The coronavirus disease 2019 (COVID‐19) pandemic is pushing health systems to, and possibly beyond, their limits.1 In Italy, the exponential rise in case numbers has caused a corresponding rise in demand for intensive care unit (ICU) beds.2 To determine how many ICU beds will be required in Australia, we propose a simple model of an uninterrupted pandemic process based on the local situation in late March 2020, and compare this model with recent data from the Lombardy.3
The uninterrupted exponential growth scenario
In queueing theory, Little's law4 describes the relationship between the number of patients in a system (L) and the mean arrival rate (λ) and length of time the patient remains in the system (W) as:
L = λW
If a tertiary hospital has a steady state rate of 20 new admissions of patients with confirmed COVID‐19 per day, of whom one requires ICU admission5 (λ) for a mean 10 days (W), the hospital ICU will need at least 10 beds to accommodate these patients.
If, however, the number of new confirmed cases increases by 20% each day (in late March 2020, the number was increasing in Australia by 23% each day6), and 100 cases are confirmed on one day, about 120 will be confirmed on the next. This increase in the daily rate of 20 new cases will mean one extra ICU admission per day, and the need for at least 10 further ICU beds.
That is, the total number of ICU beds needed will be about 10% of the number of confirmed cases, or 50% of the number of new cases during the exponential growth phase of the epidemic. Approximately 2300 ICU beds are available in Australia;7 if public health measures fail to curb the rate of growth in case numbers, the national ICU capacity would be exceeded when the number of COVID‐19 cases reaches 23 000. Other sources8 have estimated that Australia could cope with as many as 44 580 COVID‐19 cases, but this would grant only a 3‐day extension before ICU capacity was exceeded.
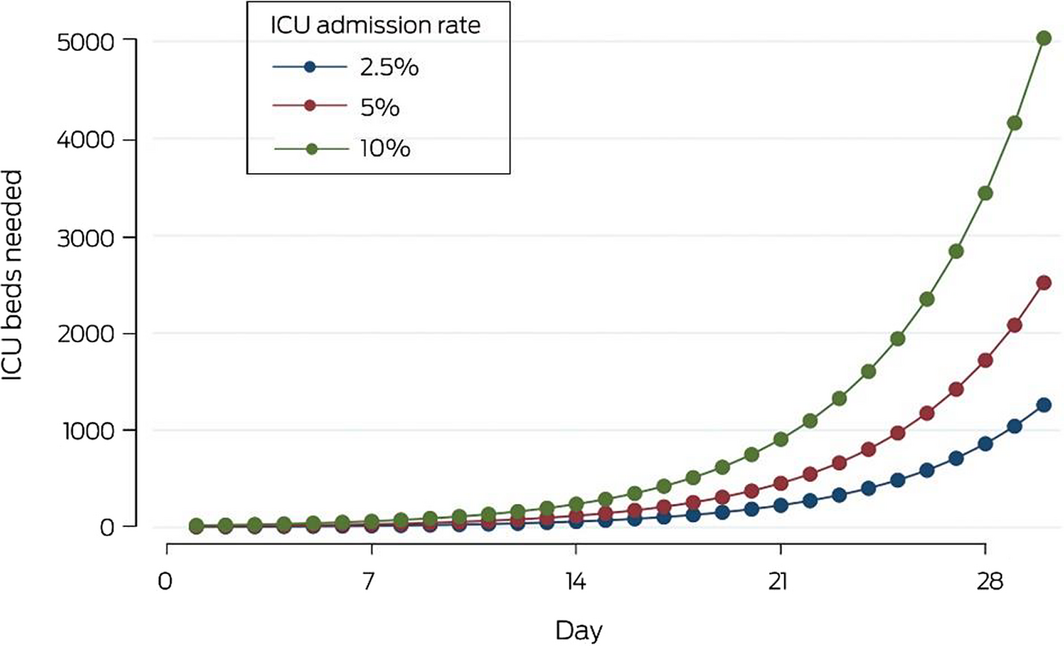
In our exponential growth scenario, commencing with 100 confirmed cases on day 1, 31 ICU beds would be required by day 7 and 119 by day 14 (Box 1). In sensitivity analyses, ICU bed capacity is sufficient even after 30 days if the ICU admission rate is reduced to 2.5%, but would be exceeded by day 26 were the ICU admission rate as high as 10%. It is important to note that our model describes a particularly serious scenario, and that actual outcomes will be modified by parameters not included in the model, including potential lags between diagnosis, hospital admission, and transfer to intensive care, and the proportion of true positive results among people tested for infecton.
Is the modelled scenario plausible?
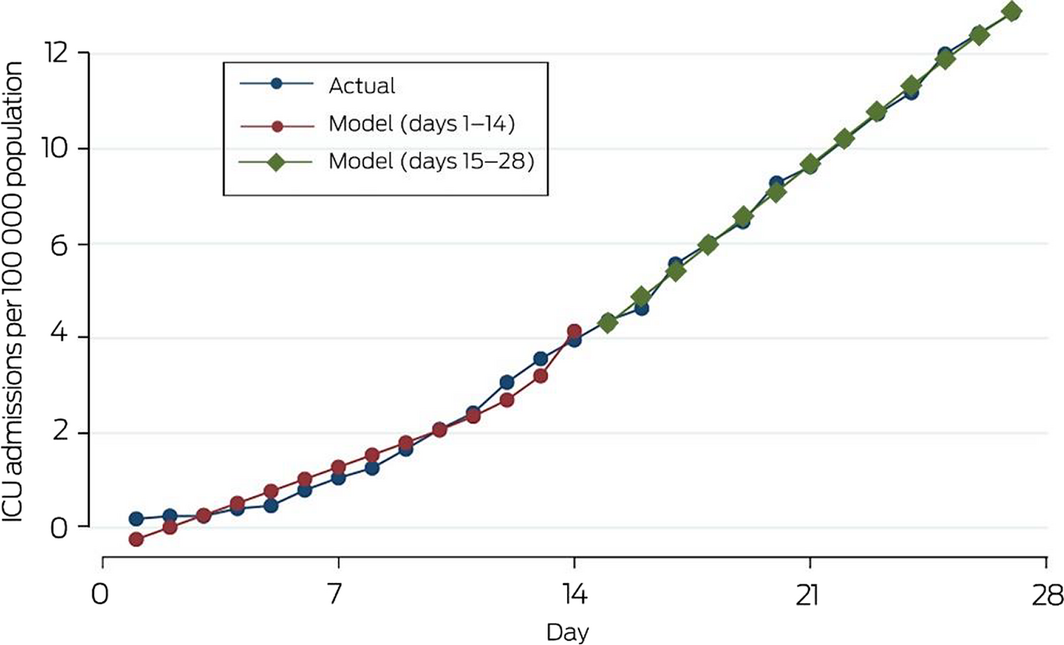
To evaluate how realistic the uninterrupted exponential growth scenario is, we compared exponential and linear growth models with recent data for the Lombardy in Italy.9 Using piecewise regression models, the increase in the number of ICU patients during days 1–14 was exponential (R2 = 0.96); from day 15, ICU admissions continued to rise steeply, but the increase was linear (R2 = 0.99) (Box 2).
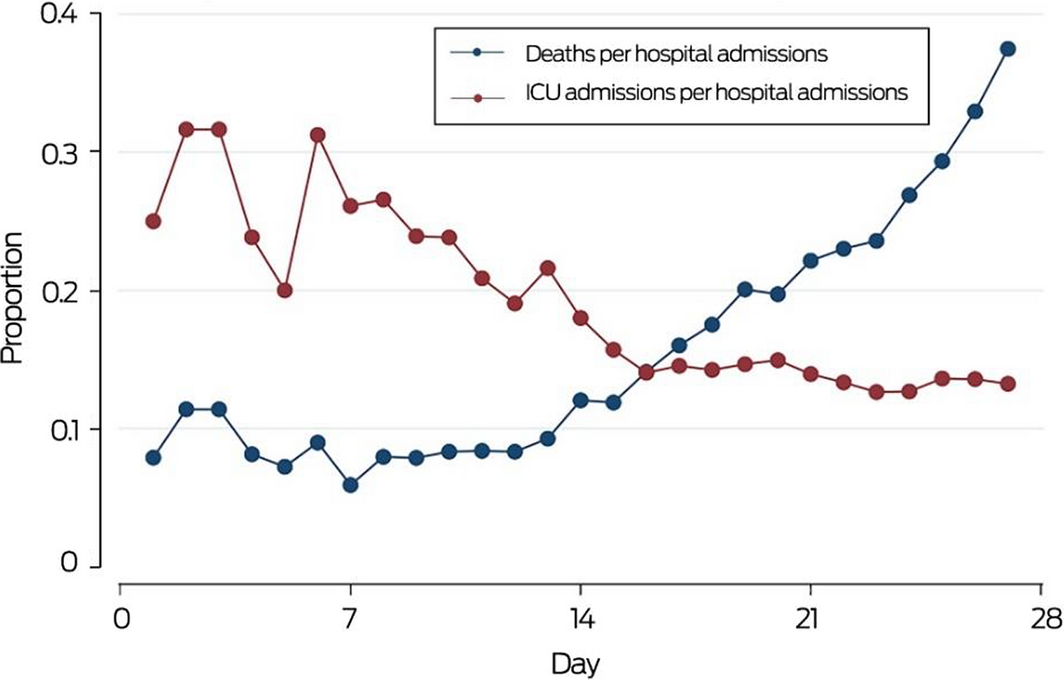
To determine the reason for the change in growth rate at day 15, we compared the ICU admission and mortality rates for patients hospitalised with COVID‐19. The mortality rate during days 1–14 was fairly constant at about 8.8%, but rose dramatically from day 15 to a mean 23%. Most deaths during the first 14 days were probably of patients in intensive care, but we suspect that from day 15 patients died partly because of the lack of access to ICU beds as demand exceeded the capacity of the system to provide them, as indicated by the fall in ICU admission rate (Box 3).
Conclusion
While the assumptions of our model can be debated, the exponential increase in Australian cases until late March suggested that it described a realistic clinical scenario consistent with overseas data available at that time.
The exponential increase in case numbers and subsequent demand for ICU beds could have overwhelmed the capacity of even the largest Australian hospitals if SARS‐CoV‐2 transmission had not been as drastically reduced as it appears to have been by the successful public health measures enacted by the federal and state governments and the adherence to these measures by the Australian public.
The rate of ICU admissions per positive case may be lower in Australia than reported for Italy and China — because of healthier underlying demographic conditions, a greater number of detected milder cases, or both — but this would not change the overall implications of the model.
Australia must maintain measures to strictly control the rate of new cases and continue to improve our ICU surge capacity, lest we squander the chance to avoid an Italian fate.
Received 24 March 2020, accepted 15 April 2020
- 1. Speciale A, Lepido D, Kresege N. Virus spread pushes Italian hospitals toward breaking point. Bloomberg [online], 10 Mar 2020. https://www.bloomberg.com/news/articles/2020-03-10/virus-spread-pushes-italian-hospitals-toward-breaking-point (viewed Mar 2020).
- 2. Remuzzi A, Remuzzi G. COVID‐19 and Italy: what next? Lancet 2020; 395: 1225–1228.
- 3. Ferguson NM, Laydon D, Nedjati‐Gilani G, et al; Imperial College COVID‐19 Response Team. Impact of non‐pharmaceutical interventions (NPIs) to reduce COVID‐19 mortality and healthcare demand. 16 Mar 2020. https://www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-NPI-modelling-16-03-2020.pdf (viewed Mar 2020).
- 4. Little JDC, Graves SC. Little's law. In: Chhajed D, Lowe TJ, editors. Building intuition: insights from basic operations management models and principles (International series in operations research and management science, 115). Boston (MA): Springer, 2008: 81–100.
- 5. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID‐19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020; 323: 1239–1242.
- 6. O'Brien J. Coronavirus (COVID‐19) in Australia [online]. https://www.covid19data.com.au (viewed 23 Mar 2020).
- 7. Litton E, Bucci T, Chavan S, et al. Surge capacity of intensive care units in case of acute increase in demand caused by COVID‐19 in Australia. Med J Aust 2020; 212: 463–467.
- 8. Higgie M, Kahn A. Without serious action, Australia may run out of intensive care beds by early April. Medium [online], updated 19 Mar 2020. https://medium.com/@megan.higgie/without-serious-action-australia-will-run-out-of-intensive-care-beds-between-7-and-10-april-59f83b52756e (viewed Mar 2020).
- 9. Kumar SR. COVID‐19 in Italy. Kaggle [online]. https://www.kaggle.com/sudalairajkumar/covid19-in-italy (viewed 19 Mar 2020).





No relevant disclosures.