The response to the largest institutional outbreak of COVID‐19 in health care workers in Australia to date needed to be multidimensional
In many countries, high rates of health care workers with coronavirus disease 2019 (COVID‐19) have been associated with inadequate personal protective equipment (PPE), exposure to large numbers of patients with COVID‐19, worker fatigue, and limited access to diagnostic testing.1,2,3 In Australia, during the initial phase of the epidemic, infections in health care workers were largely attributable to international travel, corroborated by genomically distinct severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) lineages.4,5 At the Royal Melbourne Hospital, we observed a marked increase in staff infections during July and August 2020, concurrent with a statewide surge in COVID‐19 cases. To inform future responses in the Australian setting, we present a description of health care worker infections at our institution and the suite of interventions associated with outbreak control.
Setting
The Royal Melbourne Hospital City Campus is a 550‐bed university‐affiliated tertiary hospital with an additional 150 geriatric and rehabilitation beds at the Royal Park Campus, a large mental health service and four residential aged care facilities, employing about 10 000 staff. Throughout the pandemic, a rapid access COVID‐19 testing clinic was provided for symptomatic staff. To diagnose infection, deep nasal and throat swabs were sampled for nucleic acid testing (reverse transcriptase polymerase chain reaction [RT‐PCR] for SARS‐CoV2). SARS‐CoV‐2 RNA was detected using the Coronavirus Typing assay (AusDiagnostics).5 All positive COVID‐19 tests were notified to the Department of Health and Human Services, with staff members also being notified to the Royal Melbourne Hospital infection prevention services. Infected staff were interviewed by an infection prevention nurse consultant to identify any contacts and enquire about PPE use, work locations in the days before symptoms, nature of their work, characteristics of their patients, and any suspected acquisition events. Contacts with other staff outside work were also explored.
Infected staff were required to isolate for 10 days or more after symptom onset and close contacts (≥ 15 minutes of face‐to‐face contact or ≥ 2 hours in a shared space in the 48 hours before symptom onset) were furloughed for 14 days and quarantined, according to state guidelines. Outbreaks (two or more epidemiologically and/or spatially linked staff and/or patients) were managed by a multidisciplinary incident management team. Data regarding health care worker infections were entered into a REDCap 10 (Research Electronic Data Capture) database, a secure web‐based platform, and were analysed using Stata 16. This study was approved by the Melbourne Health Human Research Ethics Committee (QA2020058).
Overview
Between 1 July and 31 August 2020, 262 cases of COVID‐19 were identified among Royal Melbourne Hospital staff (Box 1 and Box 2). Fifteen individuals (5.7%) required inpatient care and 13 (4.9%) received care by a hospital in the home service. Two were admitted to the intensive care unit (ICU), none requiring mechanical ventilation, with no deaths. Nurses were most commonly affected, followed by support staff (such as food and cleaning services) and doctors (17/21 of these being doctors‐in‐training) (Box 1). The trend in incidence of health care worker infections reflected the prevalence of inpatients with COVID‐19 (Box 3). The ICU had between zero and ten concurrent patients with COVID‐19 over the period (median, 7; interquartile range [IQR], 5.0–8.0), with four ICU staff acquiring COVID‐19. No operating theatre staff and no staff working in affiliated residential aged care facilities were infected. The median turnaround time for health care worker test results (from specimen collection to reporting) was 20.2 hours (IQR, 11.4–29.1 hours). Overt recognised PPE breaches were rarely reported. Contacts with known COVID‐19 cases outside the hospital were infrequent but did occur (eg, health care workers living together).
Outbreak linked to geriatric and rehabilitation inpatient wards
The Royal Park Campus had the highest number of staff with COVID‐19, making up 40.8% (n = 107) of health care worker infections at the Royal Melbourne Hospital, despite this campus constituting about 10% of the total staff workforce at the hospital (acknowledging that some staff move between sites). Between 12 and 18 July, the Royal Park Campus received a large number of patients from external residential aged care facilities, not affiliated with the Royal Melbourne Hospital, with COVID‐19 outbreaks. These residents were COVID‐19‐positive at admission and were managed with appropriate infection precautions throughout. COVID‐19 cases among staff rapidly escalated across all six wards at the campus after 16 July, peaking on 27 July. The peak number of patients with COVID‐19 at the Royal Park Campus was 60.
At the Royal Park Campus there are a variety of buildings constructed from the 1970s to early 2000; most have central air conditioning plants, but one has a local split system. An engineering review of the wards revealed air exchanges met current requirements; however, a more detailed assessment of air movement suggested that some were not as well ventilated as others. Some patients were in single rooms, but many were in multibed spaces. Improved nurse to patient ratios were used to help manage patients. Despite this, because of large numbers of staff furloughs, the remaining staff experienced high workloads. A decision was made on 3 August to close four wards at the Royal Park Campus. Fifteen patients were moved to other health services, while the remaining 45 were moved to single rooms in wards with more modern infrastructure.
Outbreaks linked to “hot wards”
At the Royal Melbourne Hospital City Campus, most affected staff were working in wards with patients with suspected or confirmed COVID‐19 (“hot wards”) (Box 1). These staff were highly trained in PPE use, PPE was always readily available (ie, gowns, gloves, eye protection, and masks), and use was checked by a PPE “buddy” (usually a colleague) before patient room entry and at doffing. Staff noted that particular behaviour in infected patients appeared to be linked to transmission events (patients shouting, vigorous coughing). The peak combined prevalence of inpatients at the Royal Park and City campuses was 99 on 5 August 2020. As increasing numbers of staff infections were recognised, the density of patients on the COVID‐19 wards was reduced by closing beds in shared rooms and moving each patient to a single room where possible. On 21 July, use of N95 (or P2) masks by all staff at all times on COVID‐19 wards at both campuses was instituted. “Spotters” (supernumerary staff) were deployed to observe PPE donning and doffing, and senior staff ward walk‐arounds and additional cleaning with monitoring were implemented. Staff working on “hot wards” were offered weekly asymptomatic testing to detect any infections early.
Outbreaks on “cold wards”
On three occasions, clusters occurred outside the designated “hot wards”; that is, in wards not allocated to caring for patients with suspected or confirmed COVID‐19 infection. In some staff, having previously worked at the Royal Park Campus was identified as a potential risk factor. A management plan for these wards was deployed, including closure to new admissions, moving patients to separate rooms (where possible), managing the whole ward using increased precautions, deep cleaning, and voluntary testing of all patients and staff every 3–4 days. Hospital‐wide asymptomatic staff testing was instituted (> 600 staff tested) and whole hospital inpatient testing occurred as a point prevalence activity in late July, with no additional cases identified outside the affected wards.
Institutional responses
Responses were multifactorial and iterative, with daily review of emerging evidence that informed ongoing decisions. Importantly, a hierarchy of controls was used to manage these outbreaks (Box 4). A proactive approach was used to support infected and furloughed staff wellbeing, with dedicated nursing and medical staff monitoring physical and mental health as well as providing practical supports. This service managed over 680 staff during the outbreak period.
Discussion
We describe the largest institutional outbreak of SARS‐CoV‐2 health care worker infections reported in Australia to date. Our response was necessarily iterative and pragmatic and advice often pre‐dated formal state and federal recommendations. During these outbreaks, a number of key factors emerged that shaped our responses, extending well beyond a focus on PPE alone.
First, the concept of a “critical burden” of infection framed our responses to patient movement and ward closures. Concurrent with large numbers of cases in the hospital and the community, the number of staff who acquired infection rose rapidly. Based on overseas experience,6,7 we hypothesised that large numbers of patients in confined spaces may have created a high density of droplets, aerosols and environmental contamination. This triggered a detailed assessment of ward physical layout, including the possible role of patient placement and air circulation. We elected to use single rooms wherever possible and to physically space infected patients by closing beds on the ward. The intensity of transmission in some wards led to a decision to close wards and move some patients to other health care services. Further, we adopted the use of N95 masks for staff working in areas with large numbers of patients with confirmed or suspected COVID‐19. While use of N95 masks for all COVID‐19 care was not recommended in state or federal guidelines at that time,8,9 this organisational decision was based on our local epidemiology and a need to trial any reasonably available strategy to contain health care worker infections.
Second, the availability of rapid and accessible testing for staff was critical to informing real‐time outbreak management, highlighted by international studies.10,11 Rapid availability of data informed our daily incident management meetings and enabled prompt decision making using the best possible information.
Finally, the importance of staff communication and wellbeing cannot be understated. Similar to other studies,3,12 many staff reported physical and mental fatigue and stress during these outbreaks. In addition, workforce shortages meant that staff were taking on extra shifts at short notice and working in unfamiliar roles. Accordingly, access to employee support programs was an important element of this response.
Box 1 – Demographic characteristics of health care workers with coronavirus disease 2019 (COVID‐19), confirmed by polymerase chain reaction (PCR) testing, at the Royal Melbourne Hospital (1 July – 31 August 2020)
|
Characteristic |
Number of confirmed cases (%) |
||||||||||||||
|
|
|||||||||||||||
|
Total number of confirmed cases |
262 |
||||||||||||||
|
Sex |
|
||||||||||||||
|
Male |
57 (21.8%) |
||||||||||||||
|
Female |
205 (78.2%) |
||||||||||||||
|
Median age at diagnosis (IQR), years |
32.7 (26.8–44.9) |
||||||||||||||
|
Employee type |
|
||||||||||||||
|
Nurse |
179 (68.3%) |
||||||||||||||
|
Doctor |
21 (8.0%) |
||||||||||||||
|
Allied health practitioner |
9 (3.4%) |
||||||||||||||
|
Support staff (food services, environmental services) |
38 (14.5%) |
||||||||||||||
|
Administrative staff |
6 (2.3%) |
||||||||||||||
|
Student |
4 (1.5%) |
||||||||||||||
|
Security staff |
4 (1.5%) |
||||||||||||||
|
Laboratory staff |
1 (0.4%) |
||||||||||||||
|
Location |
|
||||||||||||||
|
Royal Park Campus (rehabilitation, geriatric rehabilitation) |
107 (40.8%) |
||||||||||||||
|
Hot wards* (COVID‐19 wards,† ED, ICU) |
57 (21.8%) |
||||||||||||||
|
Cold wards‡ with recognised COVID‐19 outbreaks (3 wards) |
20 (7.6%) |
||||||||||||||
|
Cold wards‡ with no outbreaks (1 or 2 unlinked cases; 6 wards) |
7 (2.7%) |
||||||||||||||
|
Mental health ward§ |
8 (3.1%) |
||||||||||||||
|
Not ward‐based (eg, non‐clinical) |
31 (11.8%) |
||||||||||||||
|
Unknown (no campus/ward stated, includes both campuses) |
32 (12.2%) |
||||||||||||||
|
|
|||||||||||||||
|
ED = emergency department; ICU = intensive care unit; IQR = interquartile range. * Hot wards are wards dedicated to managing patients with confirmed or suspected COVID‐19. † COVID‐19 wards are wards where patients with confirmed or suspected COVID‐19 were managed. ‡ Cold wards are all other wards. § Mental health wards were situated at the City Campus and at other sites. |
|||||||||||||||
Box 2 – Epidemic curve of health care worker infections at the Royal Melbourne Hospital (1 July – 31 August 2020)
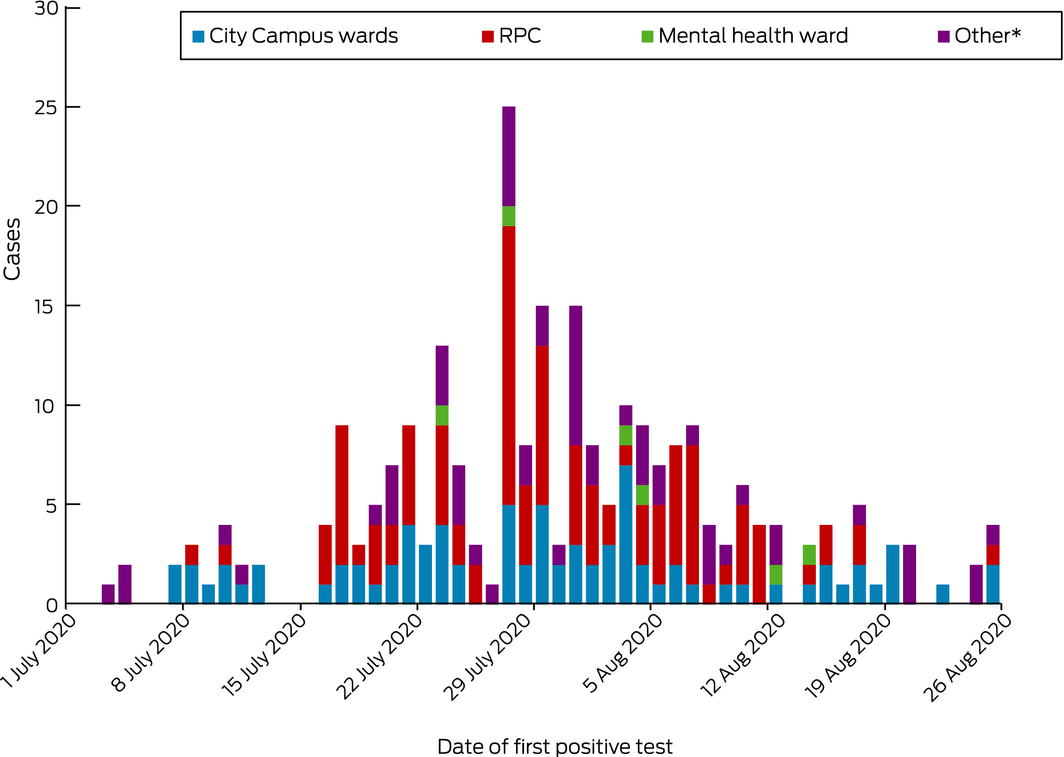
RPC = Royal Park Campus. * “Other” includes non‐clinical not ward‐based staff, staff working across several campuses, or ward not known. Mental health wards include off‐site facilities.
Box 3 – Prevalence of inpatients with coronavirus disease 2019 (COVID‐19) at both the Royal Melbourne Hospital City Campus and the Royal Park Campus over time (13 July – 31 August 2020)*

* Data start on 13 July 2020.
Box 4 – Hierarchy of controls used to guide interventions to address health care worker infection with coronavirus disease 2019 (COVID‐19) at Royal Melbourne Hospital
|
|
|||||||||||||||
|
Elimination* |
|
||||||||||||||
|
Engineering controls |
|
||||||||||||||
|
Administrative controls |
|
||||||||||||||
|
PPE |
|
||||||||||||||
|
|
|||||||||||||||
|
PPE = personal protective equipment. * Actions to remove or minimise the number of infected people on site. |
|||||||||||||||
Provenance: Not commissioned; externally peer reviewed.
- 1. Nguyen LH, Drew DA, Graham MS, et al. Risk of COVID‐19 among front‐line health‐care workers and the general community: a prospective cohort study. Lancet Public Health 2020; 5: e475–e483.
- 2. Chou R, Dana T, Buckley DI, et al. Epidemiology of and risk factors for coronavirus infection in health care workers: a living rapid review. Annals Int Med 2020; 173: 120–136.
- 3. Bielicki JA, Duval X, Gobat N, et al. Monitoring approaches for health‐care workers during the COVID‐19 pandemic. Lancet Infect Dis 2020; 20: e261–e267.
- 4. Muhi S, Irving LB, Buising KL. COVID‐19 in Australian health care workers: early experience of the Royal Melbourne Hospital emphasises the importance of community acquisition. Med J Aust 2020; 213: 44. https://www.mja.com.au/journal/2020/213/1/covid-19-australian-health-care-workers-early-experience-royal-melbourne
- 5. Williams E, Bond K, Chong B, et al. Implementation and evaluation of a novel real‐time multiplex assay for SARS‐CoV-2: in‐field learnings from a clinical microbiology laboratory. Pathology 2020; https://doi.org/10.1016/j.pathol.2020.08.004 [Epub ahead of print].
- 6. Liu Y, Ning Z, Chen Y, et al. Aerodynamic analysis of SARS‐CoV-2 in two Wuhan hospitals. Nature 2020; 582: 557–560.
- 7. Klompas M, Baker MA, Rhee C. Airborne transmission of SARS‐CoV-2: theoretical considerations and available evidence. JAMA 2020; 324: 441–442.
- 8. Bartoszko JJ, Farooqi MAM, Alhazzani W, Loeb M. Medical masks vs N95 respirators for preventing COVID‐19 in healthcare workers: a systematic review and meta‐analysis of randomized trials. Influenza Other Respir Viruses 2020; 14: 365–373.
- 9. Dau NQ, Peled H, Lau H, et al. Why N95 should be the standard for all COVID‐19 inpatient care. Annals Int Med 2020; https://doi.org/10.7326/m20-2623 [Epub ahead of print].
- 10. Keeley AJ, Evans C, Colton H, et al. Roll‐out of SARS‐CoV-2 testing for healthcare workers at a large NHS Foundation Trust in the United Kingdom, March 2020. Euro Surveill 2020; 25: 2000433.
- 11. Kluytmans‐van den Bergh MFQ, Buiting AGM, Pas SD, et al. Prevalence and clinical presentation of health care workers with symptoms of coronavirus disease 2019 in 2 Dutch hospitals during an early phase of the pandemic. JAMA Netw Open 2020; 3: e209673.
- 12. Liu Q, Luo D, Haase JE, et al. The experiences of health‐care providers during the COVID‐19 crisis in China: a qualitative study. Lancet Glob Health 2020; 8: e790–e798.





We thank Chris Bailie, Vivian Leung and Neha Verma for their support in data collection and analysis. We also thank Ashley Stevens and Nick Keogh from the Royal Melbourne Hospital engineering team for reviewing the manuscript.
No relevant disclosures.