An approach for reframing palliative care has been designed to help improve the wellbeing of people with serious illness
Most Australians can expect to die as the result of a chronic illness. The Lancet Commission on palliative care and pain relief estimated that annually, more than 61 million people experience chronic health conditions associated with suffering that could be significantly ameliorated through palliative care.1 Given the increasing incidence of chronic illness, the role of palliative care, including its availability earlier in the course of an illness, will become increasingly prominent in health care across the world.1,2,3
Modern palliative care, originally framed as “hospice care”, began in the 1960s, with the term “palliative care” adopted from the 1970s.4 Since then, palliative care has changed its focus from institutionally delivered hospice care for oncology patients to a broader purview encompassing care of patients suffering any serious illness from point of diagnosis and delivered at any site including home, hospice, residential aged care or hospital. There is also an increasing and proactive approach to early integration for improving quality of life.4 This follows a robust body of evidence demonstrating the benefits of early access to palliative care for patients, their family caregivers and the health care budget.5
Despite this, palliative care is too often considered, in the minds of both health care providers and the public, as exclusively about death and dying, and associated with a loss of control or abandoning of hope.6,7,8,9 This has significant negative consequences, including that many people are missing out on the benefits that palliative care can offer.
In addressing such misconceptions, we describe as a first step, the development of a framework to be used by our health service to help promote understanding of, and access to, palliative care. We also briefly highlight the definitional issues underpinning the rationale for such a framework and outline the steps required for systematic change.
Definition of palliative care and related terms
Arguably the most widely cited and accepted definition of palliative care is from the World Health Organization, which emphasises involvement of palliative care early in the illness course.4,10 However, there are numerous other definitions of palliative care, including those created by various organisations and jurisdictions and incorporating a varied scope of practice.11 These definitional changes are further compromised by using variable terms with different application across international settings, such as “advanced disease”, “life‐limiting illness”, “end of life” and “progressive disease”. Nearly three decades after the World Health Organization first defined palliative care, we seem to be no closer to agreeing on what the term actually means.12
Based on a review of definitions4 and palliative care standards in numerous countries, there seems to be a broad consensus that palliative care is:
- delivered by a suitably qualified multidisciplinary team;
- focused on quality of life of the patient and their family (including bereavement);
- holistic in nature (physical, emotional, existential and social);
- available to people of all ages and across a range of diagnoses or illnesses; and
- delivered across multiple care sites including hospital, home and residential aged care.
While there is less consensus around the precise timing for introducing palliative care, evidence suggests it should not be restricted to the final months of life (end of life). Rather, the benefits are evident for upstreaming palliative care much earlier in the illness.5
The implications of lack of definitional clarity
The language used to describe palliative care is important,13 having significant implications for the care of people living with serious illness. Despite the mature, established evidence base for palliative care integration early in the course of illness (including for those still receiving curative treatment), palliative care tends to remain associated in the minds of both health care providers and the public as exclusively end of life care. This creates a failure in our health care system to present palliative care earlier in the disease trajectory as a highly beneficial holistic complementary approach. Instead, when conceived as synonymous with death and dying, there may be fear and refusal of this service by patients, resulting in poorer health outcomes.4,6
Should palliative care be renamed?
For the public and health professionals alike, palliative care has an identity crisis leading many to ask “why don’t we just change its name?”. The most frequently proposed change is to “supportive care”.4 However more than 10 different definitions of supportive care have already been identified, with wide variations in focus from symptom management during cancer treatment to survivorship care.4 It also appears that renaming of individual palliative care services may only lead to short term increases in referral rates.4
Thus, changing the name seems neither practical nor necessary,2 and only likely to cause increased confusion.4 Moreover, “Patients are not interested in the name … but in what we do, how compassionate we are, how well we communicate and whether we demonstrate concern for their relatives”.14 While fearful of the term “palliative care”,15 when made aware of its core activities, patients, families and community alike are keen to avail themselves of this form of care.13 It therefore seems there are opportunities to reframe how palliative care is presented,8 rather than overhaul what it is named. Creative and consistent approaches to the framing of palliative care are required to help health professionals describe palliative care to those who may benefit from access to this care.
There are also significant issues associated with access to specialist palliative care in Australia. Furthermore, it seems that much of the palliative care delivered is restricted to end of life care, commonly the last weeks or months. This is at odds with evidence supporting earlier integration of palliative care. A reframing of palliative care, based on its core activities and practices, simultaneously highlights the opportunity — indeed the necessity — within current resources for the delivery of palliative care to be “everyone’s business”.5 For example, aspects of symptom relief or exploring preferences for care can be delivered by primary care teams or generalist providers. Hence, the responsibility for providing palliative care is not solely that of palliative care specialists (whose input should focus on more complex needs) but is a task of all health providers.5 A reframing of palliative care must reflect this.
Our proposed framing of palliative care
Given this background, we sought to:
- agree on an operational definition of palliative care for use in our own clinical tertiary hospital setting;
- create a conceptual framework to underpin accessing of palliative care; and
- develop key messages that could be used by our health service and its health care professionals to describe palliative care to those who may benefit.
To achieve this, we assembled a lead group of local senior palliative care clinicians and academics to review the literature related to palliative care definitional issues along with online resources of key professional and non‐government organisations in the field. We then convened a workshop comprising invited multidisciplinary health care professionals, consumers, a communications consultant, and a director of philanthropic funding. From this process, a framework evolved by consensus and was subject to further iterative development, arriving at the content for use within our hospital (Box 1 and Box 2).
Conclusion
Palliative care is an essential component of the goal of universal quality health coverage.12 We have argued that a name change is not required but that attention should instead focus on how palliative care is framed. A national public palliative care education campaign in Australia is required.17 We have set out one framework to help inform this in our own health service, in an attempt to locally influence the manner in which we talk about and conceptualise palliative care. While other models framing palliative care have been put forward,18 we suggest our framework explicitly highlights the ways palliative care may be integrated to complement treatment intention, respond to varying prognoses, and facilitate a response to patient and family needs throughout the care process. Nevertheless, our approach has its limitations and will require subsequent work to refine and adapt it in a way that gathers further evidence and ensures it is acceptable to a broader range of health services. Importantly, application of the framework will require a response to the individual needs and preferences of patients and family carers.
While the implementation of an effective framework can open the door to palliative care, poor service experience can also close it.2 To change the landscape, the quality of palliative care service delivery must match the promise of outcomes from consistent and evidence‐based care. Naming and characterising the three access points to palliative care (Box 2) could assist in the development of a more standardised approach to entry criteria for specialist palliative care support, with triggers specific to a person’s illness. Ultimately, this may foster better understanding of the minimum standard of palliative care expected from both specialist and generalist health care providers at each entry point.
Palliative care, effectively delivered, can restore choice regarding options for care in serious illness,13 improve a sense of control and independence, and provide peace of mind that patients and families cherish.2 When coupled with investment in public education, training, research and integration of palliative care principles earlier in an illness, the reframing of palliative care could bring us much closer to the goal of standardised high quality care for all people facing serious illness, and their families.
Box 1 – Framing palliative care and key messages
Operational definition of palliative care
We adopted elements of the World Health Organization definition10 into our set of working statements and understandings. Our operational definition of palliative care is:
- Comprehensive support for people diagnosed with a serious health condition. This support focuses on what is important to the person and their quality of life, not only their physical concerns but also emotional, social and spiritual needs. Care is delivered by the person’s main health care providers in partnership, as required, with palliative care specialists. Support is available at any stage of a serious illness including in conjunction with curative treatment, and in any setting. Support is also extended to the person’s family caregiver(s) ensuring they access the help they need to support their loved one while also maintaining their own wellbeing.
To help guide health professionals, to complement our operational definition, we specified that access to palliative care may be considered at three points (Box 2). In addition, patient and family needs for care will prompt integration at any point in the illness:
- Early palliative care (“Death is possible”). The main intent is typically curative or life‐prolonging (disease‐modifying) treatment, but palliative care staff may be involved for symptom management and explaining future palliative care involvement, should this be required.
- Mid‐stage palliative care (“Death is probable”). Clinicians would not be surprised if the person died in the foreseeable future (ie, months ahead). The main focus is therefore a palliative approach, although a number of people will be receiving disease‐modifying treatments.
- Late‐stage palliative care (“Death is imminent”). The person will likely die soon (ie, within days or weeks). The focus is therefore entirely end of life care.
To assist the health service and its health professionals describe palliative care concepts to patients, family carers and the community, we developed the following key messages:
- Palliative care is centred around you. The health care system can be complex and confusing; palliative care fits into your needs, your beliefs, your wishes, and your aims for your life. Then, you get to choose your way forward, informed by people who genuinely care.
- Palliative care enables you to be prepared. Regardless of your disease stage or prognosis, palliative care helps you explore your expectations for the future and promotes prospects of peace and dignity.
- Everyone deserves palliative care. Palliative care is “enhanced care” that focuses on you and your family. It is sometimes misunderstood but will one day be available to everyone automatically as the gold standard of best practice care.
- Palliative care is creative. Being based on your needs and those of your family, palliative care is flexible and responsive. In this way, palliative care can assist a sense of achievement and hopefulness by helping you realise and achieve your goals.
Box 2 – Framework for contemporary integrated palliative care
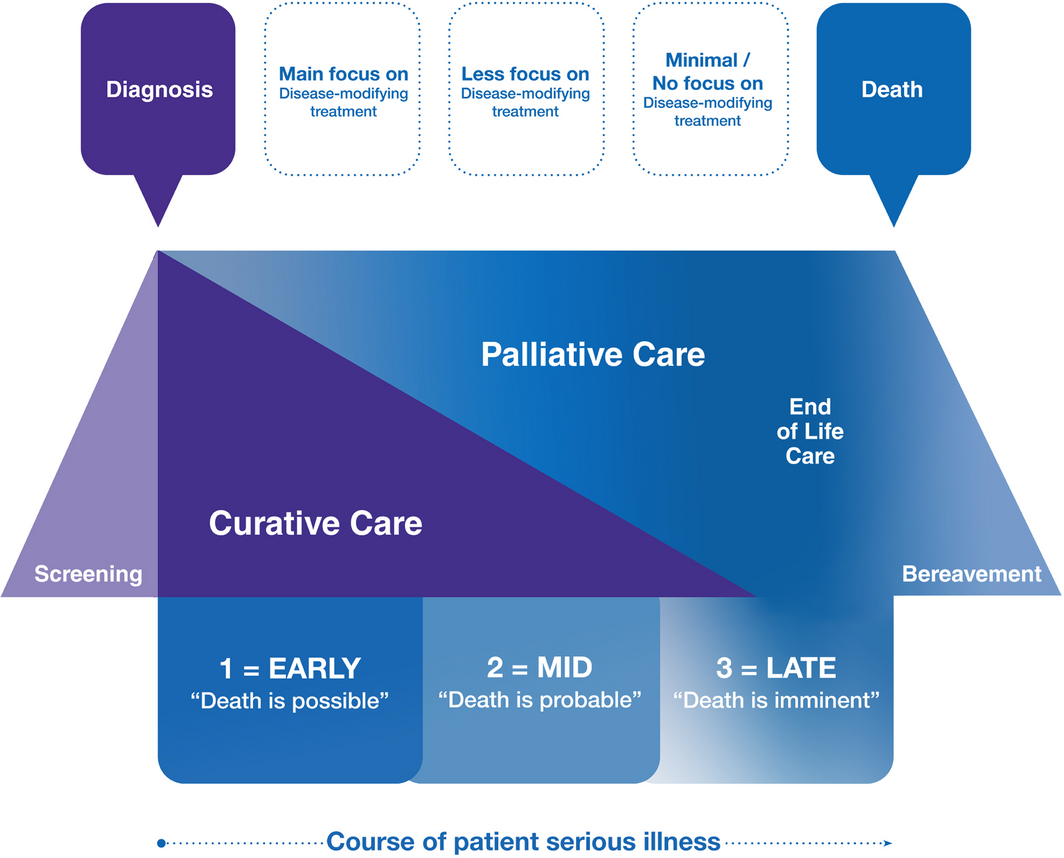
Adapted with permission from Myatra et al.16
Provenance: Not commissioned; externally peer reviewed.
- 1. Knaul FM, Farmer PE, Krakauer EL, et al. Alleviating the access abyss in palliative care and pain relief‐an imperative of universal health coverage: the Lancet Commission report. Lancet 2018; 391: 1391–1454.
- 2. Berry LL, Castellani R, Stuart B. The branding of palliative care. J Oncol Pract 2016; 12: 48–50.
- 3. Patel P, Lyons L. Examining the knowledge, awareness, and perceptions of palliative are in the general public over time: a scoping literature review. Am J Hosp Palliat Care 2020; 37: 481–487.
- 4. Ryan S, Wong J, Chow R, Zimmermann C. Evolving definitions of palliative care: upstream migration or confusion? Curr Treat Options Oncol 2020; 21: 20.
- 5. Pereira J, Chasen MR. Early palliative care: taking ownership and creating the conditions. Curr Oncol 2016; 23: 367–370.
- 6. Caprio AJ. Palliative care: renaming as supportive care and integration into comprehensive cancer care. CMAJ 2016; 188: 711–712.
- 7. Collins A, McLachlan SA, Philip J. Initial perceptions of palliative care: an exploratory qualitative study of patients with advanced cancer and their family caregivers. Palliat Med 2017; 31: 825–832.
- 8. Collins A, McLachlan SA, Philip J. Community knowledge of and attitudes to palliative care: a descriptive study. Palliat Med 2020; 34: 245–252.
- 9. Zimmermann C, Swami N, Krzyzanowska M, et al. Perceptions of palliative care among patients with advanced cancer and their caregivers. CMAJ 2016; 188: E217–E227.
- 10. World Health Organization. National cancer control programmes: policies and managerial guidelines, 2nd ed. Geneva: WHO, 2002. https://apps.who.int/iris/handle/10665/42494 (viewed July 2020).
- 11. Doyle D. The world of palliative care: one man’s view. J Palliat Care 2003; 19: 149–158.
- 12. Boyd K, Moine S, Murray SA, et al. Should palliative care be rebranded? BMJ 2019; 364: l881.
- 13. Collins A, McLachlan SA, Hill M, et al. A randomised phase II trial testing the acceptability and feasibility of a narrative approach to public health communication to increase community engagement with palliative care. Palliat Med 2020; 34: 1108–1117.
- 14. Doyle D. Proposal for a new name as well as having the new WHO definition of palliative care. Palliat Med 2003; 17: 9–10.
- 15. Collins A, McLachlan SA, Philip J. Communication about palliative care: a phenomenological study exploring patient views and responses to its discussion. Palliat Med 2018; 32: 133–142.
- 16. Myatra SN, Salins N, Iyer S, et al. End‐of‐life care policy: an integrated care plan for the dying: a joint position statement of the Indian Society of Critical Care Medicine (ISCCM) and the Indian Association of Palliative Care (IAPC). Indian J Crit Care Med 2014; 18: 615–635.
- 17. Swerissen H, Duckett SJ. What can we do to help Australians die the way they want to? Med J Aust 2015; 202: 10–11. https://www.mja.com.au/journal/2015/202/1/what‐can‐we‐do‐help‐australians‐die‐way‐they‐want
- 18. Hawley PH. The bow tie model of 21st century palliative care. J Pain Symptom Manage 2014; 47: e2–e5.






We thank Andrew Hollo (Director and Principal Consultant, Workwell) for facilitating the workshop underpinning the reframing project. We also thank the following people for attending and contributing to the workshop: Christine Elmer (General Manager, Media and Communication, St Vincent’s Hospital, Melbourne); Richard Prentice (Senior Manager, Philanthropy, St Vincent’s Hospital, Melbourne); Kirsten Rodger (General Manager, Residential Aged Care, Palliative Care and Correctional Health Services, St Vincent’s Hospital, Melbourne); Lyn Amy (CEO, St Vincent’s Health Foundation); Philippa McIlroy (Group Mission Integration Manager, Formation, Ethics and Modern Slavery, St Vincent’s Hospital, Melbourne); Kathryn Riddell (Chief Nursing Officer, St Vincent’s Hospital, Melbourne); Richard Thayer (Fundraising Manager, St Vincent’s Hospital, Melbourne); and Wendy Benson, Terence Maher and Graham Johnson (consumer representatives).
No relevant disclosures.