The known Information on the cause and manner of premature deaths of nursing home residents has been scarce.
The new During 2001–2012, the incidence of external cause deaths in nursing homes increased, particularly the incidence of deaths caused by falls.
The implications A national policy framework is needed to reduce the number of premature deaths in nursing homes. Professionals from governments and the nursing home sector should develop strategies for preventing these deaths, and a lead authority established that is responsible for reducing harm by improving practice in nursing homes.
Improving the quality of care for nursing home residents requires a better understanding of how, why, where and when they die. The global population is ageing rapidly, and the need for aged care services is consequently increasing. However, there is a paucity of information1 about the cause and manner of premature deaths of nursing home residents (ie, sooner than necessary2). At the same time, the standard of care provided in nursing homes is under increasing scrutiny by the community and governments; whether this has altered the incidence of deaths from injuries to residents, however, is unknown.
There are two populations of nursing home residents — permanent and temporary (or respite care) residents — and injury prevention strategies should probably be different for the two. Older people move to nursing homes for various reasons, including declining health,3 limited support from caregivers, increased dependence,4 security, and changes in their financial situation.5 A progressive approach to injury prevention is therefore needed, similar to other public health responses, such as the whole organisation (workplace safety) and whole of society approaches (immunisation, road safety) of public health programs.6
Mortality data are conventionally employed as indicators of population health, to identify differences in health outcomes in defined populations, to evaluate health and aged care systems, to assist policy makers assign resources according to set priorities, and to identify modifiable factors for improving quality of life. In Australia, state legislation requires that external cause deaths (ie, deaths resulting from an injury, violence or other external event) be reported to the coroner for investigation. Together with original medical records, coronial medico-legal investigations (which include specialist forensic pathology reports and a police incident report) provide some of the most detailed information about injury-related deaths in nursing homes.
Location of death data provide information about how dying is managed and the responsibility and accountability of those who have the ability to intervene and prevent an injury event. People hope for a “good death”, preferably at home, surrounded by familiar faces.7 Whether an older person has died in a nursing home is not always clear, as vital statistics do not routinely include information about the place of death, although it is recommended as a high priority characteristic by the World Health Organization.8
The aim of our study was to provide detailed information about nursing home resident deaths on the basis of coronial data, and to undertake a descriptive epidemiological analysis of external cause deaths in Australian nursing homes. It was motivated by the fact that deaths of nursing home residents have not previously been quantified nationally.
Methods
This retrospective study analysed data for people residing in accredited nursing homes whose deaths were reported to Australian coroners between 1 July 2000 and 30 June 2013 (Box 1). The definitions applied in our study are included in the online Appendix.
All deaths directly or indirectly resulting from injury or non-natural causes must be reported to coroners. The National Coronial Information System (NCIS) is the Australian electronic data storage and retrieval system that has recorded all deaths reported to coroners in Australia since July 2000 (since 2001 for Queensland). In addition to coded data fields, the NCIS contains full text documents, including the police report on the circumstances of the death, the autopsy report, any forensic toxicology report, and the coroner’s finding.9
Deaths were identified for which the incident location was classified as “home for the elderly/retirement village”, “nursing home”, “hospice, palliative or respite care”, or “residential care facility”. A further search identified deaths of people over 40 years of age at an incident location other than those listed above. Coroners’ findings were also reviewed to identify further nursing home resident deaths.
Cases were included if the death occurred between 1 July 2000 and 30 June 2013, the coroner’s investigation was completed by 31 December 2014, and the death occurred while the deceased person resided in a nursing home accredited by the Aged Care Standards and Accreditation Agency (ACSAA) (determined by comparing the residential, incident or death addresses with a list of accredited nursing homes). Cases were excluded if there was insufficient information to identify the location of the incident leading to death, or if it could not be determined whether the person resided in a nursing home or independent living facility.
Information collected included socio-demographic characteristics; the locations (ie, in or outside the nursing home) of residence, the incident leading to death, and of the death itself; the mechanism and cause of death (including the International Classification of Diseases, tenth revision [ICD-10] causes of death coding assigned by the Australian Bureau of Statistics [ABS]); and the type of care the resident received (permanent or respite resident). The classifications of death recorded in the NCIS, the basis for the ICD-10 mortality classification assigned by the ABS,10 were used. External cause deaths were then disaggregated into subgroups based on whether the death was intentional, ABS ICD-10 cause of death coding, and mechanism of injury.
Information on the broader nursing home population was obtained from government reports.11-13 Population data for nursing home residents were obtained from the Australian Institute of Health and Welfare (AIHW) for each financial year.
Data analysis
A series of descriptive statistical analyses were conducted in SPSS Statistics 23 (IBM) of the causes of death, analysed by sex and age group, and by location of incidents leading to death and location of death; coronial inquests and recommendations; and residential status. Causes of death were grouped into three larger categories — natural cause, external cause (falls), and external cause (other) — as for some specific causes the number of deaths was small. Rates of death were estimated on the basis of ABS population and AIHW nursing home data.
Ethics approval
Ethics approval for the study was granted by the Victorian Institute of Forensic Medicine Research Advisory Committee (reference, RAC 011/13) and the Department of Justice Human Research Ethics Committee (reference, CF/13/8187).
Results
Of the 22 204 deaths of nursing home residents reported to Australian coroners during 1 July 2000 – 30 June 2013, 532 were excluded (Box 1). Of the remaining 21 672 deaths, 3289 (15.2%) had been classified as external cause deaths.
Most external cause deaths were of women (2001 cases, 60.8%), consistent with the proportion of women in nursing homes.14 The age range for residents dying of external causes was 25–106 years for women (median, 88 years; interquartile range [IQR], 84–92 years) and 39–103 years for men (median, 86 years; IQR, 80–90 years). Most external cause deaths involved residents aged 85–94 years (1742 cases, 53.0%). The age distribution of nursing home residents in our study was similar to the age distribution of nursing home residents recorded by the AIHW; differences between proportions for specific age brackets ranged from 0.2% (for those under 65) to 4.7% (90–94 years of age).14
Of the 21 672 deaths of nursing home residents reported to coroners, 11 766 (54.3%) resulted in a full internal autopsy, while 8739 (40.3%) were followed only by an external examination; for 1167 cases (5.4%) there was no information on whether an autopsy had been performed.
Cause and manner of death
The majority of deaths from external causes were unintentional (3067 cases, 93.3%), most related to falls (2679 cases, 87.3% of unintentional cases, 81.5% of all cases). Intentional injuries were involved in 183 external cause deaths (5.6% of all cases), most through suicide (146 cases, 4.4%). Thirty-nine deaths (1.2% of all cases) resulted from complications of clinical care (Box 2).
Using ABS and AIHW data, the rates of death per 100 000 persons aged 65 years or more, per 1000 residential aged care services admissions, and per 100 000 nursing home bed-days were calculated for each financial year (Box 3). The incidence of natural cause deaths of nursing home residents declined during the study period (from 36.2 per 1000 admissions in 2001–02 to 10.7 per 1000 admissions in 2011–12). The rate of external cause deaths increased, particularly those caused by unintentional falls (from 1.2 per 1000 admissions in 2001–02 to 5.3 per 1000 admissions in 2011–12; Box 3).
Unintentional deaths
Almost 60% of fall-related deaths (1533 cases) were of residents aged 85–94 years; the proportion was similar to those for choking, transport, asphyxia and other incident types (data not shown). Most deaths related to thermal injuries, drowning or poisoning were of people aged 75–84 years. Most deaths related to falls, thermal injuries, asphyxia and aspiration or poisoning were of women; deaths related to drowning were more common for men, while equal proportions of deaths caused by choking and transport crashes involved men and women (Box 2).
The largest proportions of deaths attributed to complications of clinical care were of residents aged 85–94 years (17 cases, 44%; data not shown) and of women (25 cases, 64%; Box 2).
Intentional deaths
The largest proportions of deaths by suicide (55 cases, 38%) or consequences of resident-to-resident assault (14 cases, 41%) were for people aged 85–94 years (data not shown); about 70% of suicide deaths were by men (103 cases). There were three homicide deaths of residents aged 75–84 years, two of them men, but more women than men died as the result of resident-to-resident assault (22 cases, 65% of cases; Box 2).
Location of incident leading to death
Most incidents resulting in deaths of nursing home residents occurred in the nursing home (3152 cases, 95.8%; Box 4). Unsurprisingly, the incident occurred in the nursing home for most deaths resulting from choking (249 cases, 95%), suicide (116, 80%), and resident-to-resident assault (34 cases, 100%).
Location of death
Most deaths of nursing home residents resulting from external causes occurred outside the nursing home (2207 cases, 67.1%), usually in a hospital. The proportions were particularly high for deaths resulting from transport crashes (36 cases, 95%), drowning (13 cases, 87%), thermal injuries (19 cases, 83%) or falls (1939 cases, 72%; Box 4). While all resident-to-resident assaults occurred in the nursing home, most resulting deaths were outside the nursing home (22 cases, 65%). Deaths from asphyxia and aspiration (21 cases, 91%), poisoning (14 cases, 78%), choking (176 cases, 67%), homicide (2 cases, 67%) and suicide (89 cases, 61%) usually occurred in the nursing home.
Residential status
More than 98% of external cause deaths of nursing home residents were of permanent home residents (3230 cases, 98.2%). Most deaths of respite residents resulted from falls (44 of 59 respite resident deaths, 75%), suicide (6 cases, 10%) or choking (4 cases, 7%).
Inquests and coroners’ recommendations
There were 95 coroners’ inquests (open court hearings; 2.9% of external cause deaths) and coroners’ recommendations about injury prevention were made for 53 cases (1.6%). The rate of inquests in individual states and territories ranged between 0 and 8%, and that of coroners’ recommendations between 0 and 21%.
Discussion
This study was the most comprehensive descriptive epidemiologic analysis of external cause deaths in accredited nursing homes reported to Australian coroners. We found that premature and preventable deaths occur in nursing homes, and it follows that coroners have an important role in identifying factors that may prevent death and injury. However, formal coroners’ inquests examined fewer than 3% of the external cause deaths, and in 98.4% of all cases coroners made no recommendations about injury prevention. There were substantial variations between jurisdictions in the number of cases for which recommendations were delivered (0–21%).
From an injury prevention viewpoint, it is notable that most non-natural causes of deaths of nursing home residents were related to falls (81.5%); choking (7.9%) and suicide (4.4%) were the other two major causes. In contrast, the number of deaths attributed to complications of clinical care was small (1.2%).
Despite the public policy emphasis on and social expectations about dying well at home,7,15 we found that 95% of fatal incidents occurred in the nursing home, but more than two-thirds of external cause deaths were outside the facility. This reflects the large number of deaths in hospital, usually from the complications of falls.
The increase in the incidence of external cause deaths during the study period was prominent. This is partly attributable to improved coronial advisory systems and better understanding of what constitutes a reportable death, as well as removal of the requirement in some jurisdictions to report all natural cause nursing home deaths.
It is possible that we have under-reported the burden of external cause deaths in this population, as some deaths may have been misclassified as natural cause deaths because of diagnostic minimisation (downplaying the significance of illnesses or contributing injury-related factors) of the background trauma.2 Overcoming this problem would require in depth case analysis by a medico-legal clinical team, beyond the scope of our study. Researchers evaluating quality of care have reported that undertreatment and errors of omission are not easily recognised.16 The multiple comorbidities and frailty of nursing home residents make it difficult to demarcate disease progression from other causes of death, including complications of care and non-recent trauma.
In contrast, direct external cause deaths (deaths resulting directly from environmental events or circumstances)17 are by definition preventable.18 Our findings are similar to those from other developed countries.1,19,20 Disturbingly, there has been no reduction in the prevalence of these types of external cause deaths over the past 12 years. This raises an important question about governance structures for the care and safety of nursing home residents. As most incidents contributing to these deaths occurred in the nursing homes, their operators are regarded as being responsible for improving the residents’ care.
Whether operators are also responsible for deaths of residents outside the nursing home is also worth discussing. A comprehensive public health approach to injury prevention would certainly involve nursing home staff and owners. This conceptual shift provides a unique opportunity for influencing broader societal questions, such as promoting road safety.
Implications
Our study should prompt action in policy, practice and research. National policy must act upon the evidence that premature deaths occur in nursing homes. Our data challenge the misperception that all deaths of frail, older persons with multiple comorbidities living in residential care are natural. Effective planning for high quality aged care requires accurate data about preventable harm, as well as acknowledging that negatively value-laden judgements about the worth of an older person’s life do not justify inaction.
It is estimated that by the mid-2050s Australia’s population will be 31–43 million, 25% of whom will be aged 65 years or more.21 Rapid ageing of populations is apparent worldwide and will contribute to increasing numbers of nursing home residents. Better management of risks contributing to external cause deaths in nursing homes could save some of the financial costs of providing aged care. Responsibility for better management is multilayered, requiring action at the regulatory, organisational, and health and aged care professional levels. This approach is reflected in efforts to reduce the rate of preventable health care-related deaths, and should also be adopted for improving nursing home care.
As compelling as the economic argument is, more persuasive is the principle that a person’s life should not be prematurely shortened. The concept of dying well encompasses a death free of avoidable suffering. Coroners’ investigations provide greater depth to our understanding of premature deaths in aged care and, if accompanied by specific recommendations, can identify opportunities for preventing death and injury.
Although aged care in Australia is actively monitored by a range of mechanisms,22 no one entity is responsible for reducing harm by improving practice. Interventions for preventing some of these premature deaths are contentious, and there has been little empirical investigation of their effectiveness.6 For general health care, in contrast, there is a leading national agency, the Australian Commission on Safety and Quality in Health Care (https://www.safetyandquality.gov.au/), and preventable harm is monitored, investigated and acted upon by providing resources, training, education and research to rectify problems and improve care.
The major strength of our national, population-based, 13-year longitudinal study was that we analysed detailed mortality data to identify the types of deaths occurring in nursing homes. Our findings are likely to be generalisable to other jurisdictions in developed countries with similar population demographics and health and aged care systems. Limitations include the retrospective evaluation of prospectively collected data potentially causing bias, as causes of death may be incompletely recorded, missing, or misclassified.23
Conclusion
The incidence of premature and potentially preventable deaths of nursing home residents has increased over the past decade. A national policy framework and implementation plan for reducing harm in nursing homes is needed. Primary prevention should be a top priority, and professionals from governments and the nursing home sector should be involved in developing evidence-based strategies in consultation with residents and their families.
Box 1 – Selection of nursing home deaths included in our analysis*
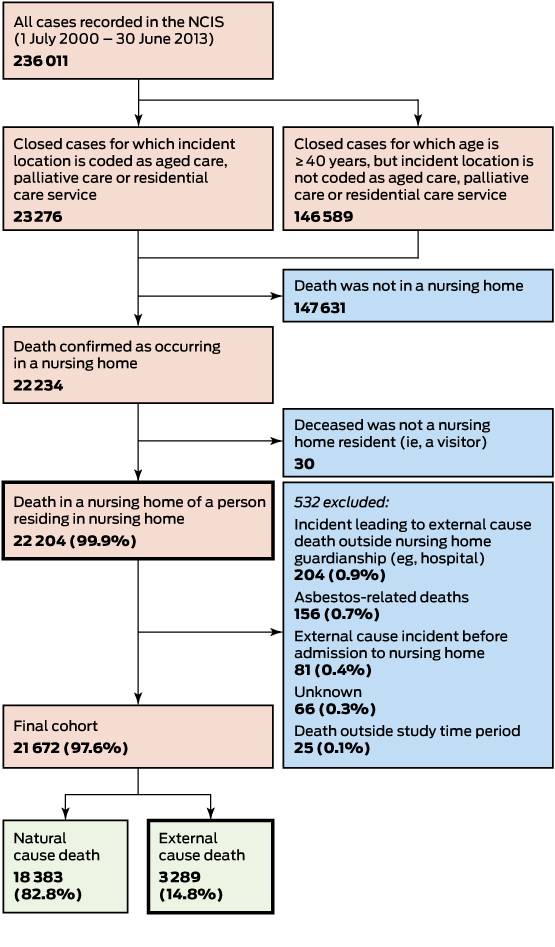
NCIS=National Coronial Information System. *The 21672 nursing home deaths reported to coroners during 1 July 2000 – 30 June 2013 comprised 3.5% of all nursing home deaths (612115) and 8.8% of all deaths reported to coroners (245437).
Box 2 – External cause deaths of nursing home residents as determined by coroner, Australia, 1 July 2000 – 30 June 2013, by sex
|
|
Women |
Men |
All residents |
||||||||||||
|
|
|||||||||||||||
|
Total number of deaths |
2001 (60.8%) |
1288 (39.2%) |
3289 |
||||||||||||
|
Cause and manner of death |
|
|
|
||||||||||||
|
Falls |
1710 (63.8%) |
969 (36.2%) |
2679 (81.5%) |
||||||||||||
|
Other unintentional |
|
|
|
||||||||||||
|
Choking |
128 (49%) |
133 (51%) |
261 (7.9%) |
||||||||||||
|
Transport crashes |
19 (50%) |
19 (50%) |
38 (1.2%) |
||||||||||||
|
Asphyxia and aspiration |
14 (61%) |
9 (39%) |
23 (0.7%) |
||||||||||||
|
Thermal |
16 (70%) |
7 (30%) |
23 (0.7%) |
||||||||||||
|
Poisoning |
11 (61%) |
7 (39%) |
18 (0.5%) |
||||||||||||
|
Drowning |
3 (20%) |
12 (80%) |
15 (0.5%) |
||||||||||||
|
Other |
9 (90%) |
1 (10%) |
10 (0.3%) |
||||||||||||
|
Complications of clinical care |
25 (64%) |
14 (36%) |
39 (1.2%) |
||||||||||||
|
Intentional |
|
|
|
||||||||||||
|
Suicide |
43 (30%) |
103 (70%) |
146 (4.4%) |
||||||||||||
|
Resident-to-resident assault |
22 (65%) |
12 (35%) |
34 (1.0%) |
||||||||||||
|
Homicide |
1 (30%) |
2 (70%) |
3 (0.1%) |
||||||||||||
|
Age group (years) |
|
|
|
||||||||||||
|
<65 |
49 (46%) |
57 (54%) |
106 (3.2%) |
||||||||||||
|
65–74 |
70 (35%) |
132 (65%) |
202 (6.1%) |
||||||||||||
|
75–84 |
452 (54.6%) |
376 (45.4%) |
828 (25.2%) |
||||||||||||
|
85–94 |
1117 (64.1%) |
625 (35.9%) |
1742 (53.0%) |
||||||||||||
|
≥95 |
312 (76%) |
98 (24%) |
410 (12.5%) |
||||||||||||
|
Unknown |
1 (<1%) |
0 |
1 (<1%) |
||||||||||||
|
|
|||||||||||||||
|
Percentages for men and women are row percentages; percentages for all residents are percentages of all external cause deaths. |
|||||||||||||||
Box 3 – Rates of death of nursing home residents, Australia, 1 July 2000 – 30 June 2013, by cause of death and financial year
|
Financial year* |
Natural cause |
External cause (falls) |
External cause (other) |
||||||||||||
|
Number |
Per 100 000 ≥65 years† |
Per 1 000 RACS admissions |
Per 10 0000 bed-days |
Number |
Per 100 000 ≥65 years† |
Per 1 000 RACS admissions |
Per 100 000 bed-days |
Number |
Per 100 000 ≥65 years† |
Per 1 000 RACS admissions |
Per 100 000 bed-days |
||||
|
|
|||||||||||||||
|
2001–02 |
2176 |
85.5 |
36.2 |
4.2 |
72 |
2.9 |
1.2 |
0.1 |
29 |
0.9 |
0.5 |
— |
|||
|
2002–03 |
2 194 |
85.4 |
33.9 |
4.2 |
71 |
2.8 |
1.1 |
0.1 |
36 |
1.3 |
0.6 |
0.1 |
|||
|
2003–04 |
2 480 |
94.6 |
37.3 |
4.5 |
119 |
4.5 |
1.8 |
0.2 |
51 |
1.8 |
0.8 |
0.1 |
|||
|
2004–05 |
2 589 |
96.4 |
39.5 |
4.6 |
118 |
4.5 |
1.8 |
0.2 |
45 |
1.6 |
0.7 |
0.1 |
|||
|
2005–06 |
1 017 |
36.3 |
15.3 |
1.7 |
140 |
5.2 |
2.1 |
0.2 |
51 |
1.7 |
0.8 |
0.1 |
|||
|
2006–07 |
976 |
34.1 |
14.6 |
1.6 |
151 |
5.5 |
2.3 |
0.3 |
30 |
0.9 |
0.4 |
— |
|||
|
2007–08 |
1 016 |
34.8 |
14.8 |
1.7 |
218 |
7.6 |
3.2 |
0.4 |
53 |
1.7 |
0.8 |
0.1 |
|||
|
2008–09 |
981 |
31.8 |
14.2 |
1.6 |
315 |
10.9 |
4.6 |
0.5 |
59 |
1.8 |
0.9 |
0.1 |
|||
|
2009–10 |
808 |
25.6 |
11.6 |
1.3 |
365 |
12.1 |
5.3 |
0.6 |
65 |
1.8 |
0.9 |
0.1 |
|||
|
2010–11 |
744 |
22.2 |
10.7 |
1.1 |
409 |
13.1 |
5.9 |
0.7 |
77 |
2.2 |
1.1 |
0.1 |
|||
|
2011–12 |
742 |
21.8 |
10.7 |
1.1 |
368 |
11.4 |
5.3 |
0.6 |
49 |
1.3 |
0.7 |
0.1 |
|||
|
|
|||||||||||||||
|
RACS=residential aged care service (the term used by the Australian Institute of Health and Welfare for nursing homes).*Financial year 2000–01 is excluded because Queensland did not contribute data to the National Coronial Information System until January 2001; financial year 2012-13 was excluded because of the requirement to exclude active coronial investigations.†Residents under 65 years of age were excluded from all analysis for this table. |
|||||||||||||||
Box 4 – Locations of incident and death for external cause deaths of nursing home residents, Australia, 1 July 2000 – 30 June 2013, by cause and manner of death
|
|
Location of incident |
Location of death |
|||||||||||||
|
Outside nursing home |
In nursing home |
Total |
Outside nursing home |
In nursing home |
Total |
||||||||||
|
|
|||||||||||||||
|
All external cause deaths |
137 (4.2%) |
3152 (95.8%) |
3289 |
2207 (67.1%) |
1082 (32.9%) |
3289 |
|||||||||
|
Falls |
42 (2%) |
2637 (98%) |
2679 |
1939 (72%) |
740 (28%) |
2679 |
|||||||||
|
Other unintentional |
|
|
|
|
|
|
|||||||||
|
Choking |
12 (5%) |
249 (95%) |
261 |
85 (33%) |
176 (67%) |
261 |
|||||||||
|
Transport crashes |
33 (87%) |
5 (13%) |
38 |
36 (95%) |
2 (5%) |
38 |
|||||||||
|
Asphyxia and aspiration |
0 |
23 (100%) |
23 |
2 (9%) |
21 (91%) |
23 |
|||||||||
|
Thermal |
2 (9%) |
21 (91%) |
23 |
19 (83%) |
4 (17%) |
23 |
|||||||||
|
Poisoning |
2 (11%) |
16 (89%) |
18 |
4 (22%) |
14 (78%) |
18 |
|||||||||
|
Drowning |
12 (80%) |
3 (20%) |
15 |
13 (87%) |
2 (13%) |
15 |
|||||||||
|
Other |
0 |
10 (100%) |
10 |
6 (60%) |
4 (40%) |
10 |
|||||||||
|
Complications of clinical care |
3 (8%) |
36 (92%) |
39 |
23 (59%) |
16 (41%) |
39 |
|||||||||
|
Intentional |
|
|
|
|
|
|
|||||||||
|
Suicide |
30 (20%) |
116 (80%) |
146 |
57 (39%) |
89 (61%) |
146 |
|||||||||
|
Resident-to-resident assault |
0 |
34 (100%) |
34 |
22 (65%) |
12 (35%) |
34 |
|||||||||
|
Homicide |
1 (33%) |
2 (67%) |
3 |
1 (33%) |
2 (67%) |
3 |
|||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Received 21 July 2016, accepted 27 January 2017
- Joseph E Ibrahim1
- Lyndal Bugeja1
- Melissa Willoughby1
- Marde Bevan1
- Chebiwot Kipsaina1
- Carmel Young1
- Tony Pham1
- David L Ranson2
- 1 Monash University, Melbourne, VIC
- 2 Victorian Institute of Forensic Medicine, Melbourne, VIC
This work was supported by the federal Department of Social Services, the Victorian Department of Health and Human Services (Ageing and Aged Care Branch), and the Department of Forensic Medicine, Monash University. None of the funders influenced the design, methods, subject recruitment, data collection, analysis or preparation of the paper.
We are affiliated with or employed by the Department of Forensic Medicine, Monash University, which was also a funding source.
- 1. Ibrahim J, Murphy B, Bugeja L, Ranson D. Nature and extent of external-cause deaths of nursing home residents in Victoria, Australia. J Am Geriatr Soc 2015; 63: 954-962.
- 2. Hitchen T, Ibrahim J, Woolford M, Bugeja L. Premature and preventable deaths in frail, older people: a new perspective. Ageing Soc 2016; doi:10.1017/S0144686X16000428.
- 3. Stoeckel KJ, Porell FW. Do older adults anticipate relocating? The relationship between housing relocation expectations and falls. J Appl Gerontol 2010; 29: 231-250.
- 4. Hallberg D, Lagergren M. Moving in and out of public old age care among the very old in Sweden. Eur J Ageing 2009; 6: 137-145.
- 5. Saito T, Lee H, Kai I. Health and motivation of elderly relocating to a suburban area in Japan. Arch Gerontol Geriatr 2007; 45: 217-232.
- 6. McClure RJ, Davis E, Yorkston E, et al. Special issues in injury prevention research: developing the science of program implementation. Injury 2010; 41: S16-S19.
- 7. Swerissen H, Duckett S. Dying well (Grattan Institute Report No. 2014-10). Melbourne: The Grattan Institute, 2014. https://grattan.edu.au/wp-content/uploads/2014/09/815-dying-well.pdf (accessed Mar 2017).
- 8. World Health Organization. Improving the quality and use of birth, death and cause-of-death information: guidance for a standards-based review of country practices. Geneva: WHO, 2010. http://www.who.int/healthinfo/tool_cod_2010.pdf (accessed Mar 2017).
- 9. National Coroners Information System. About NCIS [website]. www.ncis.org.au/data-collection/ (accessed Mar 2017).
- 10. National Coroners Information System. Data dictionary for the National Coronial Information System. Version 3b. Melbourne: NCIS, 2014. http://www.ncis.org.au/wp-content/uploads/2014/06/DataDictionary-Version3b-revised.pdf (accessed Mar 2017).
- 11. Australian Bureau of Statistics. 3101.0. Australian demographic statistics, Jun 2016. Population by age and sex, Australia, states and territories. Dec 2016. http://www.abs.gov.au/ausstats/abs@.nsf/0/1CD2B1952AFC5E7ACA257298000F2E76?OpenDocument (accessed Mar 2017).
- 12. Australian Government, Productivity Commission. Report on government services 2015. 13. Aged care services. http://www.pc.gov.au/research/ongoing/report-on-government-services/2015/community-services/aged-care-services (accessed Mar 2017).
- 13. Australian Government, Department of Health. Aged Care Service List — 30 June 2014 — Australia. https://agedcare.health.gov.au/ageing-and-aged-care-overview/about-aged-care/aged-care-service-list-30-june-2014-australia (accessed Mar 2017).
- 14. Australian Institute of Health and Welfare. Residential aged care in Australia 2010–11: a statistical overview. Canberra: AIHW, 2012.
- 15. Broad JB, Gott M, Kim H, et al. Where do people die? An international comparison of the percentage of deaths occurring in hospital and residential aged care settings in 45 populations, using published and available statistics. Int J Public Health 2013; 58: 257-267.
- 16. Kalisch B, Landstrom G, Williams R. Missed nursing care: errors of omission. Nurs Outlook 2009; 57: 3-9.
- 17. World Health Organization. International statistical classification of diseases and related health problems. Geneva: WHO, 2006.
- 18. World Health Organization. More than words: conceptual framework for the international classification for patient safety. Version 1.1. Geneva: WHO, 2009. www.who.int/patientsafety/taxonomy/icps_full_report.pdf (accessed Mar 2017).
- 19. Berry C, Heaton-Armstrong A. A review of the coroner system in England and Wales: a commentary. Clin Med 2005; 5: 455-459.
- 20. Gjertsen F, Johansson LA. Changes in statistical methods affected the validity of official suicide rates. J Clin Epidemiol 2011; 64: 1102-1108.
- 21. Australian Bureau of Statistics. One in four Australians aged 65 years and over by 2056: ABS [media release]. 4 Sept 2008. http://www.abs.gov.au/ausstats/abs@.nsf/mediareleasesbyTopic/2CA2134677EF9D03CA257C2E0017283B?OpenDocument (accessed Mar 2016).
- 22. Australian Government, Productivity Commission. Caring for older Australians. Inquiry report. Canberra: PC, 2011. http://www.pc.gov.au/inquiries/completed/aged-care/report#contents (accessed Mar 2017).
- 23. Bugeja L, Ibrahim J, Ferrah N, et al. The utility of medico-legal databases for public health research: a systematic review of peer-reviewed publications using the National Coronial Information System. Health Res Policy Syst 2016; 14: 28.





Abstract
Objectives: To conduct a descriptive epidemiological analysis of external cause deaths (premature, usually injury-related, and potentially preventable) of nursing home residents in Australia.
Design: Retrospective study of a cohort of nursing home residents, using coronial data routinely recorded by the National Coronial Information System.
Setting and participants: Residents of accredited Australian nursing homes, whose deaths were reported to coroners between 1 July 2000 and 30 June 2013, and determined to have resulted from external causes.
Main outcome measures: Causes of death, analysed by sex and age group, and by location of incidents leading to death and location of death. Rates of death were estimated on the basis of Australian Bureau of Statistics population and Australian Institute of Health and Welfare nursing home data.
Results: Of 21 672 deaths of nursing home residents, 3 289 (15.2%) resulted from external causes. The most frequent mechanisms of death were falls (2 679 cases, 81.5%), choking (261 cases, 7.9%) and suicide (146 cases, 4.4%). The incidents leading to death usually occurred in the nursing home (95.8%), but the deaths more frequently occurred outside the nursing home (67.1%). The annual number of external cause deaths in nursing homes increased during the study period (from 1.2 per 1000 admissions in 2001–02 to 5.3 per 1000 admissions in 2011–12).
Conclusion: The incidence of premature and potentially preventable deaths of nursing home residents has increased over the past decade. A national policy framework is needed to reduce the incidence of premature deaths among Australians living in nursing homes.