The known: COVID‐19‐related morbidity and mortality are reported to be lower for children than adults.
The new: A total of 393 children with SARS‐CoV‐2 infections presented to 16 participating Australian hospitals during February‒September 2020. Fifty‐one of the 426 presentations (12%) led to hospital admissions (44 children). Two children developed paediatric inflammatory multisystem syndrome temporally associated with SARS‐CoV‐2 (PIMS‐TS).
The implications: The clinical course for most children positive for SARS‐CoV‐2 was mild. Ambulatory monitoring or hospital in the home may be effective strategies for reducing the numbers of presentations and admissions to hospital of children with COVID‐19.
Coronavirus disease 2019 (COVID‐19)‐related morbidity and mortality are reported to be lower for children than adults.1 Proposed explanations include age‐related differences in clotting function, angiotensin‐converting enzyme 2 receptors, antibodies to other coronaviruses, and in innate and adaptive immune function.2,3 Severe disease is more frequent in infants than in older children, and in children with other medical conditions or elevated levels of the inflammatory marker, C‐reactive protein.4 Concerns have been expressed since the beginning of the COVID‐19 pandemic that the numbers of hospitalisations, critical care admissions, and deaths of children with comorbid conditions were high, but the situation is unclear.5,6 Of particular concern is the paediatric inflammatory multisystem syndrome temporally associated with SARS‐CoV‐2 (PIMS‐TS), or multisystem inflammatory syndrome,7 a complication reported in settings with high rates of community transmission.8,9 One of the first large multicentre studies to report this condition described 78 children in the United Kingdom with considerable short term critical care needs; two patients died.8
In Australia, the first case of COVID‐19 was reported in late January 2020.10 Following the relatively brief first wave, a second COVID‐19 outbreak from June 2020 culminated in a prolonged lockdown in Victoria, before case numbers declined by late September 2020. To this point, about 3649 people aged 19 years or younger had tested positive for the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) in Australia,11 the first in early February, a child reported to have travelled overseas.12 From mid‐March, positive test results were reported for children in Victoria, but the first patients had mild symptoms and did not require hospital admission.13
A 2020 study in a tertiary Victorian hospital identified overseas travel and contact with someone known to be SARS‐CoV‐2‐positive as risk factors for children.13 We have undertaken a multicentre study to examine the epidemiological and clinical characteristics of children positive for SARS‐CoV‐2 in Australia.
Methods
We conducted a multicentre retrospective study of children (under 18 years of age) who presented to COVID‐19 testing clinics, emergency departments, or wards in participating hospitals, for whom positive results were recorded during 1 February – 30 September 2020.
All 30 members of the Emergency Departments International Collaborative (PREDICT) research network14 were invited to participate. We aimed to recruit one tertiary hospital in each mainland state outside Victoria and to include as many active research sites in Victoria as possible. Hospitals that responded and could complete the ethics and governance application and data extraction were included in our study.
At each participating hospital, investigators obtained from their laboratories lists of children with positive SARS‐CoV‐2 test results and undertook retrospective chart reviews to check their eligibility for our study. We included all children who met the Paediatric Active Enhanced Disease Surveillance (PAEDS) case definition for PIMS‐TS and for whom there was evidence of SARS‐CoV‐2 exposure.15
SARS‐CoV‐2 was detected in oropharynx or nasopharynx (or deep nasal area) specimens by reverse transcription polymerase chain reaction, according to Australian guidelines.16
De‐identified medical records data — demographic characteristics, presenting symptoms and history, epidemiological risk factors (overseas travel and known contact with people with confirmed SARS‐CoV‐2 infections), other medical conditions, examination findings, laboratory results, imaging findings, and clinical outcomes — were entered into a standardised case reports form in a REDCap database, hosted at the Murdoch Children’s Research Institute, Melbourne. Prior to data entry, data abstractors were trained and data was entered into a training database and checked to ensure consistency in data entry between sites.17
Statistical analysis
We included all available data in our analyses. We summarise data for continuous variables as medians with interquartile ranges (IQRs) or numbers and proportions, as appropriate. Risk differences (RDs) with 95% confidence intervals (CI) were calculated. Data analyses were undertaken in Stata IC 16.0.
Ethics approval
Central ethics approval was provided by the Royal Children’s Hospital (Melbourne) Human Research Ethics Committee (HREC63071/RCHM‐2020); institutional approval was provided by the human research ethics committee at each participating site.
Results
Sixteen hospitals in five states provided data for our analysis: eleven in Victoria, two in New South Wales, and one each in Queensland, Western Australia, and South Australia; seven were major paediatric tertiary centres (Box 1). A total of 393 SARS‐CoV‐2‐positive children (including 181 girls, 46%) and 426 presentations were recorded by the participating hospitals, including 131 presentations to emergency departments (31%). The median age of the children was 5.3 years (IQR, 1.9–12.0 years; range, 10 days to 17.9 years); twelve were three months old or younger (3%), including five neonates. Eight children were Aboriginal or Torres Strait Islander Australians (2%); the Indigenous status of twelve was unknown (3%).
The first positive case was dated 3 February 2020. Thirty‐three children presented more than once (8%): 27 presented twice, three presented three times, one presented four times, and two were transferred to participating tertiary centres. Forty‐four children were admitted to hospital (11%; 51 presentations, 12%), including two diagnosed with PIMS‐TS (0.5%).
Epidemiological risk factors
A total of 288 children had known contact with people with confirmed SARS‐CoV‐2 infections (73%), 85 had no known contact (22%), and this information was not available for 21 children (5%). Of those with known contacts, the contact was a household member in 199 cases (69%), and 43 were close contacts of infected persons identified at their schools or in childcare (15%). Of the 72 children for whom details about the contact were available, 29 had developed COVID‐19 symptoms one day or more after the most recent contact (40%; median, 4 days [IQR, 1–7 days; range, 1–15 days]). Overseas travel was reported for ten children (3%) (Box 2).
Clinical characteristics
Most children had symptoms consistent with COVID‐19 at the time of their first positive swab (235 of 378, 62%), 143 were asymptomatic (38%), and this information was unavailable for 15 children. For the children with symptoms, the median time from onset to testing was two days (IQR, 1‒4 days). Seventeen asymptomatic children subsequently developed symptoms (12%; after a median of two days [IQR, 0–2 days]), 98 remained asymptomatic (69%), and this information was unavailable for 28 children. The most frequent symptoms (at presentation or subsequently) were fever (159 of 337, 47%), stuffy or runny nose (151 of 216, 70%), and cough (146 of 229, 64%) (Box 2). Four neonates presented with non‐specific lethargy as their only symptom.
Emergency department presentations
Most of the 131 presentations to emergency departments (by 112 children) were to two Victorian hospitals: the Royal Children’s (55, 44%) and Sunshine Hospitals (43, 33%); there were only five emergency department presentations outside Victoria. Nineteen presentations were second or later presentations within 14 days of the first (5%), only four of which led to hospital admissions. Compared with patients who presented to testing clinics, larger proportions of children who presented to emergency departments were under 12 months of age or had other medical conditions (Supporting Information, table 1).
The median emergency department length of stay was 2.4 hours (IQR, 1.1‒3.7 hours). In 97 cases, the child was discharged directly home (73%), in 26 they were admitted to a hospital ward (20%; including one admitted to the paediatric intensive care unit), in one they were admitted to hospital in the home (2%), and in seven they were observed for up to 12 hours (6%). Reasons for hospital admission were hydration problems (12 presentations), persistent fever (five), lethargy (five), social reasons (five), respiratory problems (three), and parental anxiety (two). COVID‐19 was not suspected at four presentations to two hospitals (diagnoses: cyclical vomiting, soft tissue abscess, and two neonates with lethargy and reduced feeding); the children were tested for SARS‐CoV‐2 only after admission to hospital. Hospital medical interventions were not required for 115 of 131 emergency department presentations (88%) (Supporting Information, table 2).
Children admitted to hospital
Fifty‐one of 426 presentations (by 44 children) led to hospital admissions (12%), including 17 hospital in the home admissions; none of the patients managed by hospital in the home subsequently presented to a participating hospital. However, only 16 of these 426 presentations required hospital medical interventions (4%). Seven hospitalised infants required intravenous antibiotics to guard against bacterial sepsis, but all cultures were negative. The demographic features, clinical characteristics, and epidemiological risk factors for hospitalised and non‐hospitalised patients were similar (Box 2). Three presentations led to admissions to paediatric intensive care units (two children with PIMS‐TS, and one with congenital cardiac disease and severe COVID‐19); two of these patients were transferred from the presenting hospital to tertiary centres. One child diagnosed with PIMS‐TS required extracorporeal membrane oxygenation; the second did not require respiratory or inotropic support, and was treated with intravenous immunoglobulins and observed in a paediatric intensive care unit. One neonate tested positive in a neonatal intensive care unit after being admitted for reasons unrelated to COVID‐19; they did not require medical treatment for COVID‐19. All hospitalised children subsequently recovered and were discharged from hospital.
Discussion
Our findings highlight the stark difference in COVID‐19 burden across five Australian states during February‒September 2020. The eleven participating Victorian hospitals reported 399 presentations by SARS‐CoV‐2‐positive people under 18 years of age, while the five large tertiary centres in four other states reported fewer than ten cases each. Only 4% of children who presented to hospitals required medical interventions, similar to overseas reports.18 Only three children were critically unwell, including two who developed PIMS‐TS, one of whom required invasive therapy. This low number is consistent with reported temporal and geographic associations between community SARS‐CoV‐2 prevalence and numbers of PIMS‐TS cases.19 More than half the patients in our study were 5 years old or younger. This may reflect limited testing of younger children in the community or parents preferring to take their young children to hospital for testing. Our data also indicate that children with SARS‐CoV‐2 infections present with symptoms similar to those of other common viral illnesses in children. There were few differences between the characteristics of hospitalised and non‐hospitalised children, and many may have been admitted as a precautionary measure.
Factors reported to predict the severity of COVID‐19 include very young age, comorbid conditions, and elevated C‐reactive protein (CRP) values.4 We did not find these associations in our study. For example, only seven of the 12 infants (0–3 months old), including five neonates, had been hospitalised. Some comorbid conditions were more frequent in hospitalised patients, but the differences were not marked (Box 2). Laboratory investigations were undertaken for fewer than half the hospitalised patients; in contrast to other studies,4 CRP levels were not markedly higher at presentation in those who required respiratory support or critical care (Supporting Information, table 2). Nine children in our study underwent chest radiography (2%). High rates of chest radiography (35% of children with COVID‐19) and computed tomography (2%) were reported by an Italian multicentre study, but only 9% of the included patients required respiratory support.20
Given the increased transmissibility of newer SARS‐CoV‐2 variants, including the Delta (B.1.617.2) variant now circulating in Australia, and our finding that 31% of presentations by SARS‐CoV‐2‐positive children were to emergency departments, continuing vigilance with regard to infection prevention is critical.21 Whether vaccination can contain the transmission of new variants remains to be established.22,23 Grouping patients in the emergency department into high and low risk categories according to their symptoms may provide false reassurance; for example, COVID‐19 was not suspected in four SARS‐CoV‐2‐positive children in our study, including two neonates with lethargy, who presented to emergency departments at the height of the Victorian epidemic.
Thirty‐three children known to be SARS‐CoV‐2‐positive presented to hospitals more than once (8%), many of whom did not require hospital admission. Providing families with details of a health service that could remotely monitor and manage people with COVID‐19, as established in some jurisdictions earlier in the epidemic,24 could avert repeated emergency department visits and the associated risks. Home or ambulatory monitoring was available for about 4% of the patients in our study, at three participating hospitals in Melbourne, Gold Coast, and Adelaide.
Limitations
Our study was the first collaborative investigation by several large Australian centres in the PREDICT network. Limitations included the fact that the data were collected retrospectively, although this was mitigated by following guidelines for high quality medical records review.25 Further, the service delivery model for COVID‐19 testing and case management differed between health services. Some hospitals did not report COVID‐19 screening clinic data, as the clinics were organisationally distinct from the hospitals. However, we included at least one hospital from each state that reported both emergency department and screening clinic data. We did not collect data on longer term outcomes, which should be the subject of further studies.
Conclusion
We present multicentre data on COVID‐19 in children in Australia, particularly Victoria, the state with the largest number of cases during the study period. The clinical course for most SARS‐CoV‐2‐positive children who presented to hospital was mild and they did not require hospital medical interventions. Ambulatory monitoring or hospital in the home may be effective as strategies for reducing the numbers of presentations and admissions to hospital by children with COVID‐19. Infants who present with non‐specific lethargy should be flagged for testing for SARS‐CoV‐2.
Box 1 – Participating hospitals and numbers of SARS‐CoV‐2‐positive children
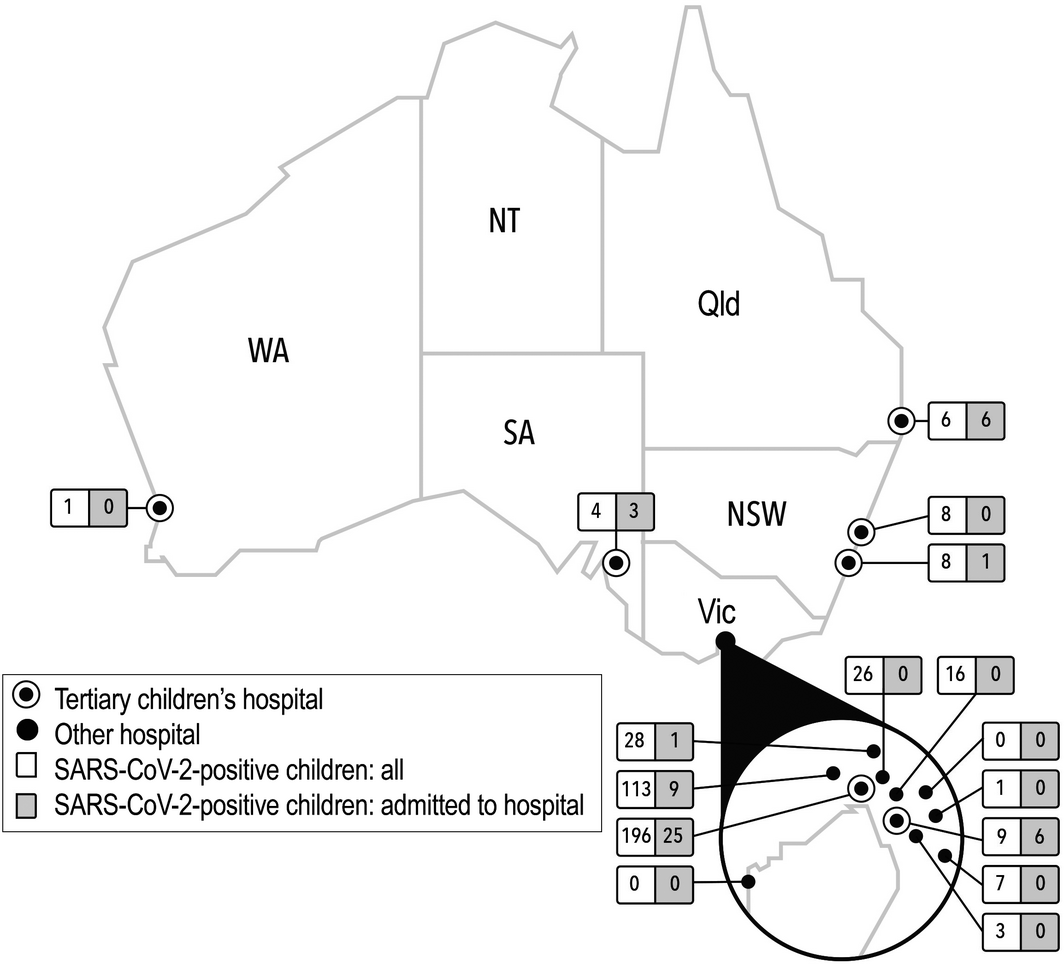
Participating hospitals: Royal Children’s Hospital Melbourne, Sunshine Hospital (Western Health), Northern Hospital, Austin Hospital, Monash Medical Centre Clayton (Monash Health), Casey Hospital (Monash Health), Dandenong Hospital (Monash Health), Box Hill Hospital (Eastern Health), Angliss Hospital (Eastern Health), Maroondah Hospital (Eastern Health), University Hospital Geelong (Barwon Health) (Victoria); John Hunter Hospital (Hunter New England Health), Children’s Hospital at Westmead (New South Wales); Gold Coast University Hospital (Queensland); Perth Children’s Hospital (Western Australia); Women’s and Children’s Hospital (South Australia).
Box 2 – Characteristics of the 393 SARS‐CoV‐2‐positive children who presented to participating hospitals, by need for hospitalisation
|
Characteristic |
All children |
Hospitalised |
Not hospitalised |
Risk difference (percentage points) (95% CI) |
|||||||||||
|
|
|||||||||||||||
|
Number of patients |
393 |
44 [11%] |
349 [89%] |
— |
|||||||||||
|
Number of presentations |
426 |
51 [12%] |
375 [88%] |
— |
|||||||||||
|
Sex (girls) |
181 (46%) |
21 (48%) |
160 (46%) |
–0.02 (–0.14 to 0.18) |
|||||||||||
|
Age |
|
|
|
|
|||||||||||
|
< 12 months |
52 (13%) |
9 (20%) |
43 (11%) |
0.08 (–0.04 to 0.21) |
|||||||||||
|
1‒5 years |
158 (40%) |
12 (27%) |
146 (42%) |
–0.15 (–0.29 to –0.00) |
|||||||||||
|
6‒10 years |
72 (18%) |
10 (23%) |
62 (18%) |
0.05 (–0.08 to 0.18) |
|||||||||||
|
> 10 years |
111 (28%) |
13 (30%) |
98 (28%) |
0.01 (–0.13 to 0.16) |
|||||||||||
|
Epidemiological risk factors |
|
|
|
|
|||||||||||
|
Contact with SARS‐CoV‐2‐positive person |
288 (73%) |
32 (69%) |
256 (78%) |
–0.08 (–0.23 to 0.06) |
|||||||||||
|
Overseas travel in past 14 days |
10 (3%) |
6 (14%) |
4 (2%) |
0.12 (–0.02 to 0.23) |
|||||||||||
|
Symptoms/signs: at time of swab |
|
|
|
|
|||||||||||
|
Any symptom/sign |
235/378 (62%) |
32/43 (74%) |
203/335 (61%) |
‒0.14 (‒0.28 to 0.00) |
|||||||||||
|
None |
143/378 (38%) |
11/43 (26%) |
132/335 (39%) |
–0.14 (–0.28 to 0.00) |
|||||||||||
|
Symptoms/signs: any time |
|
|
|
|
|||||||||||
|
Any symptom/sign |
252/350 (72%) |
33/42 (79%) |
219/308 (71%) |
–0.07 (–0.06 to 0.21) |
|||||||||||
|
None |
98/350 (28%) |
9/42 (21%)* |
89/308 (29%) |
–0.07 (–0.06 to 0.21) |
|||||||||||
|
Fever (> 37.5°C) |
159/337 (47%) |
23/42 (55%) |
136/295 (46%) |
0.09 (–0.07 to 0.25) |
|||||||||||
|
Stuffy/runny nose |
149/216 (70%) |
16/30 (53%) |
133/186 (72%) |
–0.18 (–0.37 to 0.01) |
|||||||||||
|
Cough |
146/229 (64%) |
15/33 (45%) |
131/196 (67%) |
–0.21 (–0.40 to –0.03) |
|||||||||||
|
Sore throat |
65/200 (33%) |
8/30 (27%) |
57/170 (34%) |
–0.07 (–0.24 to 0.10) |
|||||||||||
|
Headache |
37/252 (15%) |
6/33 (18%) |
31/219 (14%) |
0.04 (–0.10 to 0.18) |
|||||||||||
|
Difficulty breathing |
18/196 (9%) |
6/31 (19%) |
12/165 (7%) |
0.12 (–0.02 to 0.27) |
|||||||||||
|
Muscle ache |
14/252 (6%) |
2/33 (6%) |
12/219 (5%) |
0.01 (–0.08 to 0.09) |
|||||||||||
|
Diarrhoea |
14/252 (6%) |
3/33 (9%) |
11/219 (5%) |
0.04 (–0.06 to 0.14) |
|||||||||||
|
Anosmia |
5/252 (2%) |
1/33 (3%) |
4/219 (2%) |
0.01 (–0.05 to 0.07) |
|||||||||||
|
Comorbid conditions |
|
|
|
|
|||||||||||
|
Any condition |
60/312 (19%) |
13/44 (30%) |
47/268 (18%) |
0.12 (–0.02 to 0.26) |
|||||||||||
|
Asthma |
25/306 (8%) |
2/42 (5%) |
23/264 (9%) |
–0.04 (–0.11 to 0.03) |
|||||||||||
|
Immunosuppression/malignancy |
4/304 (1%) |
2/43 (5%) |
2/261 (1%) |
0.04 (–0.02 to 0.10) |
|||||||||||
|
Prematurity |
6/303 (2%) |
2/43 (5%) |
4/260 (2%) |
0.03 (–0.03 to 0.10) |
|||||||||||
|
Heart disease |
8/304 (3%) |
2/43 (5%) |
6/261 (2%) |
0.02 (–0.04 to 0.09) |
|||||||||||
|
Diabetes mellitus |
2/304 (0.7%) |
1/43 (2%) |
1/261 (0.4%) |
0.02 (–0.03 to 0.07) |
|||||||||||
|
Cerebral palsy |
1/302 (0.3%) |
1/42 (2%) |
0/260 |
0.02 (–0.02 to 0.07) |
|||||||||||
|
Renal disease |
0 |
0 |
0 |
— |
|||||||||||
|
None reported |
252/312 (81%) |
31/44 (70%) |
221/268 (82%) |
0.12 (–0.02 to 0.26) |
|||||||||||
|
|
|||||||||||||||
|
CI = confidence interval. * Nine children were admitted to hospital but did not develop symptoms attributed to COVID‐19: hospital in the home monitoring in anticipation of symptoms developing (four), urinary tract infection (one), testicular pain (one), social reasons for admission (three). |
|||||||||||||||
Received 13 April 2021, accepted 3 June 2021
- Laila F Ibrahim1,2
- Doris Tham1,3
- Vimuthi Chong4
- Mark Corden5
- Simon Craig6,7
- Paul Buntine8,9
- Shefali Jani10,11
- Michael Zhang12
- Shane George13,14
- Amit Kochar15
- Sharon O’Brien16,17
- Karen Robins‐Browne18
- Shidan Tosif1,2
- Andrew Daley1,2
- Sarah McNab1,2
- Nigel W Crawford1,2
- Catherine Wilson1
- Franz E Babl1,2
- 1 Murdoch Children’s Research Institute, Melbourne, VIC
- 2 University of Melbourne, Melbourne, VIC
- 3 Western Health, Melbourne, VIC
- 4 Austin Hospital, Melbourne, VIC
- 5 Northern Hospital Epping, Melbourne, VIC
- 6 Monash Health, Melbourne, VIC
- 7 Monash University, Melbourne, VIC
- 8 Eastern Health, Melbourne, VIC
- 9 Box Hill Hospital, Melbourne, VIC
- 10 The Children’s Hospital at Westmead, Sydney, NSW
- 11 The University of Sydney, Sydney, NSW
- 12 John Hunter Hospital, Newcastle, NSW
- 13 Gold Coast University Hospital, Gold Coast, QLD
- 14 The University of Queensland Child Health Research Centre, Brisbane, QLD
- 15 Women’s and Children’s Hospital, Adelaide, SA
- 16 Perth Children’s Hospital, Perth, WA
- 17 Curtin University, Perth, WA
- 18 University Hospital Geelong, Geelong, VIC
This study was unfunded, but was supported by a National Health and Medical Research Council (NHMRC) Centre of Research Excellence grant for paediatric emergency medicine (GNT1171228) and the Victorian Government Infrastructure Support Program. The participation of Franz Babl was partly funded by an NHMRC Practitioner Fellowship (GNT1124466) and by the Royal Children’s Hospital Foundation. Laila Ibrahim was supported by a Clinician‐Scientist Fellowship from the Murdoch Children’s Research Institute.
We acknowledge the staff who assisted with data retrieval: Visakan Krishnananthan and Caoimhe Basquille (emergency medicine, Eastern Health); Rebecca Gormley (Sunshine Hospital, Western Health); Gaby Nieva (Women’s and Children’s Hospital, Adelaide); and Rebecca Hughes (Royal Children’s Hospital Melbourne).
No relevant disclosures.
- 1. Lavezzo E, Franchin E, Ciavarella C, et al; Imperial College COVID‐19 Response Team. Suppression of a SARS‐CoV‐2 outbreak in the Italian municipality of Vo’. Nature 2020; 584: 425–429.
- 2. Neeland MR, Bannister S, Clifford V, et al. Innate cell profiles during the acute and convalescent phase of SARS‐CoV‐2 infection in children. Nat Commun 2021; 12: 1084.
- 3. Zimmermann P, Curtis N. Why is COVID‐19 less severe in children? A review of the proposed mechanisms underlying the age‐related difference in severity of SARS‐CoV‐2 infections. Arch Dis Child 2021; 106: 429–439.
- 4. Graff K, Smith C, Silveira L, et al. Risk factors for severe COVID‐19 in children. Pediatr Infect Dis J 2021; 40: e137–e145.
- 5. Shekerdemian LS, Mahmood NR, Wolfe KK, et al; International COVID‐19 PICU Collaborative. Characteristics and outcomes of children with coronavirus disease 2019 (COVID‐19) infection admitted to US and Canadian pediatric intensive care units. JAMA Pediatr 2020; 40: e137–e145.
- 6. Alfraij A, Bin Alamir AA, Al‐Otaibi AM, et al. Characteristics and outcomes of coronavirus disease 2019 (COVID‐19) in critically ill pediatric patients admitted to the intensive care unit: a multicenter retrospective cohort study. J Infect Public Health 2020; 14: 193–200.
- 7. Jiang L, Tang K, Levin M, et al. COVID‐19 and multisystem inflammatory syndrome in children and adolescents. Lancet Infect Dis 2020; 20: e276–e288.
- 8. Davies P, Evans C, Kanthimathinathan HK, et al. Intensive care admissions of children with paediatric inflammatory multisystem syndrome temporally associated with SARS‐CoV‐2 (PIMS‐TS) in the UK: a multicentre observational study. Lancet Child Adolesc Health 2020; 4: 669–677.
- 9. Cheung EW, Zachariah P, Gorelik M, et al. Multisystem inflammatory syndrome related to COVID‐19 in previously healthy children and adolescents in New York City. JAMA 2020; 324: 294–296.
- 10. 2019‐nCoV National Incident Room Surveillance Team. 2019‐nCoV acute respiratory disease, Australia. Epidemiology Report 1. Reporting week 26 January – 1 February 2020. Commun Dis Intell (2018) 2020; 44: https://doi.org/10.33321/cdi.2020.44.13.
- 11. COVID‐19 National Incident Room Surveillance Team. COVID‐19 Australia: Epidemiology Report 26. Fortnightly reporting period ending 27 September 2020. Commun Dis Intell (2018) 2020; 44: https://doi.org/10.33321/cdi.2020.44.78.
- 12. COVID‐19 National Incident Room Surveillance Team. COVID‐19, Australia: Epidemiology Report 2 (Reporting week ending 19:00 AEDT 8 February 2020). Commun Dis Intell (2018). 2020; 44: https://doi.org/10.33321/cdi.2020.44.14.
- 13. Ibrahim LF, Tosif S, McNab S, et al. SARS-CoV‐2 testing and outcomes in the first 30 days after the first case of COVID‐19 at an Australian children’s hospital. Emerg Med Australas 2020; 32: 801–808.
- 14. Babl FE, Krieser D, Oakley E, Dalziel S. A platform for paediatric acute care research. Emerg Med Australas 2014; 26: 419–422.
- 15. Paediatric Active Enhanced Disease Surveillance. Surveillance and research: PIMS‐TS. https://www.paeds.org.au/web/our-work/surveillance-and-research (viewed June 2021).
- 16. Australian Department of Health. Coronavirus disease 2019 (COVID‐19). CDNA national guidelines for public health units. Updated 24 June 2021. https://www1.health.gov.au/internet/main/publishing.nsf/Content/cdna-song-novel-coronavirus.htm (viewed June 2021).
- 17. Gilbert EH, Lowenstein SR, Koziol‐McLain J, et al. Chart reviews in emergency medicine research: where are the methods? Ann Emerg Med 1996; 27: 305–308.
- 18. Dong Y, Mo X, Hu Y, et al. Epidemiology of COVID‐19 among children in China. Pediatrics 2020; 145: e20200702.
- 19. Bassareo PP. Pediatric inflammatory multisystem syndrome temporally associated with SARS‐CoV‐2 (PIMS‐TS) in the United Kingdom and Ireland: what is new? Lancet Reg Health Eur 2021; 3: 100090.
- 20. Parri N, Lenge M, Cantoni B, et al; CONFIDENCE Research Group. COVID‐19 in 17 Italian pediatric emergency departments. Pediatrics 2020; 146: e20201235.
- 21. Kidd M, Richter A, Best A, et al. S‐variant SARS‐CoV‐2 lineage B1.1.7 is associated with significantly higher viral loads in samples tested by ThermoFisher TaqPath RT‐qPCR. J Infect Dis 2021; 223: 1666–1670.
- 22. Planas D, Bruel T, Grzelak L, et al. Sensitivity of infectious SARS‐CoV‐2 B.1.1.7 and B.1.351 variants to neutralizing antibodies. Nat Med 2021; 27: 917–924.
- 23. Madhi SA, Baillie V, Cutland CL, et al; NGS‐SA Group; Wits‐VIDA COVID Group. Efficacy of the ChAdOx1 nCoV‐19 Covid‐19 vaccine against the B.1.351 variant. N Engl J Med 2021; 384: 1885–1898.
- 24. The Royal Children’s Hospital Melbourne. Wallaby: Hospital‐in-the‐Home. COVID‐19 resources. https://www.rch.org.au/wallaby/COVID-19_resources (viewed June 2021).
- 25. Kaji AH, Schriger D, Green S. Looking through the retrospectoscope: reducing bias in emergency medicine chart review studies. Ann Emerg Med 2014; 64: 292–298.





Abstract
Objectives: To examine the epidemiological and clinical characteristics of SARS‐CoV‐2‐positive children in Australia during 2020.
Design, setting: Multicentre retrospective study in 16 hospitals of the Paediatric Research in Emergency Departments International Collaborative (PREDICT) network; eleven in Victoria, five in four other Australian states.
Participants: Children aged 0‒17 years who presented to hospital‐based COVID‐19 testing clinics, hospital wards, or emergency departments during 1 February ‒ 30 September 2020 and who were positive for SARS‐CoV‐2.
Main outcome measures: Epidemiological and clinical characteristics of children positive for SARS‐CoV‐2.
Results: A total of 393 SARS‐CoV‐2‐positive children (181 girls, 46%) presented to the participating hospitals (426 presentations, including 131 to emergency departments [31%]), the first on 3 February 2020. Thirty‐three children presented more than once (8%), including two who were transferred to participating tertiary centres (0.5%). The median age of the children was 5.3 years (IQR, 1.9‒12.0 years; range, 10 days to 17.9 years). Hospital admissions followed 51 of 426 presentations (12%; 44 children), including 17 patients who were managed remotely by hospital in the home. Only 16 of the 426 presentations led to hospital medical interventions (4%). Two children (0.5%) were diagnosed with the paediatric inflammatory multisystem syndrome temporally associated with SARS‐CoV‐2 (PIMS‐TS).
Conclusion: The clinical course for most SARS‐CoV‐2‐positive children who presented to Australian hospitals was mild, and did not require medical intervention.