Colorectal cancer is an important cause of morbidity and mortality in Australia.1 The National Bowel Cancer Screening Program (NBCSP) aims to detect the disease early by offering faecal occult blood testing (faecal immunochemical test, FIT) to people aged 50–74 years.2 The expansion of the NBCSP has been paralleled by increased numbers of FITs outside the program (community‐initiated FITs) for a number of reasons, including the presence of symptoms.
We investigated whether colonoscopy services should provide endoscopies to patients with positive FIT results with the same priority, regardless of whether the test was instigated by the NBCSP, by analysing data from the Newcastle Direct Access Colonoscopy Service (DACS) for the period 2014–18. The DACS manages all patients in the same manner: a positive FIT result leads to assessment for colonoscopy.3,4 Ethics approval was granted by the Hunter New England Human Research Ethics Committee (reference, AU201608‐01).
All data were recorded prospectively. Findings were categorised according to surveillance categories endorsed by the Gastroenterological Society of Australia and the Colorectal Surgical Society of Australia and New Zealand.5 Data accuracy was confirmed by reviewing the primary sources for 10% of patients.
We identified 2693 patients referred for screening colonoscopy between 1 July 2014 and 30 June 2018; 1439 (53%) had had community‐initiated FITs (Box 1). After excluding 318 patients who did not attend or were lost to follow‐up (community‐initiated, 200; NBCSP, 118) and ten patients with poor bowel preparation and no follow‐up colonoscopy during the study period, 2365 complete screening colonoscopy outcomes were analysed: 1233 following community‐initiated and 1132 following NBCSP testing. With these sample sizes, the study had 80% power to detect differences in colonic neoplasia rate ranging from 16 percentage points (assumed prevalence, 50%) to two percentage points (assumed prevalence, 3%). Z‐tests were used to calculate P values, and Wald tests (two‐tailed) for calculating confidence intervals (CIs) for the differences between the two groups. Differences between the two groups in the proportion of patients with each specific finding are presented with 99% asymptotic CIs to control for multiple testing.
Colonoscopy quality was high: the completion rate (defined as either caecal intubation, reaching an ileocolic anastomosis, or reaching an obstructing mass lesion) was 97.1% (community‐initiated, 1193 of 1233, 96.8%; NBCSP, 1104 of 1132, 97.5%), and the adenoma detection rate was 49%, exceeding international benchmarks for either symptomatic or screening patients (for screening: at least 25% in men and 15% in women;6 for populations enriched with patients with positive FIT results: 35%7). The rate of colorectal neoplasia (malignant or pre‐malignant) was similar in the two groups. Importantly, the difference in the rates of adenocarcinoma was not statistically significant (community‐initiated, 4.0%; NBCSP, 2.7%; difference, 1.3 percentage points [99% CI, –0.6 to 3.3 percentage points]; P = 0.09). The only statistically significant difference by type was that the incidence of high risk adenoma was slightly higher in the NBCSP group (22.9% v 17.2%; difference, 5.7 percentage points [99% CI, 1.4–10 percentage points]; P < 0.001) (Box 2).
We found that the incidence and detection rates of colorectal neoplasia in people aged 50–74 years were similar for people with positive results for NBCSP or community‐initiated FITs. The large population in our study means that it provides colonoscopy providers strong evidence that evaluation should be performed equally promptly for patients with positive results from NBSCP and community‐initiated FITs.
Box 1 – Demographic characteristics of the 2693 patients with positive faecal immunochemical test results and referred to the Newcastle Direct Access Colonoscopy Service for colonoscopy, 2014–18
|
|
Faecal immunochemical test |
Total |
|||||||||||||
|
Community‐initiated |
NBCSP |
||||||||||||||
|
|
|||||||||||||||
|
Number of patients |
1439 |
1254 |
2693 |
||||||||||||
|
Sex |
|
|
|
||||||||||||
|
Women |
675 |
559 |
1234 |
||||||||||||
|
Men |
764 |
695 |
1459 |
||||||||||||
|
Age (years), mean (SD) |
62.9 (6.8) |
63.2 (7.3) |
63.1 (7.0) |
||||||||||||
|
Numbers of patients |
|
|
|
||||||||||||
|
50–54 years |
213 |
147 |
360 |
||||||||||||
|
55–59 years |
280 |
271 |
551 |
||||||||||||
|
60–64 years |
312 |
212 |
524 |
||||||||||||
|
65–69 years |
330 |
288 |
618 |
||||||||||||
|
70–74 years |
304 |
336 |
640 |
||||||||||||
|
|
|||||||||||||||
|
NBCSP = National Bowel Cancer Screening Program; SD = standard deviation. |
|||||||||||||||
Box 2 – Differences in colonoscopy outcomes for people who had community‐initiated (1233 patients) or NBCSP (1132 patients) faecal immunochemical tests
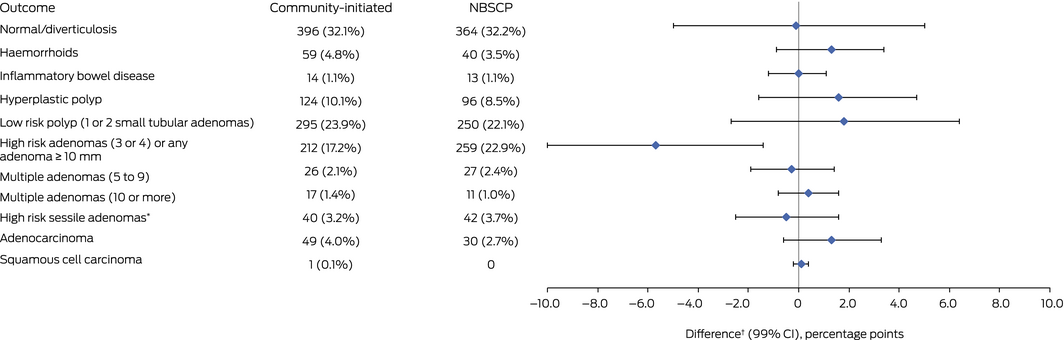
CI = confidence interval; NBCSP = National Bowel Cancer Screening Program. *Large sessile polyps (> 2 cm) or malignant polyps. † Between values for community‐initiated and NBCSP groups.
Received 29 April 2019, accepted 6 November 2019
- 1. Australian Institute of Health and Welfare. Cancer in Australia: an overview 2014 (Cat. no. CAN 88; Cancer series no. 90). Canberra: AIHW, 2015.
- 2. Australian Department of Health. National Bowel Cancer Screening Program. Undated. http://www.cancerscreening.gov.au/internet/screening/publishing.nsf/Content/bowel-screening-1 (viewed Dec 2019).
- 3. Clarke L, Pockney P, Gillies D, et al. Time to colonoscopy for patients accessing the Direct Access Colonoscopy Service compared to the normal service in Newcastle, Australia. Intern Med J 2019; 49: 1132–1137.
- 4. Clarke L, Pockney P, Gillies D, et al. Direct access colonoscopy service for bowel cancer screening produces a positive financial benefit for patients and local health districts. Intern Med J 2019; 49: 729–733.
- 5. Barclay K; Cancer Council Australia Surveillance Colonoscopy Guidelines Working Party. Algorithm for colonoscopic surveillance intervals: adenomas. 2013. https://cart.gesa.org.au/membes/files/Professional/Algorithm%20for%20Colonoscopic%20Surveillance%20Intervals%20-%20Adenomas.pdf (viewed Dec 2019).
- 6. Rex DK, Bond JH, Winawer S, et al; US Multi‐Society Task Force on Colorectal Cancer. Quality in the technical performance of colonoscopy and the continuous quality improvement process for colonoscopy: recommendations of the US Multi‐Society Task Force on Colorectal Cancer. Am J Gastroenterol 2002; 97: 1296–1308.
- 7. Cancer Council Australia. Clinical practice guidelines for surveillance colonoscopy: quality of colonoscopy. Updated Mar 2019. https://wiki.cancer.org.au/australia/Guidelines:Colorectal_cancer/Colonoscopy_surveillance/Quality_of_colonoscopy (viewed Dec 2019).





The development of the Newcastle Direct Access Colonoscopy Service was co‐funded by Cancer Institute NSW and Hunter New England LHD Cancer Services. The funders had no role in the planning, writing, or publication of this article.
Cancer Institute NSW contributed funding to establish the Direct Access Colonoscopy Service in the Hunter New England Local Health District.