The known Falls are the leading cause of injury-related hospitalisations of Aboriginal people in New South Wales.
The new The patterns of injury and outcomes of fall injury hospitalisations of older Aboriginal people were different to those of other older Australians. A higher proportion of Aboriginal patients had been hospitalised for fall-related non-fracture injuries; their hospital stay was shorter and 30-day mortality lower. The age-standardised rate of fall-related injury hospitalisations was greater for Aboriginal than for non-Indigenous people.
The implications Different approaches may be required to prevent and treat fall-related injuries to older Aboriginal people.
Falls are responsible worldwide for 5–8% of all hospitalisations of people aged 65 years or more; hip fracture is the most common injury.1,2 In Australia, fall injury hospitalisations are less prevalent (2.7% of hospitalisations), with injuries to the hip or thigh being the most common.3 Falls are the leading cause of injury hospitalisations for Aboriginal and Torres Strait Islander people in New South Wales.4 The number of fall-related injuries to older Aboriginal Australians increased from 2007–08 to 2010–11 by an average of 10.2% per year; the average annual increase for all older Australians was 4.3%.3
Severe fall injuries in older people are associated with reduced mobility, loss of independence, and, for some, the need to enter residential care.5 For older Aboriginal people, this potentially entails being separated from home country, community, and culture. Despite the growing rates of fall injury among older Aboriginal Australians, little is known about their injury profile, hospitalisation characteristics, or outcomes, or about whether they differ from those of the older Australian population overall.
In this study, our aim was to compare the socio-demographic characteristics and type of injury sustained, use of hospital resources and rates of hospitalisation by injury type, and survival following fall injuries to older Aboriginal people and non-Indigenous Australian people hospitalised for fall-related injuries.
Methods
Data source and linkage
Two data sources were linked for this study: the NSW Admitted Patient Data Collection (APDC), and death records from the NSW Register of Births, Deaths and Marriages. The APDC is a census of all admitted patient services provided by all 428 NSW hospitals, of which 55% are public.6 Details of each hospitalisation are coded according to the Australian modification of the International Statistical Classification of Diseases and Related Problems, 10th revision (ICD-10-AM).7 Probabilistic linkage of the data extracts was performed by the NSW Centre for Health Record Linkage (CHeReL, http://www.cherel.org.au). As 95.4% of the NSW Indigenous population is Aboriginal,8 this population is referred to as “Aboriginal” in this article.
Case selection
We included all 234 979 cases of people aged 50 years or more who were admitted to a NSW hospital for a fall-related injury between 1 January 2003 and 31 December 2012. Fall injury cases were identified by an ICD-10-AM principal diagnosis code of S00–T75 or T79, and a principal external cause code of W00–W19. Defining “older” in this study as being at least 50 years of age allowed us to directly compare our results with data published by the Australian Institute of Health and Welfare (AIHW).
Indigenous status is coded for each hospital episode of care in the APDC dataset. A person was classified as Aboriginal if they were listed as Aboriginal or Torres Strait Islander in the hospitalisation record for a single episode of care, at least once if there had been two episodes of care, or at least twice if there had been three or more episodes of care. This algorithm is recommended when linking data for Aboriginal and Torres Strait Islander peoples in NSW population datasets, to minimise the effects of reporting, administrative and coding errors.9
Age was categorised into 5-year brackets. Comorbidities contributing to the Charlson Comorbidity Index were identified with a validated ICD-10 coding algorithm,10 including a 12 -month look-back period.11
Hospital length of stay (LOS) was defined as the number of days between the dates of admission and of final discharge from the health system. Hospitalisations comprising multiple contiguous episodes of care for an injury were counted as one hospital stay. Records with an unusually long LOS (more than three standard deviations above the mean) were excluded as reflecting atypical care practices or possible coding errors.12
Thirty-day mortality was defined as death from any cause within 30 days of admission to hospital following a fall-related injury. Twenty-eight day hospital re-admission was defined as admission to any hospital in NSW for any cause within 28 days of discharge.
Statistical analysis
Differences between Aboriginal and non-Indigenous older Australians in the proportions of type, mechanism, and place of injury were compared in χ2 tests. Mean LOS (with 95% confidence interval [CI]) was calculated, and adjusted for age and sex differences by linear regression; the significance of differences between Aboriginal and non-Indigenous older Australians in mean LOS was assessed in t tests. Thirty-day mortality was calculated for each of the two populations. Age-standardised hospitalisation rates were calculated by dividing the number of hospitalisations in each 5-year age bracket by the NSW population in that age group for the corresponding year, with direct standardisation against the 2001 Australian standard population.13 The age-standardised rate ratio (SRR) comparing the rates for Aboriginal and non-Indigenous older Australians was calculated (with 95% CI), assuming a Poisson distribution. We assessed the statistical significance of changes in admission rates over time by negative binomial regression analysis. All statistical analyses were performed in SAS Enterprise Guide 6.1 (SAS Institute).
Ethics approval
Ethics approval for the study was obtained from the NSW Population and Health Service Research Ethics Committee and the Aboriginal Health and Medical Research Council (reference, HREC/13/CIPHS/49).
Results
There were 312 758 fall-related injury hospitalisations for people aged 50 years or more during the 10-year study period (234 979 individual patients), 2660 of which (0.85%) were of Aboriginal people, of whom 2434 (91.5%) were admitted to public hospitals; the proportion of Aboriginal people admitted to private hospitals was lower than for non-Indigenous patients (2.1% v 8.5%; P < 0.001).
Cohort and injury characteristics (Box 1)
Most fall-related injury hospitalisations were of women (55% of Aboriginal patients, 67% of non-Indigenous patients); 74% of hospitalisations of Aboriginal people were of people under 75 years of age, as were 34% of hospitalisations of other older Australians.
The proportion of hospitalisations for fall-related fracture injuries was lower for Aboriginal than for non-Indigenous Australians (49% v 60% of fall-related hospitalisations; P < 0.001), particularly with respect to fall-related hip fractures (10% v 18%; P < 0.001).
The proportion of hospitalisations for fall-related non-fracture injuries was correspondingly higher for Aboriginal than for non-Indigenous Australians (51% v 40%; P < 0.001), particularly for non-fracture injuries to the head and neck (19% v 14%; P < 0.001).
The home was the most common place of injury for both Aboriginal and non-Indigenous patients (47% v 48% of hospitalisations; P = 0.21). The proportion of hospitalisation records listing place of injury as “other/unspecified” was higher for Aboriginal than for non-Indigenous patients (32% v 21%; P < 0.001). A smaller proportion of hospitalisations of Aboriginal patients resulted in re-admission within 28 days (12% v 17% of non-Indigenous patients; P < 0.001).
Length of hospital stay
The mean LOS for a fall injury was 9.1 days for Aboriginal people and 14.0 days for non-Indigenous Australians. LOS was shorter for Aboriginal people for all injury types, with the exception of hip fracture and traumatic brain injury, where there was no difference (Box 2). The rate of self-discharge from hospital was higher for Aboriginal people than for non-Indigenous patients (3.4% v 0.6%; P < 0.001).
Mortality within 30 days of hospital admission
The proportion of hospitalisations followed by death within 30 days of admission was lower for Aboriginal than for non-Indigenous patients (2.9% v 4.2 %; P < 0.001); 30-day mortality for traumatic brain injuries in Aboriginal patients was less than half that for other older Australians (7.8% v 16.2%; P = 0.010). There was no statistically significant difference in mortality following hip and other fracture injuries. The small number of deaths of Aboriginal people precluded statistical adjustment for sex and age (Box 3).
Age-standardised hospitalisation rates
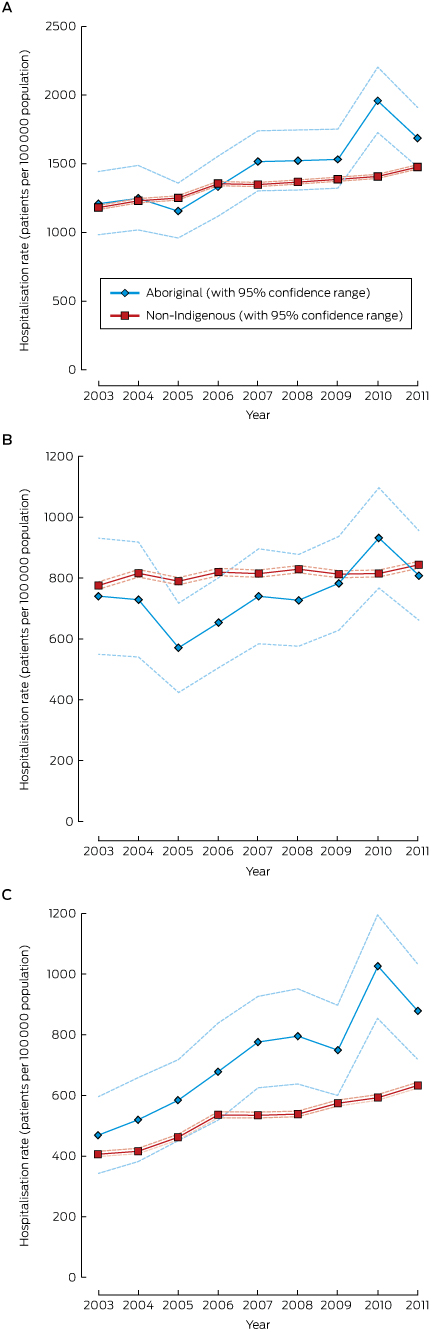
The age-standardised hospitalisation rate for all fall-related injuries was higher for Aboriginal than for non-Indigenous patients overall (SRR, 1.17; 95% CI, 1.11–1.23, P < 0.001); however, the difference in annual rate was statistically significant only for 2010 and 2011 (Box 4). Age-standardised hospitalisation rates for hip fracture were similar for Aboriginal people and non-Indigenous patients (SRR, 0.91; 95% CI, 0.79–1.05; P = 0.19), but for patients with traumatic brain injury the rates were higher for Aboriginal patients (SRR, 1.27; 95% CI, 1.24–1.30; P = 0.026). Hospitalisation rates for both populations increased over time, but the increase was greater for Aboriginal patients (Box 4).
For Aboriginal people, fall injury hospitalisations increased during 2003–2011 at an annual rate of 5.8% (95% CI, 4.0–7.7%; P < 0.001); for non-Indigenous patients, the mean annual increase was 2.5% (95% CI, 2.1–3.0; P < 0.001). Age-standardised rates of hospitalisation of Aboriginal people for fall-related fractures increased at a faster rate (annual increase, 3.0%; 95% CI, 0.5–5.6%; P = 0.020) than for other older Australians (annual increase, 0.7%; 95% CI, 0.3–1.1%; P = 0.001). The rates of hospitalisation for fall-related non-fracture injuries were similar for both populations, but the rate of increase was greater for Aboriginal people (Aboriginal, 9.2%; 95% CI, 6.9–11.5%; P < 0.001; non-Indigenous, 5.6%; 95% CI, 4.6–6.7%; P < 0.001).
Discussion
Most fall-related injury hospitalisations of Aboriginal people were of people under 75. This is consistent with results from previous research in NSW which found that 61% of Aboriginal people hospitalised for fall injuries were 50–64 years old, compared with 23% of non-Indigenous patients.14 For all-cause hospitalisations nationally, 14% of separations of Aboriginal people were for patients aged 65 years or more, compared with 42% of separations for other Australians.15
A lower proportion of Aboriginal than of non-Indigenous people admitted to hospital with a fall-related injury had a fracture injury. This difference, particularly marked for hip fractures, may be linked to higher levels of obesity in the Aboriginal population. An elevated body mass index is reported to increase bone mineral density of the femoral neck in older people, protecting it from fracture.16 Excess fat around the hip also absorbs and diverts energy in the event of an impact.17 Rates of obesity are higher among older Aboriginal people, affecting 75% those aged 55 years or more (v 59% of non-Indigenous Australians).17 The substantial burden of early onset chronic health conditions in Aboriginal populations, coupled with high mortality at younger ages,18 may mean that those who survive to a higher age are the healthiest and strongest members of their population, resulting in fewer hospitalisations for health conditions associated with ageing, such as hip fracture.
The proportion of fall-related non-fracture injury hospitalisations was higher for Aboriginal than for non-Indigenous patients, particularly non-fracture injuries to the head and neck. This type of injury after a fall suggests that neuroprotective reflexes which usually cause the person to break their fall with their arms are impaired.19 An earlier study reported that the rate of head injuries leading to hospitalisation (81% of which were caused by falls) was 1.7 times as high for Aboriginal people aged 60 years or more than for other older Australians.20
Hospital LOS was shorter for all injury types for Aboriginal patients than for non-Indigenous patients. A number of factors make hospitalisation traumatic for Aboriginal people and therefore favour an earlier discharge, including separation from family and community networks, communication and language barriers, and the fear of dying away from home country.20,21 This raises questions about the appropriateness of mainstream health care settings for providing care to Aboriginal people. A small proportion of Aboriginal patients discharged themselves from hospital (3.4%), but this was unlikely to have markedly influenced the overall LOS for this group.
We found that the frequency of death within 30 days of admission was lower for older Aboriginal patients than for non-Indigenous patients. The age distribution of hospitalised patients with a fall injury may have contributed to this finding, with younger Aboriginal people recovering more rapidly than older and frailer non-Indigenous patients.
We also found that hospitalisation rates for fall injuries increased about twice as quickly for Aboriginal people as for other older Australians. This is consistent with the findings of a nationwide study of people aged 65 years and older that reported fall-related injury hospitalisations of Aboriginal people increased during 2007–2011 at 2.4 times the rate for non-Indigenous Australians.22 The treatment-seeking behaviour of Aboriginal and non-Indigenous Australians are strikingly different: Aboriginal people use admitted patient services in public hospitals at four times the rate of other Australians, but are admitted to private hospitals less frequently.23 Past experience of discrimination and communication problems are reported to deter Aboriginal people from contacting mainstream health services.20 Fifty-two Aboriginal Community Controlled Health Services (ACCHSs) operate in NSW,24 many of which have the clinical facilities to treat less severe fall-related injuries. These services potentially offer older Aboriginal people an alternative to the hospital system for treatment.
Strengths and limitations of the study
This is the first study to specifically investigate fall injury hospitalisations and outcomes for older Aboriginal people in NSW. Its population-based nature maximised its statistical strength, and the relatively long study timeframe allowed temporal changes to be assessed. Drawing on information from all hospitalisation records for each individual increased the likelihood that all Aboriginal patients were identified.
Nevertheless, problems with correctly identifying Aboriginal people presenting to health services are likely to have led to underestimating the number of Indigenous patients. An AIHW report released in 2010 noted that 11% of Indigenous people were not identified correctly in their hospitalisation records; however, the level of Indigenous identification increased by 8% in NSW public hospitals between 2005 and 2010.25 This may have contributed to the increase in injury hospitalisation rates being greater for Aboriginal than for non-Indigenous people. The APDC is considered a reliable data source, and is routinely monitored and checked for data quality, but minor discrepancies may be caused by coding, clerical and data conversion errors.
Further research is needed to determine how hospital services could more appropriately care for older Aboriginal people. Our results could inform the design and implementation of fall prevention programs for Aboriginal communities, as we identified specific risk factors associated with falls by older Aboriginal people.
Conclusion
We found different patterns of injury for older Aboriginal people and other older Australians. Fall injury hospitalisation rates rose more rapidly during 2003–2011 for Aboriginal people than for other older people. The difference may have been influenced by the use of Aboriginal-specific health services instead of the general hospital system, historical under-reporting of Aboriginal status on presentation to medical services, and changes in reporting practices.
Box 1 – Demographic and injury characteristics for fall-related injury hospitalisations of people aged 50 years or more, New South Wales, 2003–2012
|
|
Aboriginal Australians |
Non-Indigenous Australians |
P |
||||||||||||
|
|
|||||||||||||||
|
Number of hospitalisations |
2660 |
310 098 |
|
||||||||||||
|
Sex (women) |
1458 (54.8%) |
207 166 (66.8%) |
< 0.001 |
||||||||||||
|
Age group (years) |
|
|
< 0.001 |
||||||||||||
|
50–54 |
549 (20.6%) |
16 127 (5.2%) |
|
||||||||||||
|
55–59 |
418 (15.7%) |
18 827 (6.1%) |
|
||||||||||||
|
60–64 |
382 (14.4%) |
20 623 (6.7%) |
|
||||||||||||
|
65–69 |
324 (12.2%) |
22 007 (7.1%) |
|
||||||||||||
|
70–74 |
296 (11.1%) |
28 021 (9.0%) |
|
||||||||||||
|
75–79 |
231 (8.7%) |
41 636 (13.4%) |
|
||||||||||||
|
80–84 |
210 (7.9%) |
58 942 (19.0%) |
|
||||||||||||
|
85–89 |
157 (5.9%) |
58 968 (19.0%) |
|
||||||||||||
|
≥ 90 |
93 (3.5%) |
44 947 (14.5%) |
|
||||||||||||
|
Number of comorbidities (Charlson Comorbidity Index) |
< 0.001 |
||||||||||||||
|
0 |
1476 (55.5%) |
177 195 (57.1%) |
|
||||||||||||
|
1–2 |
886 (33.3%) |
107 076 (34.5%) |
|
||||||||||||
|
≥ 3 |
298 (11.2%) |
25 827 (8.3%) |
|
||||||||||||
|
Fractures |
|
|
|
||||||||||||
|
All fractures |
1304 (49.0%) |
186 469 (60.2%) |
< 0.001 |
||||||||||||
|
Fracture of head and neck |
48 (1.8%) |
7405 (2.4%) |
0.050 |
||||||||||||
|
Fracture of trunk |
288 (10.8%) |
36 678 (11.8%) |
0.11 |
||||||||||||
|
Fracture of arm |
389 (14.6%) |
54 747 (17.7%) |
< 0.001 |
||||||||||||
|
Fracture of hip |
263 (9.9%) |
57 097 (18.4%) |
< 0.001 |
||||||||||||
|
Fracture of leg |
281 (10.6%) |
27 489 (8.9%) |
0.002 |
||||||||||||
|
Fracture injury, other |
35 (1.3%) |
3053 (1.0%) |
0.08 |
||||||||||||
|
Non-fracture injuries |
|
|
|
||||||||||||
|
All non-fracture injuries |
1356 (51.1%) |
123 629 (39.8%) |
< 0.001 |
||||||||||||
|
Non-fracture injury to the head and neck |
491 (18.5%) |
43 040 (13.9%) |
< 0.001 |
||||||||||||
|
Traumatic brain injury |
128 (4.8%) |
12 301 (4.0%) |
0.026 |
||||||||||||
|
Non-fracture injury of the arm |
199 (7.5%) |
19 375 (6.2%) |
0.009 |
||||||||||||
|
Non-fracture injury of the trunk |
191 (7.2%) |
15 502 (5.0%) |
< 0.001 |
||||||||||||
|
Non-fracture injury of the leg |
308 (11.6%) |
29 558 (9.5%) |
0.003 |
||||||||||||
|
Non-fracture, other |
39 (1.5%) |
3853 (1.2%) |
0.30 |
||||||||||||
|
Mechanism of fall |
|
|
|
||||||||||||
|
Fall on same level (low trauma) |
1395 (52.4%) |
174 224 (56.2%) |
< 0.001 |
||||||||||||
|
Fall involving furniture (low trauma) |
190 (7.1%) |
21 269 (6.9%) |
0.56 |
||||||||||||
|
Fall from one level to another (high trauma) |
372 (14.0%) |
41 798 (13.5%) |
0.45 |
||||||||||||
|
Other/unspecified |
703 (26.4%) |
72 807 (23.5%) |
< 0.001 |
||||||||||||
|
Place of injury |
|
|
|
||||||||||||
|
Home |
1257 (47.3%) |
150 328 (48.5%) |
0.21 |
||||||||||||
|
Residential care institution |
201 (7.6%) |
56 752 (18.3%) |
< 0.001 |
||||||||||||
|
Public area |
350 (13.2%) |
37 071 (12.0%) |
0.06 |
||||||||||||
|
Other/unspecified |
852 (32.0%) |
65 947 (21.3%) |
< 0.001 |
||||||||||||
|
Re-admitted to hospital within 28 days* |
434 (16.6%) |
35 063 (11.5%) |
< 0.001 |
||||||||||||
|
|
|||||||||||||||
|
* Excludes hospitalisations with date of discharge after 3 December 2012. |
|||||||||||||||
Box 2 – Length of hospital stay for fall-related injury hospitalisations of people aged 50 years or more, New South Wales, 2003–2012
|
Injury type |
Mean length of stay (95% CI), days |
P |
Mean length of stay (95% CI), adjusted for age and sex, days |
P* |
|||||||||||
|
Aboriginal Australians |
Non-Indigenous Australians |
Aboriginal Australians |
Non-Indigenous Australians |
||||||||||||
|
|
|||||||||||||||
|
All fall-related injuries |
9.1 (8.5–9.6) |
14.0 (13.9–14.0) |
0.001 |
9.5 (9.3–9.7) |
13.7 (13.7–13.7) |
< 0.001 |
|||||||||
|
Hip fracture |
25.6 (23.0–29.2) |
26.5 (26.3–26.6) |
0.89 |
25.0 (24.8–25.3) |
26.5 (26.5–26.5) |
< 0.001 |
|||||||||
|
All other fractures |
9.9 (9.0–10.8) |
13.7 (13.6–13.8) |
< 0.001 |
9.2 (8.9–9.6) |
13.8 (13.8–13.8) |
< 0.001 |
|||||||||
|
Traumatic brain injury |
9.6 (7.1–12.8) |
12.8 (12.6–13.2) |
0.43 |
10.4 (10.0–10.8) |
12.9 (12.9–12.9) |
< 0.001 |
|||||||||
|
All other non-fracture injuries |
4.4 (3.9–4.9) |
7.1 (7.0–7.2) |
0.006 |
4.8 (4.7–4.9) |
7.1 (7.1–7.2) |
< 0.001 |
|||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 3 – Thirty-day mortality for fall-related injury hospitalisations of people aged 50 years or more, New South Wales, 2003–2012
|
Injury type |
Aboriginal Australians |
Non-Indigenous Australians |
P |
||||||||||||
|
|
|||||||||||||||
|
Number of hospitalisations |
2660 |
310 098 |
|
||||||||||||
|
All fall-related injuries |
76 (2.9%) |
13 034 (4.2%) |
< 0.001 |
||||||||||||
|
Hip fracture |
18 (7.9%) |
4535 (6.8%) |
0.50 |
||||||||||||
|
All other fractures |
22 (2.2%) |
2995 (2.4%) |
0.70 |
||||||||||||
|
Traumatic brain injury |
10 (7.8%) |
1988 (16.2%) |
0.010 |
||||||||||||
|
All other non-fracture injuries |
26 (3.1%) |
3495 (2.1%) |
0.041 |
||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Received 7 October 2016, accepted 21 December 2016
- Caroline Lukaszyk1
- Lara A Harvey2,3
- Catherine Sherrington1
- Jacqueline CT Close2,4
- Julieann Coombes1
- Rebecca J Mitchell2,5
- Robyn Moore6
- Rebecca Ivers1,7
- 1 George Institute for Global Health, University of Sydney, Sydney, NSW
- 2 Falls, Balance and Injury Research Centre, Neuroscience Research Australia, Sydney, NSW
- 3 University of New South Wales, Sydney, NSW
- 4 Prince of Wales Clinical School, Sydney, NSW
- 5 Australian Institute of Health Innovation, Macquarie University, NSW
- 6 Yerin Aboriginal Health Services, Wyong, NSW
- 7 Flinders University, Adelaide, SA
Caroline Lukaszyk was funded by the NSW Ministry of Health through the Aboriginal Injury Prevention and Safety Promotion Demonstration Projects Program. Lara Harvey was funded by a National Health and Medical Research Council Early Career Fellowship. Linkage of data was funded by the Dementia Collaborative Research Centres -; Assessment and Better Care, University of New South Wales. We thank the NSW Ministry of Health and NSW Registry of Births, Deaths and Marriages for providing the hospitalisation and death data extracts, and the Centre for Health Record Linkage (CHeReL) for providing unique patient identifiers used to link the datasets. We also thank the project steering committee for their feedback on the study design and manuscript drafts.
No relevant disclosures.
- 1. Alexander BH, Rivara FP, Wolf ME. The cost and frequency of hospitalization for fall-related injuries in older adults. Am J Public Health 1992; 82: 1020-1023.
- 2. Scott V, Wagar L, Elliott S. Falls and related injuries among older Canadians: fall-related hospitalizations and intervention initiatives. Victoria, BC: Victoria Scott Consulting, 2010. http://www.hiphealth.ca/media/research_cemfia_phac_epi_and_inventor_20100610.pdf (accessed Apr 2017).
- 3. Bradley C. Hospitalisations due to falls by older people, Australia 2009–10 (AIHW Cat. No. INJCAT 146; Injury Research and Statistics Series No. 70). Canberra: AIHW, 2013 http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=60129542822 (accessed Apr 2017).
- 4. New South Wales Ministry of Health. The health of Aboriginal people of NSW: report of the Chief Health Officer 2012. Sydney: Ministry of Health, 2012. http://www.health.nsw.gov.au/epidemiology/Publications/Aboriginal-Health-CHO-report.pdf (accessed Apr 2017).
- 5. Lord SR, Menz HB, Sherrington C, Close JCT. Falls in older people: risk factors and strategies for prevention. Cambridge: Cambridge University Press, 2007.
- 6. Australian Bureau of Statistics. 1368.1. New South Wales Regional Statistics, 2007. NSW Health Department, Admitted Patient Data Collection [webpage]. Apr 2008. http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/1368.1Explanatory%20Notes1452007 (accessed Apr 2017).
- 7. National Centre for Classification in Health. International statistical classification of diseases and related health problems, tenth revision, Australian modification (ICD-10-AM). Sydney: University of Sydney, 2010.
- 8. Australian Bureau of Statistics. 3238.0. Experimental estimates and projections, Aboriginal and Torres Strait Islander Australians, 1991 to 2021. Sept 2009. http://www.abs.gov.au/AUSSTATS/abs@.nsf/allprimarymainfeatures/497290ADDF187134CA257CC900143EAA?opendocument (accessed Apr 2017).
- 9. Centre for Epidemiology and Evidence, Population and Public Health Division. Improved reporting of Aboriginal and Torres Strait Islander peoples on population datasets in New South Wales using record linkage. A feasibility study. Sydney: NSW Ministry of Health, 2012. http://www.health.nsw.gov.au/hsnsw/Publications/atsi-data-linkage-report.pdf (accessed Apr 2017).
- 10. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005; 43: 1130-1139.
- 11. Preen DB, Holman CAJ, Spilsbury K, et al. Length of comorbidity lookback period affected regression model performance of administrative health data. J Clin Epidemiol 2006; 59: 940-946.
- 12. National Health Performance Authority. Hospital performance: length of stay in public hospitals in 2011–12. Technical supplement. Sydney: NHPA, 2013. http://www.myhospitals.gov.au/docs/default-source/our-report-pdfs/HP_LengthOfStay_2011-12_TECH.pdf (accessed Apr 2017).
- 13. Australian Bureau of Statistics. 3101.0. Australian demographic statistics, Dec 2012. Standard population for use in age-standardisation: June 2013. http://www.abs.gov.au/websitedbs/censushome.nsf/home/historicaldata2001?opendocument (accessed May 2017).
- 14. Centre for Aboriginal Health. Mortality and hospitalisation due to injury in the Aboriginal population of New South Wales. Sydney: NSW Department of Health, 2010. http://www.health.nsw.gov.au/aboriginal/Publications/pub-mortality.pdf (accessed Apr 2017).
- 15. Australian Institute of Health and Welfare. Admitted patient care 2014–15: Australian hospital statistics (AIHW Cat. No. HSE 172; Health Services Series No. 68). Canberra: AIHW, 2016. http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=60129554729 (accessed Apr 2017).
- 16. Barrera G, Bunout D, Gattás V, et al. A high body mass index protects against femoral neck osteoporosis in healthy elderly subjects. Nutrition 2004; 20: 769-771.
- 17. Johansson H, Kanis JA, Odén A, et al. A meta-analysis of the association of fracture risk and body mass index in women. J Bone Miner Res 2014; 29: 223-233.
- 18. Australian Bureau of Statistics. 4722.0.55.002. Older Aboriginal and Torres Strait Islander people: a snapshot, 2004–05 [webpage]. May 2007. http://www.abs.gov.au/ausstats/abs@.nsf/mf/4722.0.55.002?OpenDocument (accessed Apr 2017).
- 19. Tinetti ME, Doucette J, Claus E, Marottoli R. Risk factors for serious injury during falls by older persons in the community. J Am Geriatr Soc 1995; 43: 1214-1221.
- 20. Jamieson LM, Roberts-Thomson KF. Hospitalized head injuries among older people in Australia, 1998/1999 to 2004/2005. Inj Prev 2007; 13: 243-247.
- 21. Arkles R, Jackson Pulver Lisa, Robertson H, et al. Ageing, cognition and dementia in Australian Aboriginal and Torres Strait Islander people, a life cycle approach: a literature review. Sydney: Neuroscience Research Australia and Muru Marri Indigenous Health Unit, University of New South Wales, 2010. http://researchdirect.westernsydney.edu.au/islandora/object/uws%3A34258/datastream/PDF/download/citation.pdf (accessed Apr 2017).
- 22. Bradley C. Trends in hospitalisations due to falls by older people, Australia, 1999–00 to 2010–11 (AIHW Cat. No. INJCAT 160; Injury Research and Statistics Series No. 84). Canberra: Australian Institute of Health and Welfare, 2013.
- 23. Australian Institute of Health and Welfare. Access to health services for Aboriginal and Torres Strait Islander people (AIHW Cat. No. IHW 46). Canberra: AIHW, 2011. http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=10737418951 (accessed Apr 2017).
- 24. Australian Government, Department of Health. Aged care service list: New South Wales 2015. Updated Feb 2016. https://agedcare.health.gov.au/ageing-and-aged-care-overview/about-aged-care/aged-care-service-list-new-south-wales (accessed Apr 2017).
- 25. Australian Institute of Health and Welfare. Indigenous identification in hospital separations data-quality report (AIHW Cat. No. HSE 85; Health Services Series No. 35). Canberra: AIHW. http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=6442457092 (accessed Apr 2017).





Abstract
Objectives: To compare the socio-demographic characteristics and type of injury sustained, the use of hospital resources and rates of hospitalisation by injury type, and survival following fall injuries to older Aboriginal people and non-Indigenous Australian people hospitalised for fall-related injuries.
Design: Population-based retrospective cohort data linkage study.
Setting, participants: New South Wales residents aged 50 years or more admitted to a public or private NSW hospital for a fall-related injury during 1 January 2003 – 31 December 2012.
Main outcome measures: Proportions of patients with defined injury types, mean hospital length of stay (LOS), 30-day mortality, age-standardised hospitalisation rates and age-adjusted rate ratios, 28-day re-admission rates.
Results: There were 312 758 fall-related injury hospitalisations for 234 979 individuals; 2660 admissions (0.85%) were of Aboriginal people. The proportion of hospitalisations for fall-related fracture injuries was lower for Aboriginal than for non-Indigenous Australians (49% v 60% of fall-related hospitalisations; P < 0.001). The major injury type for Aboriginal patients was non-fracture injury to head or neck (19% of hospitalisations); for non-Indigenous patients it was hip fractures (18%). Age-adjusted LOS was lower for Aboriginal than for non-Indigenous patients (9.1 v 14.0 days; P < 0.001), as was 30-day mortality (2.9% v 4.2%; P < 0.001). For Aboriginal people, fall injury hospitalisations increased at an annual rate of 5.8% (95% CI, 4.0–7.7%; P < 0.001); for non-Indigenous patients, the mean annual increase was 2.5% (95% CI, 2.1–3.0; P < 0.001).
Conclusions: The patterns of injury and outcomes of fall injury hospitalisations were different for older Aboriginal people and other older Australians, suggesting that different approaches are required to prevent and treat fall injuries.