The known Suicide and self-harm are significant causes of morbidity and mortality worldwide, and suicide is a leading cause of death among adolescent Australians.
The new The number of mental health presentations to emergency departments in NSW increased during 2010–2014, particularly presentations by adolescents with suicidal ideation/behaviour or self-harm.
The implications Our findings highlight the need to better delineate drivers of the rise in presentation numbers, and to improve targeted mental health care delivery in emergency departments.
Suicide and intentional self-harm are significant causes of adolescent morbidity and mortality worldwide.1,2 In Australia, suicide was the most common cause of death in those aged 5–17 years in 2016,3-5 with a national rate of 2.3 per 100 000 population nationwide during 2012–2016, and 1.8 per 100 000 in New South Wales.4 In a recent survey, self-harm at some point in their lives was reported by 11% of Australians aged 12–17,6 and this is similar to overseas figures.7 A prior history of self-harm is a well described risk factor for further self-harm8 and for attempted and completed suicide.7,9
The emergency department (ED) is often the first point of contact with the health system for people in mental distress,10,11 particularly those who have harmed themselves or have suicidal ideation, but few Australian studies have examined this group of vulnerable ED patients.10 A retrospective review of mental health presentations to 36 NSW EDs during 1999–2006 found that the number of presentations had increased by 49.8%;12 in a Victorian study, the number of ED mental health presentations had more than doubled between 2004 and 2013.13
Our study evaluated population trends in presentations to NSW EDs for mental health problems during 2010–2014, particularly presentations with self-harm, intentional poisoning, or suicidal thoughts or behaviour. Our aim was to provide insights that would assist identifying people at particular risk, as well as shortcomings of our health care system that might be eased by appropriate early interventions, models of acute care, and health policy.
Methods
Design and setting
We undertook a retrospective, descriptive analysis of linked ED presentation data for NSW over five calendar years, 2010–2014. NSW is the most populous Australian state, with a population of about 7.5 million people in 2014.14
Data sources
The Emergency Department Data Collection (EDDC) registry contains routinely collected administrative and clinical data for presentations to all public hospital EDs in NSW. Probabilistic linkage was performed by the NSW Centre for Health Record Linkage (CHeReL; www.cherel.org.au) to obtain patient-level data for all sites and to avoid double-counting of encounters for patients transferred between hospitals. Data analysed included arrival mode, patient registration, type of visit, triage category, mode of separation, and the ED diagnosis at discharge. Population data for the Sydney Statistical Division were obtained from the Australian Bureau of Statistics.14
Patient population
Patients were included if they had presented to an ED and had a mental health-related diagnosis recorded by clinicians as the principal ED diagnosis. Diagnoses were entered by ED clinicians into ED electronic medical records as SNOMED-CT concept identifiers15 or International Classification of Diseases, version 10, Australian modification (ICD-10-AM) codes.16 Patients transferred from other health facilities were excluded to avoid double-counting of presentations, as were patients who were dead on arrival. Of the 150 EDs that submitted data to the EDDC during 2010–2014, 35 small rural EDs were excluded because data were incomplete for 2010–11. Patient presentation, rather than individual-level risk or incidence of diagnoses, was the unit of analysis for measuring ED workload.
Data variable definitions
A full list of data definitions and data collection methods for the EDDC is available online.17 The principal ED diagnosis for mental health presentations entered by treating clinicians as SNOMED-CT or ICD-10-AM codes were collated into broad diagnostic groups (ICD-10-AM codes F10–F99 and E950–E959, mapped to equivalent International Classification of Diseases, ninth revision, clinical modification [ICD-9-CM]18 and SNOMED codes). Self-harm included diagnoses encompassing “self-cutting”, “thoughts of self-harm”, and “threatening self-harm”. Suicidal ideation and behaviour included diagnostic terms such as “feeling suicidal”, “suicide risk”, “suicide attempt”, and “suicidal plans”. Intentional poisoning excluded accidental poisonings and diagnoses related to drug dependence. Diagnoses related to developmental disorders or eating disorders were excluded.
The Australasian Triage Scale19 was used to define urgency. Patient details, including age, sex, and Indigenous status, were recorded at the time of patient registration by the ED.
Outcomes
Outcomes of interest were rates of mental health-related presentations to EDs by age group and calendar year, both overall and for the subgroups of self-harm, suicidal ideation and behaviour (suicidal intent, suicidal ideation or attempted suicide), and intentional poisoning presentations.
Statistical analysis
Annual rates of change for each age group were calculated using the compound interest formula:
Annual rate = [(P1/P0)1/n–1] × 100%
where P1 is the final rate, P0 the initial rate, and n the number of years. Statistical analyses were performed in SAS Enterprise Guide 4.3 (SAS Institute). Age-specific rates per 100 000 population were calculated and plotted in Excel (Microsoft).
Ethics
Approval for analysing de-identified data was obtained from the NSW Population and Health Services Research Ethics Committee and the Aboriginal Health and Medical Research Council Ethics Committee (reference for both, 2014/06/537).
Results
All mental health-related presentations
There were 338 303 mental health presentations to 115 NSW EDs during 2010–2014, of which 331 493 met study inclusion criteria. Of these, 22 274 presentations (6.7%) were by Indigenous Australians. The mean age of presenting patients was 37.3 years (standard deviation [SD], 17.4 years) (Box 1). A similar proportion of males and females received mental health-related principal ED diagnoses, but 64% of those diagnosed with self-harm and 71% of those diagnosed with intentional poisoning were female. About 60% of presentations were classified as triage categories 1–3 (urgent to potentially life-threatening). The median length of stay in the ED was 227 min (interquartile range, 125–399 min); 54% of patients were discharged from the ED within 4 hours of arrival and 36% were admitted to hospital. Nearly one-third of presentations (31.5%) were associated with at least one other mental health presentation by the patient during the previous month.
In 2014, the presentation rate was highest for the 15–19-year-old age group (2167 cases per 100 000 population), and had increased by 11.8% per year during 2010–2014; the presentation rate for the 10–14-year-old age group was 653 cases per 100 000 population, but had increased by 13.8% per year across the study period (Box 2).
Presentations with self-harm, suicidal ideation, or intentional poisoning
More than half of all presentations in these categories were outside normal working hours (08:00–18:00); 46% of people presenting with self-harm, 43% of those with suicidal ideation, and 45% of those with intentional poisoning presented between 18:01 and 23:59. Although rates of presentation were lower than for the other two categories, intentional poisoning was associated with more urgent triage categories (categories 1 or 2, 37%), higher admission rates (66%), and longer ED lengths of stay (median, 402 min; interquartile range, 255–701 min). Self-harm-related presentations were associated with younger age groups (mean, 28.4 years; SD, 13.7 years) and a higher number of re-presentations in the past month and year (median, 3; interquartile range, 1–8) (Box 1).
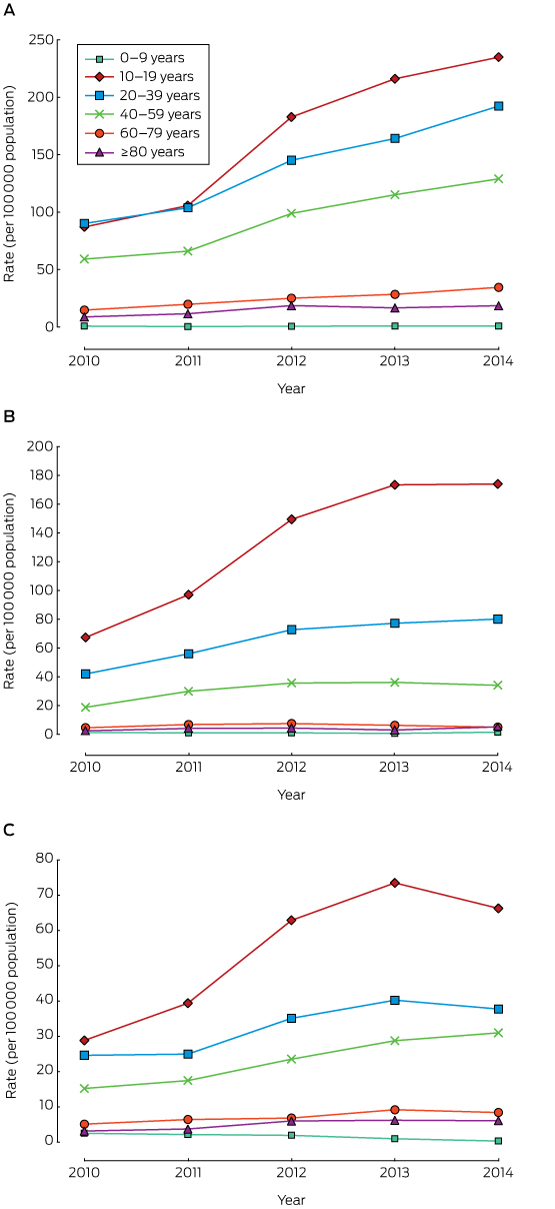
Presentation rates increased across the study period for all age groups, except for children aged 0–9 years. The most marked increase was for those aged 10–19 years (mean annual increase, 27%) (Box 3). The overall number of presentations for suicidal ideation was higher than for self-harm and intentional poisoning combined (Box 1). Changes in presentation rates for suicidal ideation, self-harm, and intentional poisoning by age group across the study period are depicted in Box 4.
Discussion
Although increases in the number of ED presentations over the past decade have been described,20 ours is the first report to describe the rising rate of mental health presentations in NSW on the basis of linked data. We found that the rate of increase was greater than the reported overall increase in ED presentation numbers,20 and was more pronounced in certain age groups. Analysing linked data for all mental health-related presentations to EDs provided a more complete picture of the overall burden of mental health-related presentations in the public hospital system, including the impact of repeat presentations, than earlier studies of inpatient admissions.21
This approach allowed a number of important observations. Firstly, there was a marked rise in the population rate of patients presenting with mental health problems to EDs, particularly of adolescents (10–19 years old) presenting with self-harm or suicidal ideation; this is consistent with overseas reports.6 Secondly, more than half the patients presenting with suicidal ideation, self-harm, and intentional poisoning did so outside normal working hours. There has been much debate in health policy circles about whether increases in the number of ED presentations are driven by changes in access to primary care or community health services, especially by difficulties in obtaining same-day or after-hours appointments, and by the financial burden of general practice appointments that are not bulk-billed.22 However, about 60% of all mental health presentations to EDs were triaged as urgent or potentially life-threatening (Box 1), highlighting the acute nature of these presentations and the probable need for ED assessment. Thirdly, about one-third of all mental health presentations were associated with another mental health-related ED presentation during the previous month, suggesting deficiencies in current models of care, access to general practice follow-up, and community mental health resource provision.
Adolescence is a period of significant neurocognitive development and hormonal change,7,23,24 and is associated with heightened impulsivity and risk-taking behaviour.7 This period of vulnerability is the peak phase for the emergence of mental health disorders,24 which may contribute to the high rate of mental health-related ED presentations by adolescents. Their first presentation to an ED may also be their first mental health-related presentation to any medical service, potentially placing additional stress on the health system in terms of diagnosis and linkage with treatment.
However, the rapid rise in presentations between 2010 and 2014 is likely to be multifactorial, with contributing elements including changes to family and peer relationships,7 onset of substance misuse (which often co-exists with mental health disorders) at younger ages,6,25 improved recognition of mental health problems, and the increasing prevalence of social media and smartphone technology.7,26-28 Recent reviews underscore the significance of social media for adolescent mental health, although definite causative associations have not been established.26,27 Nevertheless, it has been hypothesised that increased exposure to social media normalises self-harm,26 making teenagers vulnerable to peer pressure7 and cyber-bullying,6,27 as well as to low self-esteem, anxiety, depression, self-harm, and suicidal ideation.
The rising number of presentations to EDs may not reflect a genuine increase in the prevalence of mental health disorders in the community. The 2015 Australian Child and Adolescent Survey of Mental Health and Wellbeing6 found no change in the reported prevalence of major depressive disorder in 6–11-year-old children between 1998 and 2013–14, but the prevalence in 12–17-year-olds rose from 2.9% to 5.0%.6 On the other hand, both school- and health system-based service use by 6–17-year-olds with mental health disorders increased significantly between 1998 and 2013–14, with health system use increasing from 25.7% to 50.9%.6 As noted in the report on this survey6 and in the Fourth Australian National Mental Health Plan,11 higher rates of presentation may reflect improved awareness among individuals, schools, and the community of mental health problems, leading to more young people seeking help. Further, recognition of the ED as the first point for accessing care for acute mental health problems may have increased.10,11
Whatever the reasons for the increase in presentation numbers, our findings indicate that improved models of mental health care are required, both in NSW EDs and in the community. A recent Cochrane review29 of interventions for self-harm in children and adolescents noted that investigations of treatments and their effectiveness were rare. The review found little support for group-based therapy; promising interventions generally required extended one-on-one contact. Additionally, evidence for the usefulness of cognitive behavioural therapy in this age group was lacking, despite its known benefits in adults who self-harm.29 A trial of an extended hours mental health liaison service in the ED of an inner city Sydney teaching hospital30 improved access to specialised assessment, support, and therapeutic care, and enhanced the follow-up of people presenting with undifferentiated mental health problems. The service also supported ED staff and improved overall ED service provision; the model is now being more broadly implemented across NSW.
The 2015 Council of Australian Governments’ strategic framework for child and youth health nominated reducing the rates of self-harm and suicide by young people and the prevalence of mental health disorders in these age groups as key priorities for the coming decade.31 The fourth Australian National Mental Health Plan (2009–2014) recognised that EDs are frequently the initial point of contact with the mental health system,11 providing an initial opportunity for identifying people at risk. Early one-on-one interventions could play a crucial role in altering the trajectory of mental illness, with prompt treatment at a young age potentially reducing disease burden and disability in later life,23,32 and may also prevent secondary functional disturbances.
Limitations
The most important limitation of our study was that it was based on linkage of statewide administrative data with clinical diagnoses in the ED dataset (ie, SNOMED-CT and ICD-10-AM codes entered by clinicians). We did not assess the accuracy of coding by ED clinicians, but the broad diagnosis classification groups of this dataset, including mental health diagnoses, have been reported to be aligned with national ED data published by the Australian Institute of Health and Welfare.30 Nevertheless, the validity of and variation in the entry of specific mental health diagnosis codes by ED clinicians should be further investigated to inform the development of better clinical systems for accurate diagnostic coding in electronic medical records. Further, the dataset only captured the principal diagnosis and presenting problem, and did not provide information on secondary or concurrent diagnoses that may have been relevant. Finally, significant overlap between presentations in the categories of self-harm, suicidal ideation or behaviour, and intentional poisoning is likely.
Data from several small rural centres (around 1% of the dataset) were incomplete for the period 2010–2014 and therefore excluded. We did not examine sex-specific trends, nor did we explore the effects of socio-economic factors, such as location and cultural influences, which are known to affect mental health. Indigenous patients constituted 6.7% of all patients presenting to NSW EDs with mental health problems, higher than the proportion of Indigenous Australians in the NSW population (2.9%);14 this is consistent with the higher rate of suicidal behaviour in Indigenous Australian communities.3,21
Conclusions
During 2010–2014, the number of adolescents presenting to EDs in NSW with suicidal ideation and behaviour, self-harm, or intentional poisoning increased markedly. Improved ED models of care and access to community mental health services are required to reverse this worrying trend. Causative factors and gaps in care should be investigated to allow development of targeted policy and services, both in the ED and in the community.
Box 1 – Demographic and clinical characteristics of patients presenting to New South Wales emergency departments (EDs) with mental health problems, 2010–2014
|
|
Emergency department presentations by category |
||||||||||||||
|
All mental health presentations |
Self-harm |
Suicidal ideation and behaviour |
Intentional poisoning |
||||||||||||
|
|
|||||||||||||||
|
Number of patients |
331 493 |
16 215 |
32 663 |
8638 |
|||||||||||
|
Age mean (years), mean (SD) |
37.3 (17.4) |
28.4 (13.7) |
33.7 (15.0) |
32.7 (16.0) |
|||||||||||
|
Sex (male) |
159 024 (48.0%) |
5802 (35.8%) |
16 601 (50.8%) |
2532 (29.3%) |
|||||||||||
|
Indigenous Australians |
22 274 (6.7%) |
1317 (8.1%) |
2558 (7.8%) |
490 (5.7%) |
|||||||||||
|
Admitted to hospital |
120 322 (36.3%) |
5470 (33.7%) |
16 499 (50.5%) |
5727 (66.3%) |
|||||||||||
|
Left prior to completion of treatment |
26 157 (7.9%) |
1461 (9.0%) |
2041 (6.3%) |
230 (2.7%) |
|||||||||||
|
Had presented to ED with mental health problem in past month |
104 565 (31.5%) |
5439 (33.5%) |
10 944 (33.5%) |
2012 (23.3%) |
|||||||||||
|
Re-presentations in past year, median (IQR) |
1 (0–4) |
3 (1–8) |
3 (1–6) |
2 (1–5) |
|||||||||||
|
Triage category |
|
|
|
|
|||||||||||
|
1 (immediately life-threatening) |
2019 (0.6%) |
100 (0.6%) |
148 (0.5%) |
398 (4.6%) |
|||||||||||
|
2 (imminently life-threatening) |
42 253 (12.8%) |
2343 (14.5%) |
7021 (21.5%) |
2829 (32.8%) |
|||||||||||
|
3 (potentially life-threatening) |
155 232 (46.8%) |
9011 (55.6%) |
18 602 (57.0%) |
4752 (55.0%) |
|||||||||||
|
4 (potentially serious) |
113 803 (34.3%) |
4481 (27.7%) |
6522 (20.0%) |
628 (7.3%) |
|||||||||||
|
5 (less urgent) |
18 090 (5.5%) |
274 (1.7%) |
365 (1.1%) |
30 (0.4%) |
|||||||||||
|
Length of stay (min), median (IQR) |
227 (125–399) |
253 (158–460) |
275 (164–507) |
402 (255–701) |
|||||||||||
|
Presented to metropolitan hospital ED |
217 833 (65.7%) |
11 524 (71.1%) |
22 949 (70.3%) |
5987 (69.3%) |
|||||||||||
|
Presented to tertiary hospital ED |
203 182 (61.2%) |
10 674 (65.8%) |
22 211 (68.0%) |
5432 (62.9%) |
|||||||||||
|
Time of presentation |
|
|
|
|
|||||||||||
|
08:00–18:00 |
153 794 (46.4%) |
5628 (34.7%) |
13 565 (41.5%) |
3130 (36.2%) |
|||||||||||
|
18:01–23:59 |
126 608 (38.2%) |
7462 (46.0%) |
14 067 (43.1%) |
3916 (45.3%) |
|||||||||||
|
00:00–07:59 |
51 091 (15.4%) |
3125 (19.3%) |
5031 (15.4%) |
1592 (18.4%) |
|||||||||||
|
|
|||||||||||||||
|
IQR = interquartile range; SD = standard deviation. |
|||||||||||||||
Box 2 – Age-specific rates of presentations for mental health problems to New South Wales emergency departments, 2010–2014
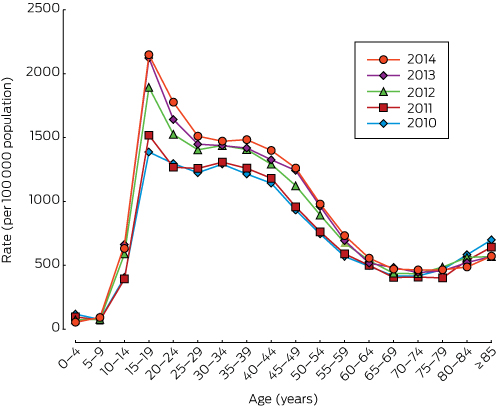
Data source: Emergency Department Data Collection Registry.
Box 3 – Age-specific rates of presentation to New South Wales emergency departments, 2010–2014, by age group
|
Age group |
Age-specific rate of emergency department presentations per 100 000 population |
Total change |
Mean annual change |
||||||||||||
|
2010 |
2011 |
2012 |
2013 |
2014 |
|||||||||||
|
|
|||||||||||||||
|
0–9 years |
4.5 |
3.5 |
3.5 |
2.4 |
2.6 |
–42% |
–13% |
||||||||
|
10–19 years |
183.2 |
242.1 |
395.2 |
463.0 |
475.2 |
159% |
27% |
||||||||
|
20–39 years |
156.7 |
184.7 |
253.0 |
281.6 |
310.2 |
98% |
19% |
||||||||
|
40–59 years |
93.1 |
113.3 |
158.1 |
179.9 |
194.0 |
108% |
20% |
||||||||
|
60–79 years |
24.4 |
32.9 |
39.3 |
43.8 |
47.8 |
96% |
18% |
||||||||
|
≥ 80 years |
14.3 |
19.3 |
28.9 |
25.7 |
29.7 |
107% |
20% |
||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Received 19 June 2017, accepted 9 January 2018
- Jayashanki Perera1
- Timothy Wand1,2
- Kendall J Bein1
- Dane Chalkley1
- Rebecca Ivers3,4
- Katharine S Steinbeck5
- Robyn Shields1
- Michael M Dinh6
- 1 Royal Prince Alfred Hospital, Sydney, NSW
- 2 Sydney Nursing School, University of Sydney, Sydney, NSW
- 3 The George Institute for Global Health, Sydney, NSW
- 4 Flinders University, Adelaide, SA
- 5 University of Sydney, Sydney, NSW
- 6 Sydney Medical School, University of Sydney, Sydney, NSW
We acknowledge the NSW Ministry of Health and the Centre for Health Record Linkage (CHeReL) for granting access to and linkage of the data. This project was funded by the NSW Agency for Clinical Innovation and Emergency Care Institute.
No relevant disclosures.
- 1. Patton GC, Coffey C, Sawyer SM, et al. Global patterns of mortality in young people: a systematic analysis of population health data. Lancet 2009; 374: 881-892.
- 2. Mokdad AH, Patton GC, Murray CJL, et al. Global burden of diseases, injuries, and risk factors for young people’s health during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2016; 387: 2383-2401.
- 3. Australian Bureau of Statistics. 3303.0. Causes of death, Australia, 2015. Suicide in Australia. Sept 2017. http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/3303.0∼2016∼Main%20Features∼Intentional%20self-harm:%20key%20characteristics∼7 (viewed Feb 2018).
- 4. Australian Bureau of Statistics. 3303.0. Causes of death, Australia, 2015. Data cube: Intentional self-harm (suicide) (Australia). Sept 2017. http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3303.02016?OpenDocument (viewed Feb 2018).
- 5. Australian Institute of Health and Welfare. Australian Burden of Disease Study: impact and causes of illness and death in Australia 2011 (AIHW Cat. No. BOD 4; Australian Burden of Disease Study Series No. 3). Canberra: AIHW, 2016.
- 6. Lawrence D, Johnson S, Hafekost J, et al. The mental health of children and adolescents. Report on the second Australian Child and Adolescent Survey of Mental Health and Wellbeing. Canberra: Department of Health, 2015. https://www.health.gov.au/internet/main/publishing.nsf/Content/9DA8CA21306FE6EDCA257E2700016945/%24File/child2.pdf (viewed Apr 2017).
- 7. Hawton K, Saunders KE, O’Connor RC. Self-harm and suicide in adolescents. Lancet 2012; 379: 2373-2382.
- 8. Madge N, Hewitt A, Hawton K, et al. Deliberate self-harm within an international community sample of young people: comparative findings from the Child & Adolescent Self-harm in Europe (CASE) Study. J Child Psychol Psychiatry 2008; 49: 667-677.
- 9. Hawton K, Bergen H, Kapur N, et al. Repetition of self-harm and suicide following self-harm in children and adolescents: findings from the Multicentre Study of Self-harm in England. J Child Psychol Psychiatry 2012; 53: 1212-1219.
- 10. Spirito A, Lewander W. Assessment and disposition planning for adolescent suicide attempters treated in the emergency department. Clin Pediatr Emerg Med 2004: 5: 154-163.
- 11. Australian Health Ministers’ Conference. Fourth National Mental Health Plan. An agenda for collaborative government action in mental health (2009–2014). Canberra: AHMC, 2009. https://www.health.gov.au/internet/main/publishing.nsf/Content/9A5A0E8BDFC55D3BCA257BF0001C1B1C/$File/plan09v2.pdf (viewed Mar 2017).
- 12. Tankel AS, Di Palma MJ, Kramer KM, et al. Increasing impact of mental health presentations on New South Wales public hospital emergency departments 1999–2006. Emerg Med Australas 2011; 23: 689-696.
- 13. Alarcon Manchego P, Knott J, Graudins A, et al. Management of mental health patients in Victorian emergency departments: a 10 year follow-up study. Emerg Med Australas 2015; 27: 529-536.
- 14. Australian Bureau of Statistics. 3101.0. Australian demographic statistics, Jun 2014. Dec 2014. http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/3101.0Main+Features1Jun%202014 (viewed Aug 2016).
- 15. SNOMED International. SNOMED CT browser. http://browser.ihtsdotools.org/? (viewed Mar 2017).
- 16. National Centre for Classification in Health. The International Statistical Classification of Diseases and Related Health Problems, tenth revision, Australian modification (ICD-10-AM). Eighth edition. Wollongong: National Casemix and Classification Centre, University of Wollongong, 2013.
- 17. NSW Ministry of Health. Emergency Department Data Collection. Updated July 2017. http://www.cherel.org.au/media/23786/eddc-data-dictionary-for-cherel-website_20170710.docx (viewed Sept 2017).
- 18. Centers for Disease Control and Prevention. ICD-9-CM. International classification of diseases, ninth revision: clinical modification, 6th edition. Atlanta (GA): US Department of Health and Human Services, CDC, Centers for Medicare and Medicaid Services, 2010.
- 19. Australasian College for Emergency Medicine. Guidelines on the implementation of the Australasian Triage Scale In emergency departments. Nov 2000; revised July 2016. https://acem.org.au/getmedia/51dc74f7-9ff0-42ce-872a-0437f3db640a/G24_04_Guidelines_on_Implementation_of_ATS_Jul-16.aspx (viewed Sept 2017).
- 20. Dinh MM, Berendsen Russell S, Bein KJ, et al. Understanding drivers of demand for emergency service trends in years 2010-2014 in New South Wales: an initial overview of the DESTINY project. Emerg Med Australas 2016; 28: 179-186.
- 21. Australian Institute of Health and Welfare. Suicide and hospitalised self-harm in Australia: trends and analysis (AIHW Cat. No. INJCAT 169; Injury Research and Statistics Series No. 93). Canberra: AIHW, 2014.
- 22. Freed GL, Bingham A, Allen A, et al. Actual availability of general practice appointments for mildly ill children. Med J Aust 2015; 203: 145. <MJA full text>
- 23. Smith AR, Chein J, Steinberg L. Impact of socio-emotional context, brain development, and pubertal maturation on adolescent risk-taking. Horm Behav 2013; 64: 323-332.
- 24. Patton GC, Coffey C, Romaniuk H, et al. The prognosis of common mental disorders in adolescents: a 14-year prospective cohort study. Lancet 2014; 383: 1404-1411.
- 25. Bell L, Stargatt R, Bosanac P, et al. Child and adolescent mental health problems and substance use presentations to an emergency department. Australas Psychiatry 2011; 19: 521-525.
- 26. Rowe SL, French RS, Henderson C, et al. Help-seeking behaviour and adolescent self-harm: a systematic review. Aust N Z J Psychiatry 2014; 48: 1083-1095.
- 27. Hamm MP, Newton AS, Chisholm A, et al. Prevalence and effect of cyberbullying on children and young people: a scoping review of social media studies. JAMA Pediatr 2015; 69: 770-777.
- 28. Ortega-Montiel G. Aussie teens online [online]. Australian Communications and Media Authority. July 2014. http://www.acma.gov.au/theACMA/engage-blogs/engage-blogs/Research-snapshots/Aussie-teens-online (viewed Feb 2017).
- 29. Hawton K, Witt KG, Taylor Salisbury TL, et al. Interventions for self-harm in children and adolescents. Cochrane Database Syst Rev 2015; (12): CD012013.
- 30. Wand T, D’Abrew N, Barnett C, et al. Evaluation of a nurse practitioner-led extended hours mental health liaison nurse service based in the emergency department. Aust Health Rev 2015; 39: 1-8.
- 31. Australian Health Ministers’ Advisory Council. Healthy, safe and thriving: National strategic framework for child and youth health. Aug 2015. http://www.coaghealthcouncil.gov.au/Portals/0/Healthy%20Safe%20and%20Thriving%20-%20National%20Strategic%20Framework%20for%20Child%20and%20Youth%20Health.pdf (viewed Nov 2016).
- 32. Moran P, Coffey C, Romaniuk H, et al. The natural history of self-harm from adolescence to young adulthood: a population-based cohort study. Lancet 2012; 379: 236-243.





Abstract
Objective: To evaluate population trends in presentations for mental health problems presenting to emergency departments (EDs) in New South Wales during 2010–2014, particularly patients presenting with suicidal ideation, self-harm, or intentional poisoning.
Design, setting and participants: This was a retrospective, descriptive analysis of linked Emergency Department Data Collection registry data for presentations to NSW public hospital EDs over five calendar years, 2010–2014. Patients were included if they had presented to an ED and a mental health-related diagnosis was recorded as the principal diagnosis.
Main outcome measures: Rates of mental health-related presentations to EDs by age group and calendar year, both overall and for the subgroups of self-harm, suicidal ideation and behaviour, and intentional poisoning presentations.
Results: 331 493 mental health-related presentations to 115 NSW EDs during 2010–2014 were analysed. The presentation rate was highest for 15–19-year-old patients (2014: 2167 per 100 000 population), but had grown most rapidly for 10–14-year-old children (13.8% per year). The combined number of presentations for suicidal ideation, self-harm, or intentional poisoning increased in all age groups, other than those aged 0–9 years; the greatest increase was for the 10–19-year-old age group (27% per year).
Conclusions: The rate of mental health presentations to EDs increased significantly in NSW between 2010 and 2014, particularly presentations by adolescents. Urgent action is needed to provide better access to adolescent mental health services in the community and to enhance ED models of mental health care. The underlying drivers of this trend should be investigated to improve mental health care.