In response to the coronavirus disease 2019 (COVID‐19) outbreak in early 2020, a public health order was enacted in March 2020 that required all people arriving in New South Wales from overseas to quarantine for fourteen days.1 To manage the process and minimise the risk of community transmission, all people who arrived from 16 March 2020 were accommodated in 30 temporarily re‐purposed hotels in inner Sydney and the central business district. People with identified acute or ongoing health care needs were referred to the Royal Prince Alfred (RPA) Virtual Hospital, including those who tested positive for the severe acute respiratory syndrome coronavirus 2 (SARS CoV‐2), and were housed in three Special Health Accommodation hotels to facilitate remote monitoring of their symptoms and signs according to the RPA Virtual Hospital model of care.2 Analysis of the characteristics of these patients will inform the public health and hospital response to COVID‐19 and ensure a patient‐centred approach to health services for quarantined people.
We undertook a retrospective study of emergency department (ED) presentations by patients referred from Special Health Accommodation hotels in Sydney during 1 June – 30 September 2020. We analysed clinical characteristics and outcomes recorded in electronic medical records, including diagnosis categories, comorbid conditions, and ED length of stay. Our study was approved by the Sydney Local Health District Research Ethics Committee (references, X20‐0365; 2020/ETH02007).
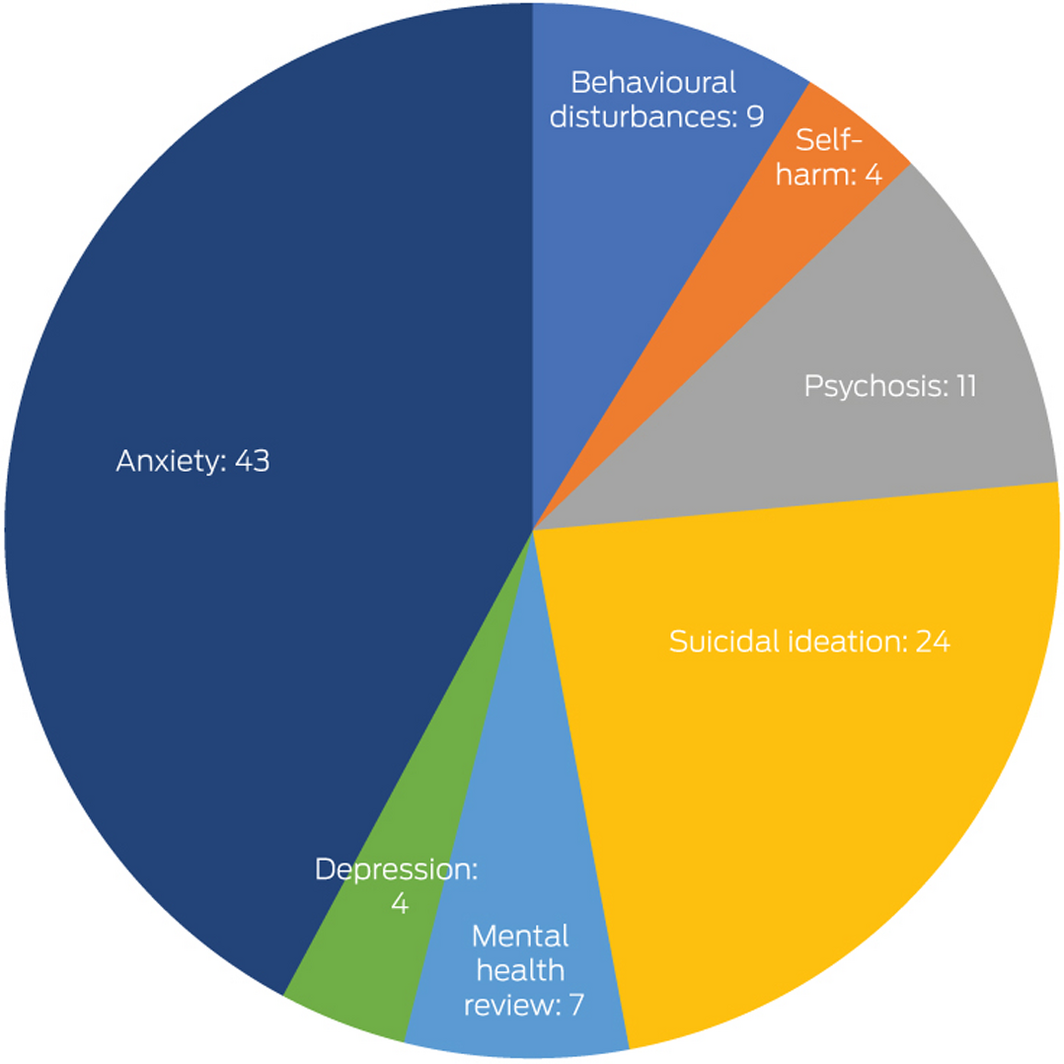
During June – September 2020, 2774 people were registered for accommodation in Special Health Accommodation hotels, of whom 461 (16.6%) presented at least once to the RPA ED (542 ED presentations in total). Thirteen patients (2.8%) were diagnosed with COVID‐19, none of whom required intensive care. The most frequent ED diagnosis categories were mental health (102 presentations, 19%) and cardiovascular conditions (84, 15%) (Box 1). The most frequent reasons for mental health presentations were anxiety (43 presentations), suicidal ideation (24), and acute psychosis (11) (Box 2). The median length of stay for presentations with mental health conditions (543 min; interquartile range [IQR], 372–788 min) was longer than for non‐mental health presentations (433 min; IQR, 302–598 min). Mental health‐related presentations were also associated with higher triage acuity: 86 presentations (84%) were deemed urgent or potentially life‐threatening, compared with 316 of the 440 ED presentations not related to mental health (72%). A larger proportion of mental health presentations were by patients with pre‐existing mental health conditions (65, 64% v 49 non‐mental health presentations, 11%).
The COVID‐19 pandemic continues to have significant direct and indirect health care consequences, including effects on mental health.3 Mental health presentations to the RPA ED comprised 19% of presentations by people from Special Health Accommodation hotels, five times the proportion for all ED presentations in Australia (3.6%).4,5 Further, lengthy ED stays (the median stay was longer than nine hours) probably compounded psychological stress in patients who presented with mental health problems; only 16% of patients were admitted or discharged within the recommended four hours (Box 1).
Our study, the first to assess the impact of mental health during hotel quarantine in Australia, highlights the need for increased psychological support and other services for people in quarantine.6 While quarantine was a vital public health measure for curbing the spread of SARS‐CoV‐2, isolation can cause direct and indirect physical and psychological harm.7 All patients who presented to the RPA ED with mental health problems were routinely followed up by RPA Virtual Hospital psychologists. A prospective study is currently underway to better understand the psychological impact of hotel quarantine as the COVID‐19 pandemic response evolves in 2021.
Box 1 – Characteristics of 542 presentations by people from Special Health Accommodation hotels to the Royal Prince Alfred emergency department, June–September 2020
|
Characteristic |
Number |
||||||||||||||
|
|
|||||||||||||||
|
Age (years), mean (SD) |
43.5 (22.0) |
||||||||||||||
|
Sex (men) |
284 (52.4%) |
||||||||||||||
|
Triage category |
|
||||||||||||||
|
1 (life threatening) |
0 |
||||||||||||||
|
2 (potentially life threatening) |
87 (16%) |
||||||||||||||
|
3 (urgent) |
315 (58%) |
||||||||||||||
|
4 (semi‐urgent) |
121 (22%) |
||||||||||||||
|
5 (non‐urgent) |
19 (4%) |
||||||||||||||
|
Diagnosis category |
|
||||||||||||||
|
Mental health |
102 (19%) |
||||||||||||||
|
Cardiovascular |
84 (15%) |
||||||||||||||
|
Abdominal/gastrointestinal |
68 (13%) |
||||||||||||||
|
Musculoskeletal |
35 (6%) |
||||||||||||||
|
Injury |
32 (6%) |
||||||||||||||
|
Neurological |
28 (5%) |
||||||||||||||
|
Urological |
27 (5%) |
||||||||||||||
|
Fever/infection |
26 (5%) |
||||||||||||||
|
Social |
23 (4%) |
||||||||||||||
|
Obstetrics/gynaecology |
23 (4%) |
||||||||||||||
|
Allergy/skin rash |
19 (4%) |
||||||||||||||
|
Respiratory |
12 (2%) |
||||||||||||||
|
Ear, nose, throat, and eye |
12 (2%) |
||||||||||||||
|
Administrative/pathology tests/prescriptions |
11 (2%) |
||||||||||||||
|
General complaints |
10 (2%) |
||||||||||||||
|
Drug health/toxicology |
10 (2%) |
||||||||||||||
|
Haematology/oncology |
7 (1%) |
||||||||||||||
|
Other |
13 (2%) |
||||||||||||||
|
Length of stay: less than 4 hours, by disposition |
|
||||||||||||||
|
All presentations |
86/542 (16%) |
||||||||||||||
|
Discharged from emergency department |
58/416 (14%) |
||||||||||||||
|
Admitted to inpatient ward |
28/126 (22%) |
||||||||||||||
|
Pre‐existing conditions (461 patients) |
|
||||||||||||||
|
None |
154 (33%) |
||||||||||||||
|
Mental health |
89 (19%) |
||||||||||||||
|
Hypertension |
83 (18%) |
||||||||||||||
|
Ischaemic heart disease |
25 (5%) |
||||||||||||||
|
Diabetes mellitus |
34 (7%) |
||||||||||||||
|
Respiratory disorder |
28 (6%) |
||||||||||||||
|
Renal disorder |
5 (1%) |
||||||||||||||
|
Cancer |
15 (4%) |
||||||||||||||
|
Neurological disorder |
13 (3%) |
||||||||||||||
|
Pregnancy |
24/220 (11%) |
||||||||||||||
|
Disposition at discharge |
|
||||||||||||||
|
Treatment complete |
409 (75%) |
||||||||||||||
|
Admitted to critical care ward |
14 (3%) |
||||||||||||||
|
Admitted to ward |
112 (21%) |
||||||||||||||
|
Discharged |
7 (1%) |
||||||||||||||
|
|
|||||||||||||||
|
SD = standard deviation. |
|||||||||||||||
Received 23 October 2020, accepted 16 March 2021
- 1. NSW Ministry of Health. Public health (COVID‐19 quarantine) order 2020. https://www.health.nsw.gov.au/Infectious/diseases/Documents/covid-19-quarantine-order-2020.pdf (viewed Apr 2021).
- 2. Hutchings O, Dearing C, Jagers D, et al. Virtual health care for community management of patients with COVID‐19 [preprint]; 15 May 2020. medRxiv 2020; https://doi.org/10.1101/2020.05.11.20082396.
- 3. Pfefferbaum B, North CS. Mental health and the Covid‐19 pandemic. N Engl J Med 2020; 383: 510–512.
- 4. Australian Institute of Health and Welfare. Mental health services in Australia. Updated 26 Mar 2021. https://www.aihw.gov.au/reports/mental-health-services/mental-health-services-in-australia/report-contents/hospital-emergency-services (viewed Apr 2021).
- 5. Perera J, Wand T, Bein KJ, et al. Presentations to NSW emergency departments with self‐harm, suicidal ideation, or intentional poisoning, 2010–2014. Med J Aust 2018; 208: 348–353. https://www.mja.com.au/journal/2018/208/8/presentations-nsw-emergency-departments-self-harm-suicidal-ideation-or
- 6. Nussbaumer‐Streit B, Mayr V, Dobrescu AI, et al. Quarantine alone or in combination with other public health measures to control COVID‐19: a rapid review. Cochrane Database Syst Rev 2020; CD013574.
- 7. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 2020; 395: 912–920.





We thank all the staff who provided care for patients in the Special Health Accommodation hotels and COVID‐19 hot zones in the Royal Prince Alfred emergency department.
No relevant disclosures.