The known The burden of cardiovascular disease (CVD) in Australia is disproportionately high for Aboriginal and Torres Strait Islander people. Current guidelines recommend assessing absolute CVD risk in this population in those aged 35–74 years.
The new 15.7% of Aboriginal and Torres Strait Islander Australians aged 35–74 years were at high primary absolute CVD risk; 9.6% had prior CVD. 1.1% of 18–24-year-olds and 4.7% of 25–34-year-olds were at high primary risk. Lipid-lowering therapy was not used by most of those at high risk.
The implications CVD risk assessment and management guidelines for Aboriginal and Torres Strait Islander Australians need to be revised to better target efforts to reduce CVD-associated morbidity and mortality in this population.
Cardiovascular disease (CVD) is a leading cause of disease burden worldwide. In almost all industrialised countries, the risk of CVD is higher for indigenous than non-indigenous populations, including Native American, Canadian First Nation, Māori, and Australian Aboriginal and Torres Strait Islander peoples.1-5 CVD is responsible for 21% of the fatal disease burden among Aboriginal and Torres Strait Islander people, and is the largest contributor to the health gap between Indigenous and non-Indigenous Australians.6 Hospitalisation rates for coronary heart disease are 7–8 times higher for Aboriginal and Torres Strait Islander people aged 25–44 years than for non-Indigenous Australians in this age group, and 52% of Aboriginal and Torres Strait Islander people hospitalised for CVD are under 55, compared with 17% of non-Indigenous patients.7
CVD mortality in Australia has declined by about 80% since peaking in 1968.8 Australian guidelines for preventing CVD and those from other countries recommend an absolute risk approach to assessment and management because it is cost-effective and is associated with less under- and overtreatment than strategies based on single risk factors.9-12 An absolute risk approach integrates data for multiple risk factors to determine an individual’s level of risk of a CVD event within a given time period.11 Best practice management of people identified as being at high absolute CVD risk — in Australia, those with a greater than 15% risk of a CVD event within 5 years according to clinical criteria or the Framingham risk equation — includes combined lipid- and blood pressure-lowering therapies and lifestyle modification.11 Population-level data on absolute CVD risk and levels of treatment can inform health care programs, policy, and planning, including that of large scale preventive treatment.13
Population data on absolute CVD risk and management are not available for any indigenous peoples, and it is therefore unclear how CVD prevention and treatment in these often underserved populations can be optimised. Australian guidelines recommend that Aboriginal and Torres Strait Islander people aged 35–74 years should be assessed for absolute CVD risk.11 As there are no national population-based data on absolute CVD risk in Aboriginal and Torres Strait Islander Australians, the age cut-off for assessment is consensus- rather than evidence-based.
We therefore quantified absolute CVD risk among Aboriginal and Torres Strait Islander people and lipid-lowering medication use according to absolute risk, with the aim of informing prevention research, policy, and practice.
Methods
Contribution of the Aboriginal Reference Group for Cardiovascular Health
An Aboriginal Reference Group for Cardiovascular Health provides expertise and ongoing advice to the research team’s Aboriginal cardiovascular research program. Members of the Group are Aboriginal people who have expertise in research, health service, community partnerships and/or lived experience of CVD. The Group played a key role in focusing the aims of this paper and the interpretation of study findings.
Study population
The study population comprised participants aged 18–74 years who provided biomedical data for the National Aboriginal and Torres Strait Islander Health Measures Survey (NATSIHMS) component of the Australian Bureau of Statistics (ABS) 2012–13 Australian Aboriginal and Torres Strait Islander Health Survey (AATSIHS).14 (Box 1, online Appendix).
Data and variables
Socio-demographic characteristics, medical history (including prior CVD), and health behaviour information were gathered by interview. Participants were deemed to have had a previous CVD event if they responded affirmatively to the question “Including any conditions which can be controlled with medications, have you ever been told by a doctor or nurse that you have any heart or circulatory conditions?” and then reported ischaemic heart disease, heart failure, oedema, other heart disease (including atrial fibrillation/flutter), cerebrovascular disease, or diseases of arteries, arterioles and capillaries.
Height, weight, waist circumference, and systolic and diastolic blood pressure were measured. Fasting blood and urine samples were collected and assayed with standard techniques for evidence of diabetes and chronic kidney disease.14 A participant was deemed to have diabetes if ever told by a doctor or nurse that they had diabetes and they were taking diabetes medication (insulin or tablets), their fasting plasma glucose level was at least 7.0 mmol/L, or their glycated haemoglobin (HbA1c) level was at least 48 mmol/mol. Participants were deemed to have moderate or severe chronic kidney disease if their estimated glomerular filtration rate was below 45 mL/min/1.73m2. Microalbuminuria was defined by an albumin/creatinine ratio of 2.5–25 mg/mol (men) or 3.5–35 mg/mol (women).
Information on medication use was not collected as part of the survey, but participants who agreed to blood collection were asked to complete a three-item questionnaire that included the question, “Do you regularly take prescription medication for any of these conditions: high cholesterol, diabetes, reduced kidney function, reduced liver function?” This information was available for participants who provided fasting blood samples (69.6% of study participants aged 35–74 years). Information on blood pressure medications was not collected. Details on derived variables are included in the online Appendix.
Absolute risk of a primary CVD event in the next 5 years was estimated by the ABS with the Australian National Vascular Disease Prevention Alliance (NVDPA) risk assessment and risk management algorithm (http://www.cvdcheck.org.au); this encompasses both clinical assessment of risk and assessment with the Framingham CVD risk equation of those not at high risk according to clinical criteria.11,15 Based on the algorithm, participants in the study were categorised as being at low (< 10%), moderate (10–15%) or high (> 15%) absolute risk of a primary CVD event (online Appendix).
National expert opinion-informed guidelines recommend that the absolute CVD risk algorithm be applied to Aboriginal and Torres Strait Islander people aged 35–74 years.11 Results are therefore presented separately for those aged 35–74 years (people aged 75 or more are automatically classified as being at high risk and were excluded from our study), as well as for a range of age groups.
Statistical methods
All analyses were carried out in the ABS Remote Access Data Laboratory (http://www.abs.gov.au/websitedbs/D3310114.nsf/home/CURF:+Remote+Access+Data+Laboratory+(RADL)), with approval from the ABS to access the data in accordance with the Census and Statistics Act 1905 (Cwlth). Analyses accounted for the complex sampling strategy and survey non-response by applying appropriate weights to produce estimates that are representative of the Aboriginal and Torres Strait Islander population nationally. The population-weighted proportions of all people aged 18–74 years at high, moderate and low absolute CVD risk or with prior CVD were calculated, by sex and age group. The weighted proportions of individuals aged 35–74 years who reported regular use of prescription cholesterol-reducing medication were estimated according to absolute CVD risk and prior CVD. Confidence intervals (CIs) were calculated for all proportions (online Appendix).
Ethics approval
Ethics approval for the NATSIHMS data collection was provided by the Australian Government Department of Health and Ageing Departmental Ethics Committee (reference, 7/2011). Approval for our analyses was provided by the Australian National University Human Research Ethics Committee (reference, 2014/208) and the Aboriginal Health and Medical Research Council of New South Wales (reference, 1006/14).
Results
Data for absolute CVD risk assessment algorithm components, including factors in the Framingham CVD risk equation, were missing for 403 respondents; they were excluded from analyses. The final sample included 2820 Aboriginal and Torres Strait Islander people aged 18–74 years (1151 men, 1669 women), corresponding to a population-weighted sample of 308 897 Aboriginal and Torres Strait Islander people nationally (155 175 men, 153 722 women).
Included participants did not differ significantly from those with missing data in terms of age, sex, employment or relationship status, socio-economic disadvantage, household income, self-rated health, smoking status, diabetes status, blood pressure, or cholesterol level; however, they did differ in terms of education level and speaking an Indigenous language at home (data not shown).
Prior cardiovascular disease and absolute risk of a primary cardiovascular disease event
Among Aboriginal and Torres Strait Islander people aged 18–74 years, 5.4% (95% CI, 4.1–6.7%; corresponding to an estimated 16 608 adults) had prior CVD, including 9.6% (95% CI, 7.2–12.0%) of those aged 35–74 years (an estimated 15 977 adults).
The prevalence of many of the CVD risk factors included in the NVDPA algorithm was high among Aboriginal and Torres Strait Islander people without prior CVD: 38.3% of those aged 18–74 were current smokers, 15.6% had diastolic blood pressure of 90 mmHg or more, and 10.7% had diabetes (Box 2).
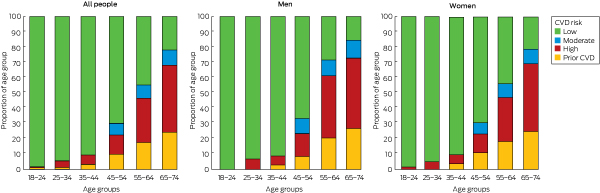
Overall, an estimated 9.8% (95% CI, 8.2–11.4%) of the Aboriginal and Torres Strait Islander population aged 18–74 years were at high absolute risk of a primary CVD event (estimated 30 321 adults), including 15.7% (95% CI, 13.0–18.3%) of those aged 35–74 years (estimated 26 115 adults) (Box 3). The proportion at high primary risk increased with age from 1.1% (95% CI, 0.0–2.5%) of 18–24-year-olds (estimated 760 adults) to 4.7% (95% CI, 2.0–7.5%) of 25–34-year-olds (estimated 3446 adults) to 44.2% (95% CI, 33.1–55.3%) of 65–74-year-olds (estimated 6855 adults) (Box 3, Box 4).
A total of 2.7% (95% CI, 1.8–3.5%) of Aboriginal and Torres Strait Islander people aged 18–74 years (estimated 8216 adults) were at moderate risk of a primary CVD event, including 4.9% (95% CI, 3.3–6.6%) of those aged 35–74 years (estimated 8216 adults); 82.1% (95% CI, 80.4–83.9%; estimated 253 753 adults) were at low primary risk, including 69.8% (66.8–72.8%) of those aged 35–74 years (estimated 116 519 adults) (Box 3).
The distribution of absolute primary CVD risk in the age group recommended for assessment is depicted in Box 5. Of people aged 35–74 years with a high absolute primary CVD risk, 82.6% (or 12.9% of people aged 35–74 years) were determined to be at high risk solely on the basis of clinical criteria and 17.4% (2.7% of people aged 35–74 years) were categorised as being at high risk by the Framingham risk equation. The most common clinical factors that determined high risk were having diabetes with microalbuminuria (45.5% of patients with clinically determined high primary CVD risk), having diabetes and being over 60 (31.4%), total cholesterol level greater than 7.5 mmol/L (17.4%), and moderate to severe kidney disease (9.3%) (online Appendix, table 1).
Cholesterol-lowering medication use
Lipid-lowering therapy was being used by 52.9% (95% CI, 38.2–67.6%) of Aboriginal and Torres Strait Islander people aged 35–74 years with prior CVD (estimated 7050 adults) and by 42.2% (95% CI, 30.5–53.8%) of those at high primary CVD risk (estimated 8596 adults) (Box 6).
Discussion
Levels of CVD morbidity and risk are high among Aboriginal and Torres Strait Islander people. More than one-quarter of Aboriginal and Torres Strait Islander people aged 35–74 years were estimated to be at high risk of a CVD event in the next 5 years: 9.6% with prior CVD and 15.7% at high risk of a primary event, an estimated total of 42 093 people nationally. More than 80% of those at high primary risk aged 35–74 years were identified by clinical criteria, mainly diabetes; further, 58% of those at high primary risk were not receiving recommended lipid-lowering therapy. Below the cut-off age for recommended screening, 1.1% of 18–24-year-olds and 4.7% of 25–34-year-olds were at high primary absolute CVD risk.
This is the first report worldwide of a national absolute CVD risk profile for an indigenous population. The absolute CVD risk profile of Aboriginal and Torres Strait Islander Australians has previously been reported for clinical primary health care populations. One study of Aboriginal clients of primary health care services in remote areas of the Northern Territory found that 9% of 20–34-year-olds, 31% of 35–45-year-olds, 51% of 45–54-year-olds, 72% of 55–64-year-olds, and 83% of 65–74 year-olds were at high absolute CVD risk (5% was added to Framingham risk equation risk scores for Aboriginal people).16 While the risk profile of primary health care clients is important for assessing service needs, these patients are generally at higher risk than the broader population.17 The national profile of absolute CVD risk we report provides evidence for optimising prevention at the population level.
The elevated absolute CVD risk in Aboriginal and Torres Strait Islander we identified can be attributed to the greater prevalence of CVD risk factors in this population than in the general Australian population, particularly of diabetes, dyslipidaemia, chronic kidney disease and smoking.17 Further, the higher absolute CVD risk at younger ages than in the general population17 is consistent with the fact that CVD events and CVD-related deaths occur a mean 10–20 years earlier for Aboriginal and Torres Strait Islander people than for non-Indigenous Australians.7 Higher CVD hospitalisation and mortality rates than for the corresponding general populations have also been reported for Māori, First Nation Canadian, and America Indian and Alaskan Native populations.5,18-20
Current Australian national guidelines define high absolute CVD risk as a greater than 15% probability of a major CVD event in the next 5 years; treatment thresholds are lower in United States (3.5%)12 and British guidelines (5%).21 Assessment according to current guidelines will not identify the substantial number of Aboriginal and Torres Strait Islander people at high primary absolute CVD risk under 35 years of age, compromising the detection of elevated risk and the prevention of CVD in this population. Guidelines for non-Indigenous Australians that recommend assessment of absolute CVD risk from age 45 years are supported by recent evidence that 4.0% of the general Australian population aged 45–54 years and fewer than 2% of those under 45 are at high primary absolute CVD risk.17 On the basis of our findings, a quantitatively equivalent risk assessment regimen for Aboriginal and Torres Strait Islander people would require reducing the minimum assessment age to 25 years or younger, as 4.7% of those aged 25–34 years and fewer than 2% of those under 25 were at high primary absolute CVD risk. However, other considerations, including community acceptability and health service factors, would need to be borne in mind.
In Australia, national guidelines recommend combined lipid- and blood pressure-lowering therapies and lifestyle modifications for people at high absolute CVD risk unless such therapy is contraindicated. Pharmacotherapy is also recommended for those at moderate risk if lifestyle modification does not sufficiently reduce risk within 6 months.11 Our findings indicate substantial undertreatment with lipid-lowering therapies of Aboriginal and Torres Strait Islander people with prior CVD or at high primary risk, consistent with data from primary care settings;22 the level of undertreatment is comparable with that reported for the corresponding general Australian population.17 CVD risk management for Aboriginal and Torres Strait Islander people is most beneficial when delivered in specific Aboriginal and Torres Strait Islander health care settings.23
The NVDPA absolute CVD risk algorithm, including the Framingham equation, has not been validated for Aboriginal and Torres Strait Islander Australians, nor has it been validated for individuals under 30. However, all people aged 18–29 years classified as being at high absolute CVD risk in our study were classified according to clinical criteria (data not shown). Although the Framingham equation is designed for assessing people before they are treated, we analysed data for a population that also included treated individuals. It is therefore likely that we underestimated risk levels, especially given the heavy weighting of age by the algorithm.24 In order to compensate for such underestimation, New Zealand guidelines recommend adding 5% to the absolute CVD risk score of Māori.10 In the absence of a measure specifically calibrated and validated for Aboriginal and Torres Strait Islander Australians, we used the nationally recommended algorithm.11
There is high quality empirical evidence that older people with diabetes, people with high blood pressure and those with chronic kidney disease are at high risk of CVD events.25-27 However, data on the exact probability of CVD events in people with each condition by age are limited, especially at younger ages and for Aboriginal and Torres Strait Islander people. Further validation and calibration of CVD risk assessment for Aboriginal and Torres Strait Islander people is needed to improve CVD prevention.28
Although estimates from the AATSIHS sample are considered to be nationally representative, the survey did not sample individuals from non-private dwellings (eg, hotels, short stay caravan parks, hospitals, prisons). However, our sample was the largest and most representative sample of an indigenous population, in Australia or elsewhere, ever assessed for CVD risk, and population weights were applied to achieve reliable estimates. The overall response rate for AATSIHS was 80% and that for NATSIHMS 40% (ranging from 28% in non-remote to 56% in remote locations14), comparable with the 37% response rate for the equivalent survey in the general population.29 Further, certain data elements were based on self-reports. Greater than 90% agreement between self-reported and formal medication review data on the use of lipid-lowering therapies has been reported for the general US and Australian populations;30,31 specific information for the Aboriginal and Torres Strait Islander population is not available. Medications data were not available for some respondents, and data on lipid-lowering medications were more frequently missing for smokers and participants with greater levels of disadvantage, those speaking an Indigenous language at home, and people with poorer health (data not shown). Overall, it is likely we underestimated the proportion of respondents being treated. In contrast to the general Australian population, comprehensive quantification of recommended prescribed treatments according to absolute risk was not possible, as a full medications review was not included in the AATSIHS.14
Conclusion
The absolute risk of CVD among Aboriginal and Torres Strait Islander people is high, consistent with the high incidence of CVD in this population and in indigenous populations elsewhere. High absolute risk is evident at younger ages in the Aboriginal and Torres Strait Islander population than in the general population, and assessment according to current Australian guidelines is likely to miss a substantial number of people under 35 at high risk. We found evidence of widespread undertreatment of people at risk, which is of greater consequence in groups at higher risk, including indigenous populations. Best practice treatment according to absolute CVD risk would prevent many CVD events, including CVD-related deaths, among Aboriginal and Torres Strait Islander people. A number of policy and practice initiatives have been implemented to improve the uptake of absolute CVD risk assessment and management according to absolute CVD risk, including the introduction of two national Key Performance Indicators for Aboriginal and Torres Strait Islander primary health care related to absolute CVD risk assessment32 and several state-level programs.33 Given the significant contribution of CVD to the burden of disease experienced by Aboriginal and Torres Strait Islander Australians and indigenous people internationally, increasing the quality of our data and improving prevention with an absolute CVD risk approach must be priorities.
Box 1 – Recruitment of the study population for the investigation of absolute cardiovascular disease (CVD) risk among Aboriginal and Torres Strait Islander Australians
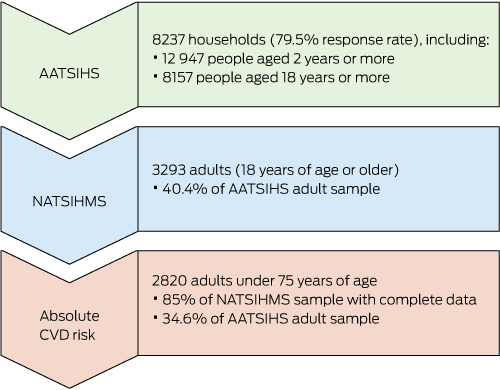
AATSIHS = Australian Aboriginal and Torres Strait Islander Health Survey (2012–13); NATSIHMS = National Aboriginal and Torres Strait Islander Health Measures Survey.
Box 2 – Weighted estimated prevalence of cardiovascular disease (CVD) risk factors included in the National Vascular Disease Prevention Alliance algorithm among Aboriginal and Torres Strait Islander people without prior CVD, by age group
|
|
Age group (years) |
Total |
|||||||||||||
|
18–24 |
25–34 |
35–44 |
45–54 |
55–64 |
65–74 |
||||||||||
|
|
|||||||||||||||
|
Smoking status |
|
|
|
|
|
|
|
||||||||
|
Never smoked |
43.8% |
37.7% |
35.6% |
25.4% |
30.1% |
34.1% |
35.9% |
||||||||
|
Ex-smoker |
18.2% |
14.9% |
31.5% |
34.3% |
37.3% |
46.6% |
25.8% |
||||||||
|
Current smoker |
37.9% |
47.4% |
32.9% |
40.3% |
32.6% |
19.3% |
38.3% |
||||||||
|
Systolic blood pressure |
|
|
|
|
|
|
|
||||||||
|
< 120 mmHg |
63.4% |
64.1% |
57.5% |
40.7% |
30.8% |
17.0% |
54.0% |
||||||||
|
120 to < 140 mmHg |
34.5% |
29.4% |
33.0% |
40.7% |
38.7% |
45.0% |
34.7% |
||||||||
|
140 to < 180 mmHg |
2.1% |
6.4% |
9.5% |
16.3% |
30.2% |
36.5% |
10.8% |
||||||||
|
≥ 180 mmHg |
0 |
< 0.1% |
< 0.1% |
2.2% |
0.3% |
1.6% |
0.5% |
||||||||
|
Diastolic blood pressure |
|
|
|
|
|
|
|
||||||||
|
< 90 mmHg |
93.4% |
86.8% |
82.7% |
74.1% |
76.9% |
82.7% |
84.4% |
||||||||
|
90–< 110 mmHg |
6.5% |
12.2% |
16.4% |
24.9% |
22.6% |
17.3% |
14.9% |
||||||||
|
≥ 110 mmHg |
0.1% |
1.1% |
1.0% |
1.0% |
0.5% |
0 |
0.7% |
||||||||
|
Low-density lipoprotein cholesterol |
|||||||||||||||
|
< 2.0 mmol/L |
18.6% |
6.4% |
3.1% |
6.2% |
8.0% |
23.2% |
9.3% |
||||||||
|
2.0–3.5 mmol/L |
67.7% |
76.0% |
66.8% |
51.3% |
68.3% |
64.6% |
66.9% |
||||||||
|
> 3.5 mmol/L |
13.7% |
17.5% |
30.1% |
42.5% |
23.8% |
12.2% |
23.8% |
||||||||
|
High-density lipoprotein cholesterol (HDL-C) |
|||||||||||||||
|
≥ 1.0 mmol/L |
86.4% |
79.3% |
74.1% |
78.5% |
76.7% |
79.5% |
79.4% |
||||||||
|
< 1.0 mmol/L |
13.6% |
20.7% |
25.9% |
21.5% |
23.3% |
20.5% |
20.6% |
||||||||
|
Total cholesterol |
|
|
|
|
|
|
|
||||||||
|
< 4.0 mmol/L |
28.7% |
17.3% |
10.0% |
13.0% |
18.0% |
25.1% |
18.0% |
||||||||
|
4.0–7.5 mmol/L |
70.3% |
82.0% |
88.6% |
83.7% |
79.5% |
74.1% |
80.5% |
||||||||
|
> 7.5 mmol/L |
1.0% |
0.8% |
1.5% |
3.3% |
2.4% |
0.8% |
1.5% |
||||||||
|
Total cholesterol:HDL-C ratio |
|||||||||||||||
|
< 4.5 |
72.4% |
59.6% |
51.8% |
52.1% |
62.2% |
73.1% |
60.4% |
||||||||
|
4.5–< 6 |
21.8% |
29.6% |
28.9% |
33.2% |
28.6% |
15.4% |
27.5% |
||||||||
|
≥6 |
5.8% |
10.7% |
19.3% |
14.7% |
9.2% |
11.5% |
12.1% |
||||||||
|
Diabetes |
0.5% |
4.3% |
10.1% |
15.8% |
32.6% |
47.8% |
10.7% |
||||||||
|
Diabetes with microalbuminuria |
< 0.1% |
1.5% |
2.7% |
5.5% |
16.0% |
20.1% |
4.0% |
||||||||
|
Moderate/severe chronic kidney disease |
0 |
0.5% |
0.8% |
0.5% |
1.8% |
7.1% |
0.8% |
||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 3 – Weighted proportions (with 95% confidence intervals) of the Aboriginal and Torres Strait Islander population in each absolute cardiovascular disease risk category, by age group and sex
|
Age group (years) |
No prior cardiovascular disease (CVD) |
Prior CVD |
|||||||||||||
|
Low absolute CVD risk (< 10%) |
Moderate absolute CVD risk (10–15%) |
High absolute CVD risk (≥ 15%) |
|||||||||||||
|
|
|||||||||||||||
|
Total population |
|
|
|
|
|||||||||||
|
18–24 |
98.5% (96.9–100%)* |
0.0% (0.0–0.0%) |
1.1% (0.0–2.5%)* |
0.4% (0.0–1.3%)* |
|||||||||||
|
25–34 |
94.8% (92.0–97.6%) |
0.0% (0.0–0.0%) |
4.7% (2.0–7.5%) |
0.5% (0.0–1.2%)* |
|||||||||||
|
35–44 |
90.6% (87.7–93.6%) |
0.3% (0.0–0.9%)* |
6.0% (3.4–8.6%) |
3.0% (1.5–4.6%) |
|||||||||||
|
45–54 |
70.1% (63.3–76.9%) |
7.4% (3.7–11.2%) |
12.8% (8.2–17.4%) |
9.7% (5.5–13.9%) |
|||||||||||
|
55–64 |
44.5% (36.6–52.4%) |
8.8% (3.4–14.3%) |
29.1% (21.2–37.0%) |
17.5% (9.5–25.6%) |
|||||||||||
|
65–74 |
21.6% (12.6–30.6%) |
10.1% (3.4–16.7%) |
44.2% (33.1–55.3%) |
24.2% (14.7–33.7%) |
|||||||||||
|
35–74 |
69.8% (66.8–72.8%) |
4.9% (3.3–6.6%) |
15.7% (13.0–18.3%) |
9.6% (7.2–12.0%) |
|||||||||||
|
18–74 |
82.1% (80.4–83.9%) |
2.7% (1.8–3.5%) |
9.8% (8.2–11.4%) |
5.4% (4.1–6.7%) |
|||||||||||
|
Men |
|
|
|
|
|||||||||||
|
18–24 |
99.6% (99.1–100.0%)* |
0.0% (0.0–0.0%) |
0.4% (0.0–0.9%)* |
0.0% (0.0–0.0%) |
|||||||||||
|
25–34 |
95.3% (90.6–100.0%)* |
0.0% (0.0–0.0%) |
4.7% (0.0–9.4%)* |
0.0% (0.0–0.0%) |
|||||||||||
|
35–44 |
91.7% (87.4–96.0%) |
0.2% (0.0–0.5%)* |
6.3% (2.1–10.4%) |
1.9% (0.4–3.3%) |
|||||||||||
|
45–54 |
67.1% (57.4–76.9%) |
9.9% (3.5–16.4%) |
14.6% (7.1–22.1%) |
8.3% (2.4–14.2%) |
|||||||||||
|
55–64 |
29.5% (17.4–41.6%) |
10.4% (2.4–18.4%) |
39.9% (24.9–55.0%) |
20.1% (7.2–33.0%) |
|||||||||||
|
65–74 |
17.1% (4.6–29.7%) |
11.4% (3.3–19.4%) |
45.0% (29.0–61.0%) |
26.5% (12.3–40.8%) |
|||||||||||
|
35–74 |
66.6% (62.3–70.9%) |
6.1% (3.5–8.7%) |
18.1% (13.9–22.3%) |
9.2% (5.9–12.5%) |
|||||||||||
|
18–74 |
81.0% (78.4–83.6%) |
3.3% (1.9–4.6%) |
10.8% (8.3–13.4%) |
4.9% (3.1–6.7%) |
|||||||||||
|
Women |
|
|
|
|
|||||||||||
|
18–24 |
97.3% (94.0–100.0%)* |
0.0% (0.0–0.0%) |
1.9% (0.0–4.7%)* |
0.9% (0.0–2.6%)* |
|||||||||||
|
25–34 |
94.2% (91.4–97.0%) |
0.0% (0.0–0.0%) |
4.8% (2.4–7.3%) |
1.0% (0.0–2.4%)* |
|||||||||||
|
35–44 |
89.6% (85.3–93.9%) |
0.5% (0.0–1.5%)* |
5.7% (2.4–9.0%) |
4.1% (1.5–6.8%) |
|||||||||||
|
45–54 |
73.2% (64.7–81.8%) |
4.7% (1.0–8.4%) |
10.8% (4.9–16.8%) |
11.2% (5.4–17.1%) |
|||||||||||
|
55–64 |
60.4% (49.4–71.3%) |
7.2% (0.3–14.1%) |
17.7% (10.1–25.2%) |
14.8% (6.0–23.5%) |
|||||||||||
|
65–74 |
24.9% (10.9–38.9%) |
9.1% (0.0–19.8%)* |
43.6% (28.5–58.7%) |
22.4% (9.9–34.9%) |
|||||||||||
|
35–74 |
73.0% (68.9–77.2%) |
3.8% (1.8–5.7%) |
13.2% (10.3–16.2%) |
9.9% (7.1–12.8%) |
|||||||||||
|
18–74 |
83.3% (80.9–85.8%) |
2.1% (1.0–3.1%) |
8.8% (7.0–10.6%) |
5.8% (4.3–7.4%) |
|||||||||||
|
|
|||||||||||||||
|
* Confidence interval truncated at 0 or 100%. |
|||||||||||||||
Box 4 – Estimated weighted distribution of 5-year absolute cardiovascular disease (CVD) risk categories for Aboriginal and Torres Strait Islander adults aged 18–74 years, by sex and age group
Box 5 – Estimated weighted distribution of 5-year absolute cardiovascular disease (CVD) risk for Aboriginal and Torres Strait Islander adults aged 35–74 years
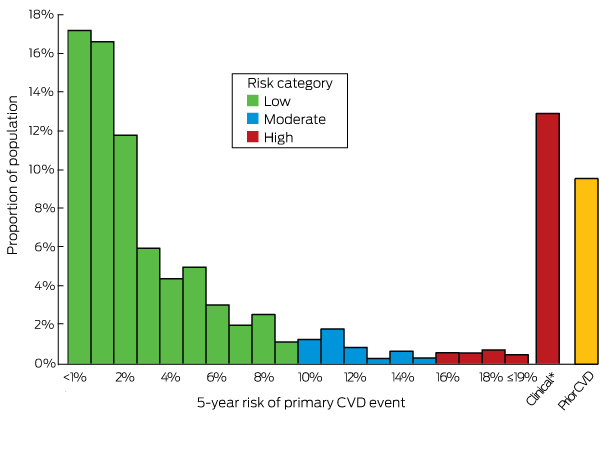
* Assessed as being at high absolute risk according to clinical criteria.
Box 6 – Weighted estimated proportions (with 95% confidence intervals) of Aboriginal and Torres Strait Islander adults aged 35–74 years who reported regularly using prescription medications to treat high cholesterol, by prior cardiovascular disease (CVD) status and 5-year absolute primary CVD risk
|
|
No prior CVD |
Prior CVD |
|||||||||||||
|
Low absolute CVD risk (< 10%) |
Moderate absolute CVD risk (10–15%) |
High absolute CVD risk (≥ 15%) |
|||||||||||||
|
|
|||||||||||||||
|
Lipid medication |
12.9% |
22.5% |
42.2% |
52.9% |
|||||||||||
|
No lipid medication |
87.1% |
77.5% |
57.8% |
47.1% |
|||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Received 16 September 2017, accepted 25 January 2018
- Bianca Calabria1,2
- Rosemary J Korda1
- Raymond W Lovett1,3
- Peter Fernando4
- Tanya Martin5
- Leone Malamoo1
- Jennifer Welsh1
- Emily Banks1,4
- 1 National Centre for Epidemiology and Population Health, Research School of Population Health, Australian National University, Canberra, ACT
- 2 National Drug and Alcohol Research Centre, University of New South Wales, Sydney, NSW
- 3 Australian Institute of Aboriginal and Torres Strait Islander Studies, Canberra, ACT
- 4 Sax Institute, Sydney, NSW
- 5 Poche Centre for Indigenous Health, University of Sydney, Sydney, NSW
We thank the participants of the AATSIHS 2012–13 and NATSIHMS 2012–13, and the Australian Government and the Australian Bureau of Statistics for supporting biomedical data collection and the NATSIHMS. We thank investigators in the National Health and Medical Research Council (NHMRC) Partnership Project and from the National Heart Foundation for their feedback on preliminary findings, and Cate D’Este for statistical advice. This investigation was supported by an NHMRC and Heart Foundation of Australia Partnership Project (1092674). Emily Banks is supported by an NHMRC grant (1042717). The funding sources had no role in the study design, collection, analysis or interpretation of the data, in the writing of the article, or in the decision to submit it for publication.
No relevant disclosures.
- 1. GBD 2015 DALYs and HALE collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016; 288: 1603-1658.
- 2. Rhoades DA. Racial misclassification and disparities in cardiovascular disease among American Indians and Alaska Natives. Circulation 2005; 111: 1250-1256.
- 3. Smith ER. The Canadian Heart Health Strategy and Action Plan. Can J Cardiol 2009; 25: 451-452.
- 4. Atzema CL, Khan S, Lu H, et al. Cardiovascular disease rates, outcomes, and quality of care in Ontario Metis: a population-based cohort study. PLoS One 2015; 10: e0121779.
- 5. New Zealand Ministry of Health. Tatau Kahukura: Māori health chart book 2015. 3rd edition. Wellington: Ministry of Health, 2015. https://www.health.govt.nz/publication/tatau-kahukura-maori-health-chart-book-2015-3rd-edition (viewed Apr 2018).
- 6. Australian Institute of Health and Welfare. Australian Burden of Disease Study: fatal burden of disease in Aboriginal and Torres Strait Islander people 2010 (AIHW Cat. No. BOD 2). Canberra: AIHW, 2015.
- 7. Australian Institute of Health and Welfare. Cardiovascular disease, diabetes and chronic kidney disease. Australian facts: Aboriginal and Torres Strait Islander people (AIHW Cat. No. CDK 5). Canberra: AIHW, 2015.
- 8. Australian Institute of Health and Welfare. Cardiovascular disease: Australian facts 2011 (AIHW Cat. No. CVD 53). Canberra: AIHW, 2011.
- 9. Cobiac LJ, Magnus A, Lim S, et al. Which interventions offer best value for money in primary prevention of cardiovascular disease. PLoS One 2012; 7: e41842.
- 10. New Zealand Guidelines Group. Cardiovascular risk assessment and diabetes screening. In: New Zealand Primary care handbook 2012. 3rd ed. Wellington: NZGG, 2012. https://www.health.govt.nz/publication/new-zealand-primary-care-handbook-2012 (viewed Apr 2018).
- 11. National Vascular Disease Prevention Alliance. Guidelines for the management of absolute cardiovascular disease risk. Canberra: National Vascular Disease Prevention Alliance, 2012. https://www.heartfoundation.org.au/images/uploads/publications/Absolute-CVD-Risk-Full-Guidelines.pdf (viewed Apr 2018).
- 12. Goff DC, Lloyd-Jones DM, Bennett G, et al. ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2013; 129 (25 Suppl 2): S49-S73.
- 13. Pencina MJ, Navar-Boggan AM, D’Agostino RB, et al. Application of new cholesterol guidelines to a population-based sample. N Engl J Med 2014; 370: 1422-1431.
- 14. Australian Bureau of Statistics. 4727.0.55.002. Australian Aboriginal and Torres Strait Islander Health Survey: users’ guide, 2012–13. Nov 2013. http://www.abs.gov.au/AUSSTATS/abs@.nsf/Latestproducts/4727.0.55.002Main%20Features12012-13?opendocument&tabname=Summary&prodno=4727.0.55.002&issue=2012-13&num=&view= (viewed Apr 2018).
- 15. D’Agostino RB, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation 2008; 117: 743-753.
- 16. Burgess CP, Sinclair G, Ramjan M, et al. Strengthening cardiovascular disease prevention in remote Indigenous communities in Australia’s Northern Territory. Heart Lung Circ 2015; 24: 450-457.
- 17. Banks E, Crouch S, Korda R, et al. Absolute risk of cardiovascular disease events, and blood pressure- and lipid-lowering therapy in Australia. Med J Aust 2016; 204: 320.e1-e.8. <MJA full text>
- 18. Young TK. Cardiovascular health among Canada’s aboriginal populations: a review. Heart Lung Circ 2012; 21: 618-622.
- 19. Tjepkema M, Wilkins R, Goedhuis N, Pennock J. Cardiovascular disease mortality among First Nations people in Canada, 1991–2001. Chronic Dis Inj Can 2012; 32: 200-207.
- 20. Centers for Disease Control and Prevention. Health, United States, 2015, table 19. Leading causes of death and numbers of deaths, by sex, race, and Hispanic origin: United States, 1980 and 2014. http://www.cdc.gov/nchs/hus/contents2015.htm#019 (viewed Sept 2016).
- 21. JBS3 Board. Joint British Societies’ consensus recommendations for the prevention of cardiovascular disease (JBS3). Heart 2014; 100 Suppl 2: ii1-ii67.
- 22. Peiris DP, Patel AA, Cass A, et al. Cardiovascular disease risk management for Aboriginal and Torres Strait Islander peoples in primary health care settings: findings from the Kanyini Audit. Med J Aust 2009; 191: 304-309. <MJA full text>
- 23. Ong K, Carter R, Vos T, et al. Cost-effectiveness of interventions to prevent cardiovascular disease in Australia’s Indigenous population. Heart Lung Circ 2014; 23: 414-421.
- 24. Wang Z, Hoy WE. Is the Framingham coronary heart disease absolute risk function applicable to Aboriginal people? Med J Aust 2005; 182: 66-69. <MJA full text>
- 25. The Emerging Risk Factors Collaboration. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 2010; 375: 2215-2222.
- 26. Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet 2014; 383: 1899-1911.
- 27. Chronic Kidney Disease Prognosis Consortium. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet 2010; 375: 2073-2081.
- 28. Hua X, McDermott R, Lung T, et al. Validation and recalibration of the Framingham cardiovascular disease risk models in an Australian Indigenous cohort. Eur J Prev Cardiol 2017; 24: 1660-1669.
- 29. Australian Bureau of Statistics. 4363.0.55.001. Australian Health Survey: users’ guide, 2011–13. June 2013. http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/F87826FDF716EB94CA257B8D00229E83?opendocument (viewed Apr 2018).
- 30. Drieling RL, LaCroix AZ, Beresford SAA, et al. Validity of self-reported medication use compared with pharmacy records in a cohort of older women: findings from the Women’s Health Initiative. Am J Epidemiol 2016; 184: 233-238.
- 31. Gnjidic D, Du W, Pearson SA, et al. Ascertainment of self-reported prescription medication use compared with pharmaceutical claims data. Public Health Res Pract 2017; 27: 27341702.
- 32. Australian Institute of Health and Welfare. National Key Performance Indicators for Aboriginal and Torres Strait Islander primary health care: results from June 2016. (AIHW Cat. No. IHW 177; National Key Performance Indicators for Aboriginal and Torres Strait Islander Primary Health Care Series No. 4). Canberra: AIHW, 2017.
- 33. Burgess CP, Sinclair G, Ramjan M, et al. Strengthening cardiovascular disease prevention in remote Indigenous communities in Australia's Northern Territory. Heart Lung Circ 2015; 24: 450-457.





Abstract
Objective: To quantify absolute cardiovascular disease (CVD) risk in Aboriginal and Torres Strait Islander people and their use of lipid-lowering therapies.
Design, participants: Cross-sectional analysis of nationally representative data from 2820 participants aged 18–74 years who provided biomedical data for the National Aboriginal and Torres Strait Islander Health Measures Survey component of the 2012–13 Australian Aboriginal and Torres Strait Islander Health Survey.
Main outcome measures: Prior CVD and use of lipid-lowering medications were ascertained at interview. 5-year absolute risk of a primary CVD event was calculated with the Australian National Vascular Disease Prevention Alliance algorithm, with categories low (< 10%), moderate (10–15%) and high risk (> 15%).
Results: Among participants aged 35–74 years, 9.6% (95% CI, 7.2–12.0%) had prior CVD; 15.7% (95% CI, 13.0–18.3%) were at high, 4.9% (95% CI, 3.3–6.6%) at moderate, and 69.8% (95% CI, 66.8–72.8%) at low absolute primary CVD risk. 82.6% of those at high primary risk were identified on the basis of clinical criteria. High primary absolute risk affected 1.1% (95% CI, 0.0–2.5%) of 18–24-year-olds, 4.7% (95% CI, 2.0–7.5%) of 25–34-year-olds, and 44.2% (95% CI, 33.1–55.3%) of 65–74-year-olds. Lipid-lowering therapy was being used by 52.9% (95% CI, 38.2–67.6%) of people aged 35–74 years with prior CVD and by 42.2% (95% CI, 30.5–53.8%) of those at high primary CVD risk.
Conclusion: Absolute CVD risk is high among Aboriginal and Torres Strait Islander people, and most of those at high risk are undertreated. Substantial proportions of people under 35 years of age are at high risk, but are not targeted by current guidelines for absolute CVD risk assessment, compromising CVD prevention in this population.