‐more‐australians‐than‐ever‐seeking‐support.pdf (viewed Sept 2021).
- 4. Tanaka T, Okamoto S. Increase in suicide following an initial decline during the COVID‐19 pandemic in Japan. Nat Hum Behav 2021; 5: 229‐238.
- 5. Michelmore L, Hindley P. Help‐seeking for suicidal thoughts and self‐harm in young people: a systematic review. Suicide Life Threat Behav 2012; 42: 507‐524.
- 6. Robinson J, Bailey E, Witt K, et al. What works in youth suicide prevention? A systematic review and meta‐analysis. EClinicalMedicine 2018; 4‐5: 52‐91.
- 7. Castellanos N, Conrod P. Brief interventions targeting personality risk factors for adolescent substance misuse reduce depression, panic and risk‐taking behaviours. J Ment Health 2006; 15: 645‐658.
- 8. O’Connor RC, Nock MK. The psychology of suicidal behaviour. Lancet Psychiatry 2014; 1: 73‐85.
- 9. Gvion Y, Apter A. Suicide and suicidal behavior. Public Health Rev 2012; 34: 9.
- 10. Conrod PJ, Castellanos‐Ryan N, Mackie C. Personality‐targeted interventions delay the growth of adolescent drinking and binge drinking. J Child Psychol Psychiatry 2008; 49: 181‐190.
- 11. Conrod PJ. Personality‐targeted interventions for substance use and misuse. Curr Addict Rep 2016; 3: 426‐436.
- 12. Newton NC, Conrod PJ, Slade T, et al. The long‐term effectiveness of a selective, personality‐targeted prevention program in reducing alcohol use and related harms: a cluster randomized controlled trial. J Child Psychol Psychiatry 2016; 57: 1056‐1065.
- 13. Stanley B, Brown G, Brent DA, et al. Cognitive‐behavioral therapy for suicide prevention (CBT‐SP): treatment model, feasibility, and acceptability. J Am Acad Child Adolesc Psychiatry 2009; 48: 1005‐1013.
- 14. Kelly EV, Newton NC, Stapinski LA, et al. A novel approach to tackling bullying in schools: personality‐targeted intervention for adolescent victims and bullies in Australia. J Am Acad Child Adolesc Psychiatry 2020; 59: 508‐518.e2.
- 15. O’Leary‐Barrett M, Topper L, Al‐Khudhairy N, et al. Two‐year impact of personality‐targeted, teacher‐delivered interventions on youth internalizing and externalizing problems: a cluster‐randomized trial. J Am Acad Child Adolesc Psychiatry 2013; 52: 911‐920.
- 16. Newton NC, Teesson M, Barrett EL, et al. The CAP study, evaluation of integrated universal and selective prevention strategies for youth alcohol misuse: study protocol of a cluster randomized controlled trial. BMC Psychiatry 2012; 12: 118.
- 17. Teesson M, Newton NC, Slade T, et al. Combined universal and selective prevention for adolescent alcohol use: a cluster randomized controlled trial. Psychol Med 2017; 47: 1761‐1770.
- 18. Newton NC, Stapinski L, Teesson M, et al. Evaluating the differential effectiveness of social influence and personality‐targeted alcohol prevention on mental health outcomes among high‐risk youth: a novel cluster randomised controlled factorial design trial. Aust N Z J Psychiatry 2019; 54: 259‐271.
- 19. Newton NC, Teesson M, Vogl LE, Andrews G. Internet‐based prevention for alcohol and cannabis use: final results of the Climate Schools course. Addiction 2010; 105: 749‐759.
- 20. Woicik PB, Stewart SH, Pihl RO, Conrod P. The Substance Use Risk Profile Scale: a scale measuring traits linked to reinforcement‐specific substance use profiles. Addict Behav 2009; 32: 1042‐1055.
- 21. Newton NC, Barrett EL, Castellanos‐Ryan N, et al. The validity of the Substance Use Risk Profile Scale (SURPS) among Australian adolescents. Addictive Behav 2016; 53: 23‐30.
- 22. Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med 1983; 13: 595‐605.
- 23. Johnston AK, Pirkis JE, Burgess PM. Suicidal thoughts and behaviours among Australian Adults: findings from the 2007 National Survey of Mental Health and Wellbeing. Aust N Z J Psychiatry 2009; 43: 635‐643.
- 24. Australian Bureau of Statistics. 2033.0.55.001. Census of Population and Housing: Socio‐Economic Indexes for Areas (SEIFA), Australia, 2016. IRSD interactive map. 27 Mar 2018. https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/2033.0.55.001~2016~Main%20Features~IRSD%20Interactive%20Map~15 (viewed Sept 2021).
- 25. Lawrence D, Johnson S, Hafekost J, et al. The mental health of children and adolescents. Report on the second Australian Child and Adolescent Survey of Mental Health and Wellbeing. Aug 2015. https://www.health.gov.au/sites/default/files/documents/2020/11/the‐mental‐health‐of‐children‐and‐adolescents_0.pdf (viewed Dec 2021).
- 26. Slade T, Johnston A, Oakley Browne MA, et al. 2007 National Survey of Mental Health and Wellbeing: methods and key findings. Aust N Z J Psychiatry 2009; 43: 594‐605.
- 27. Nock MK, Borges G, Bromet EJ, et al. Cross‐national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry 2008; 192: 98‐105.
- 28. Keyes KM, Gary D, O’Malley PM, et al. Recent increases in depressive symptoms among US adolescents: trends from 1991 to 2018. Soc Psychiatry Psychiatr Epidemiol 2019; 54: 987‐996.






Abstract
Objective: To assess the efficacy of a selective, personality‐targeted intervention for reducing suicidal ideation in adolescents.
Design:Post hoc analysis of survey data collected in the Climate and Preventure (CAP) study, a cluster randomised controlled trial that compared strategies for reducing alcohol misuse by adolescents, 2012–2015.
Setting, participants: Year 8 students at 16 New South Wales non‐government schools and one Victorian non‐government school.
Intervention: Preventure, a selective, personality‐targeted intervention designed to help adolescents with personality risk factors for alcohol misuse, comprising two 90‐minute sessions, one week apart. For ourpost hoc analysis, we combined data from the two CAP trial groups in which Preventure was offered (the Preventure and the Preventure/Climate Schools [a non‐selective prevention strategy] groups) as the intervention group; and data from the two groups in which Preventure was not offered (usual health education only [control] and Climate Schools groups) as the control group.
Main outcome measure: Difference betweenpost hoc control and intervention groups in the change in proportions of students reporting suicidal ideation during the preceding six months (single item of Brief Symptom Inventory depression subscale) over three years.
Results: A total of 1636 students (mean age at baseline, 13.3 years; standard deviation, 0.5 years) were included in our analysis, of whom 1087 (66%) completed the suicidal ideation item in the three‐year follow‐up assessment. Thepost hoc control group included 755 students (nine schools), the intervention group 881 students (eight schools). After adjusting for nesting of students in schools and sex, reporting of suicidal ideation by students who had received Preventure had declined over three years, compared with the control group (per year: adjusted odds ratio, 0.80; 95% CI, 0.66–0.97).
Conclusion: Personality‐targeted selective prevention during early secondary school can have a lasting impact on suicidal ideation during adolescence.
Trial registration (CAP study only): Australian and New Zealand Clinical Trials Registry, ACTRN12612000026820 (prospective).