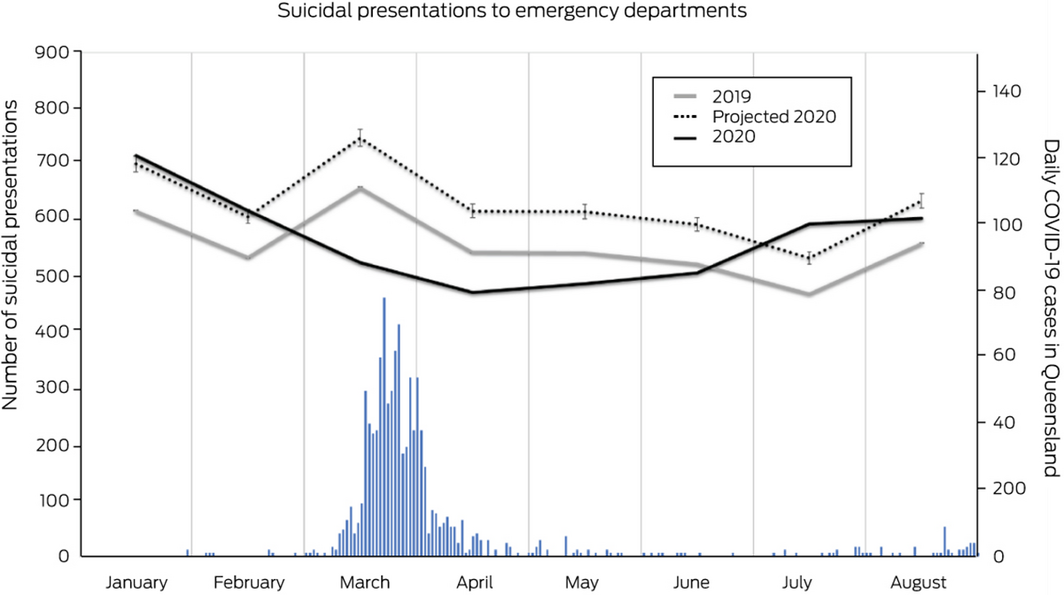
To the Editor: The coronavirus disease 2019 (COVID‐19) pandemic has raised concerns of a subsequent increase in suicides,1 but limited empirical data are available on this topic.2,3 We analysed numbers of suicidal presentations (including suicidal ideation, non‐suicidal self‐injury and suicide attempts) to emergency departments (EDs) within the Gold Coast Hospital and Health Service before and since the spread of COVID‐19 in Queensland, Australia. Cases were identified from ED administrative data through relevant diagnoses, presenting problems and keywords, followed by a manual investigation of triage narratives to exclude false positive cases, such as non‐deliberate injuries or poisonings. The numbers of ED visits between January and August 2020 were compared with the projected numbers, calculated by applying an annual increase of 13.5%4 to presentations during the same period in 2019.
From March 2020 onwards, a marked divergence between observed and projected numbers is noted, corresponding to the oscillations in the numbers of diagnosed COVID‐19 cases in Queensland (Box). At the peak of the pandemic, the reductions in suicidal presentations were the largest (29.8% in March and 23.6% in April 2020). Over the next 2 months, daily numbers of diagnosed COVID‐19 cases remained low and the difference between observed and projected numbers gradually narrowed (20.8% in May and 14.6% in June 2020). In July 2020, observed numbers exceeded projected numbers by 11.4%, but then declined again in August 2020, coinciding with another resurgence of COVID‐19. Between March and August 2020, the Gold Coast Hospital and Health Service had 554 less suicidal presentations than expected.
The well documented negative impact of COVID‐19 on all aspects of society, including mental health,5 suggests that a substantial reduction of suicide risk during this time is unlikely. Instead, our results may reflect changes in help‐seeking behaviour, with fewer people willing to seek help for suicidality through in‐hospital consultations due to fears of contracting COVID‐19.6 Ongoing promotion of telehealth and enabling safe hospital presentations or alternatives to ED7 is therefore needed to prevent the adverse outcomes of the COVID‐19 pandemic due to delayed access to care.
Limitations of this work include potential underestimations of suicidal presentations due to coding issues8 and the inability to differentiate between types of suicidal presentations.
- 1. Gunnell D, Appleby L, Arensman E, et al. Suicide risk and prevention during the COVID‐19 pandemic. Lancet Psychiatry 2020; 7: 468–471.
- 2. Calderon‐Anyosa RJC, Kaufman JS. Impact of COVID‐19 lockdown policy on homicide, suicide, and motor vehicle deaths in Peru. Prev Med 2021; 143: 106331.
- 3. Smalley CM, Malone DA, Meldon SW, et al. The impact of COVID‐19 on suicidal ideation and alcohol presentations to emergency departments in a large healthcare system. Am J Emerg Med 2020; https://doi.org/10.1016/j.ajem.2020.05. [Epub ahead of print].
- 4. Stapelberg NJ, Sveticic J, Hughes I, Turner K. Suicidal presentations to emergency departments in a large Australian public health service over 10 years. Int J Environ Res Public Health 2020; 17: 5920.
- 5. Pfefferbaum B, North CS. Mental health and the Covid‐19 pandemic. N Engl J Med 2020; 383: 510–512.
- 6. Metzler B, Siostrzonek P, Binder RK, et al. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID‐19: the pandemic response causes cardiac collateral damage. Eur Heart J Cardiovasc Pharmacother 2020; 41: 1852–1853.
- 7. Paton F, Wright K, Ayre N, et al. Improving outcomes for people in mental health crisis: a rapid synthesis of the evidence for available models of care. Health Technol Assess 2016; 20: 1–162.
- 8. Sveticic J, Stapelberg NC, Turner K. Suicidal and self‐harm presentations to emergency departments: the challenges of identification through diagnostic codes and presenting complaints. Health Inf Manag 2020; 49: 38–46.





No relevant disclosures.