Characterising the care requirements of patients with coronavirus disease 2019 (COVID‐19) is essential for resource allocation.1 Knowledge of care needs is based predominantly on experience in regions where health care capacity has been strained, and may not reflect ideal practice.2,3
We therefore examined COVID‐19 testing data for South Australia, the care requirements of patients with confirmed COVID‐19, and the disposition of people with potential COVID‐19 who presented to the designated COVID‐19 hospital for SA, the Royal Adelaide Hospital (RAH), during a period of low COVID‐19 prevalence and limited community transmission (30 January – 26 April 2020). We analysed SA Pathology data on tests for severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) and other respiratory pathogens, and clinical data from hospital electronic health records (further details: online Supporting Information). The Central Adelaide Local Health Network Human Research Ethics Committee approved the study, and waived the requirement for patient consent (reference, 13091).
Of 52 883 people tested in SA for SARS‐CoV‐2, 438 had polymerase chain reaction (PCR)‐confirmed infections (0.8%); their median age was 54 years (interquartile range [IQR], 31–64 years; range, 1–94 years), and 211 were female (48%). The median age of screened people with negative results was 43 years (IQR, 28–60 years; range, 0–104 years), of whom 30 380 were female (58%). Seventeen people with confirmed COVID‐19 (3.9%) and 7588 of those without COVID‐19 (14%) were also positive for another respiratory pathogen (Supporting Information, table 1). There were no cases of COVID‐19 among people in high care nursing facilities or prisons, nor among homeless people; one infection of a health care worker caring for people with COVID‐19 was recorded in Adelaide.
The number of patients admitted to the RAH with COVID‐19 broadly paralleled that of new cases in SA, but intensive care unit (ICU) occupancy peaked (6/7 April) and the number of people screened in the RAH emergency department for COVID‐19 declined (from 17 April) after the peak in new cases (21 March) (Box 1). The median time from diagnosis to viral clearance (according to national guidelines4) was 15 days (IQR, 12–19 days); it was lower for people managed in the community (14 days; IQR, 11–17 days) than for those admitted to hospital (17 days; IQR, 13–22 days), and there were no sex‐ or age‐related differences (data not shown).
A total of 285 people with confirmed COVID‐19 (227 aged 18–65 years; 58 over 65 years) were managed entirely in the community (Box 2); their age and sex distributions were similar to those of all SARS‐CoV‐2‐positive people (data not shown).
Of 18 228 patients who presented to the RAH emergency department, 2327 (12.8%) met screening criteria for potential COVID‐19, of whom 120 (5.2%) proved to be SARS‐CoV‐2‐positive (new diagnoses in 19 people) (Supporting Information, figure). Among people who met the criteria for potential COVID‐19, a larger proportion of people with positive results than of those with negative results arrived by private vehicle (59 [49%] v 797 [36%]), and smaller proportions required resuscitation (one [0.8%] v 72 [3%]) or had conditions deemed imminently life‐threatening (14 [12%]) v 706 [32%]); among people over 65 years, two of 37 SARS‐CoV‐2‐positive people (5%) and 406 of 939 SARS‐CoV‐2‐negative people (43%) required resuscitation or emergency review. Most people with confirmed infections were admitted to the inpatient COVID‐19 unit (90 [75%] v 419 with negative results [19%]), while three SARS‐CoV‐2‐positive (2%) and 79 SARS‐CoV‐2‐negative people (4%) were admitted from the emergency department to the ICU (Supporting Information, table 2). One of 18 228 people who presented to the ED did not meet screening criteria for potential COVID‐19 but subsequently tested positive (screening failure rate, 0.005%).
A total of 536 patients were admitted to the inpatient COVID‐19 unit, including 117 who were SARS‐CoV‐2‐positive (22%). The proportion of SARS‐CoV‐2‐positive patients aged 18–65 years was larger than for other patients in the COVID‐19 unit (84 [72%] v 188 patients [45%]); the proportions of women were similar (53 [45%] v 186 patients [44%]). Median length of stay was longer for SARS‐CoV‐2‐positive than for SARS‐CoV‐2‐negative patients over 65 years of age (182 h; IQR, 87–285 h v 96 h; IQR, 48–158 h), but was similar for all patients aged 18–65 years. Six SARS‐CoV‐2‐positive (18%) and five SARS‐CoV‐2‐negative patients over 65 (2%) were transferred from the COVID‐19 unit to the ICU (Supporting Information, table 3).
Seventeen patients hospitalised with COVID‐19 (14%) were admitted to the ICU. The median time from hospital to ICU admission was 2.4 days (IQR, 1.8–3.4 days) for the eight patients over 65, and 5.2 days (IQR, 1.0–6.1 days) for the nine aged 18–65 years; the median ICU stay was 17.3 days (IQR, 3.0–29.3 days) for those over 65, and 2.2 days (IQR, 1.6–4.4 days) for those aged 18–65 years. Four patients died (24%), the only COVID‐19‐related deaths in South Australia (overall case fatality, 0.9%; 18–65 years, 0.3%; over 65 years, 3.2%) (Supporting Information, table 4). Over the past 14 years, 15% of RAH patients with viral pneumonia in intensive care died, with a medium length of stay of 6.2 days (18–65 years, 7.4 days; over 65 years, 4.8 days) (unpublished data).
More modest, but persistent, prevalence of COVID‐19 is expected to follow the major pandemic wave of 2020. Our data, gathered in an environment of low community transmission and a health care system with considerably greater capacity than demand, reflects the COVID‐19‐related resource burden that might be anticipated as we prepare for living with COVID‐19.
Box 1 – New confirmed cases of COVID‐19 in South Australia, numbers of inpatients with COVID‐19 in the Royal Adelaide Hospital, and numbers of people presenting with potential COVID‐19 infection to the Royal Adelaide Hospital emergency department, 30 January – 26 April 2020
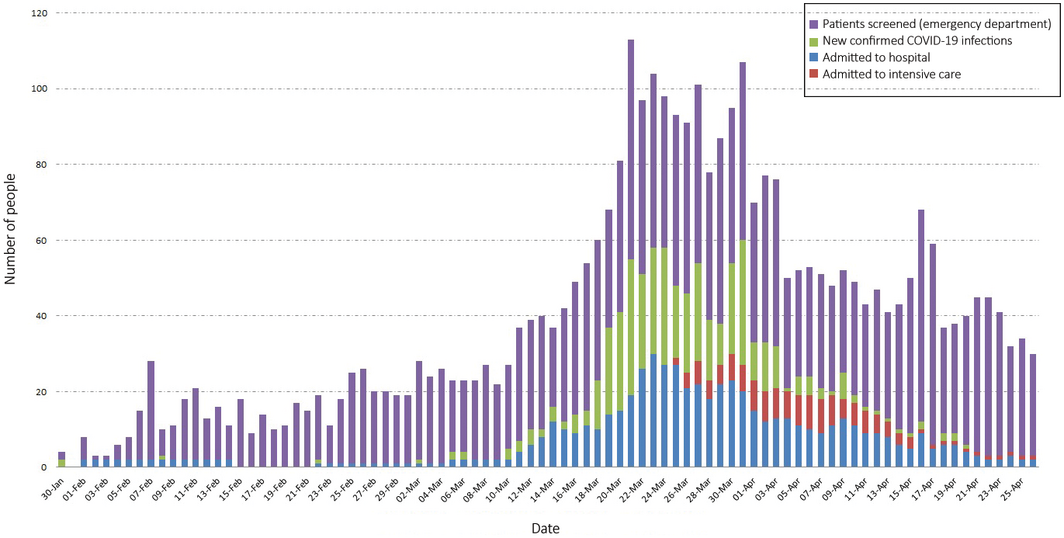
COVID‐19 = coronavirus disease 2019.
Box 2 – Care requirements of people with confirmed COVID‐19 admitted to the Royal Adelaide Hospital, 30 January – 26 April 2020
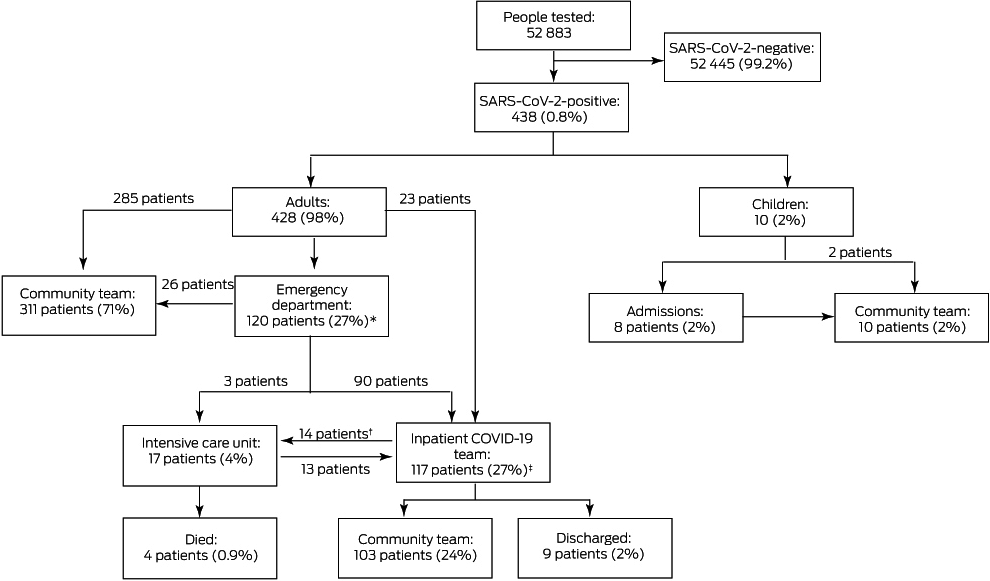
COVID‐19 = coronavirus disease 2019; SARS‐CoV‐2 = severe acute respiratory syndrome coronavirus 2.
* Includes one patient initially admitted under a non‐COVID‐19 inpatient team. † Fourteen SARS‐CoV‐2‐positive patients admitted under the COVID‐19 inpatient team required transfer to the intensive care unit, 11 of whom returned to the COVID‐19 inpatient team, as did two of three patients admitted to the intensive care unit from the emergency department. These patients are counted in both intensive care unit and COVID‐19 inpatient team numbers. ‡ includes three intensive care unit patients admitted directly from the emergency department then transferred to the inpatient team, and one patient who was still an inpatient at the end of the study.
Received 9 June 2020, accepted 10 March 2021
- 1. Adalja AA, Toner E, Inglesby TV. Priorities for the US health community responding to COVID‐19. JAMA 2020; 323: 1343–1344.
- 2. Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS‐CoV‐2 pneumonia in Wuhan, China: a single‐centered, retrospective, observational study. Lancet Respir Med 2020; 8: 475–481.
- 3. Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID‐19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA 2020; 323: 1545–1546.
- 4. Communicable Diseases Network Australia. Coronavirus disease 2019 (COVID‐19). CDNA national guidelines for public health units, version 1.0. 23 Jan 2020. https://www1.health.gov.au/internet/main/publishing.nsf/Content/cdna-song-novel-coronavirus.htm (viewed May 2020).





No relevant disclosures.