Clinical record
A 52-year-old man was referred for laser therapy of facial papules for cosmetic reasons. The patient presented with a history of multiple asymptomatic facial lesions that had slowly erupted over a 10-year period. Before this consultation, the patient had been referred to a dermatologist to exclude skin cancer and biopsy of a lesion showed an angiofibroma and no evidence of malignancy. Personal history was remarkable for recurrent bilateral spontaneous pneumothoraces requiring pleurodesis. His family history was positive for recurrent pneumothorax in an adult son and recent onset of similar facial lesions in another son. There was no personal or family history of renal carcinoma.
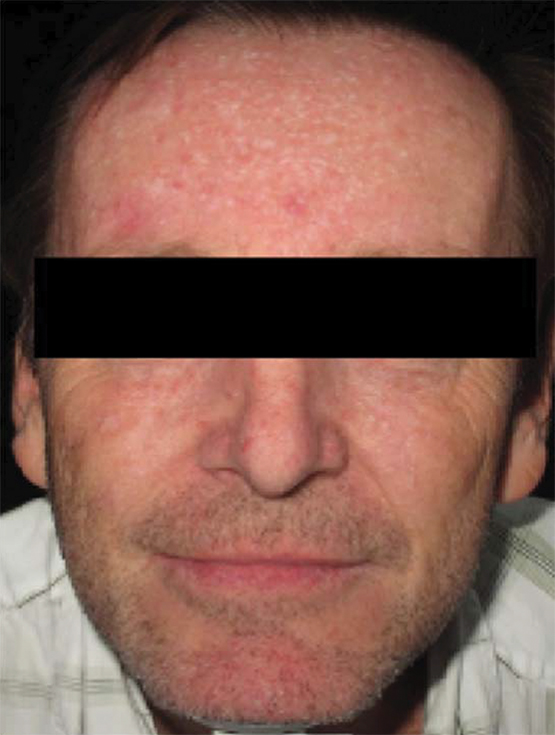
Physical examination revealed multiple dome-shaped firm whitish papules over the forehead and cheeks (Figure 1 and Figure 2). The clinical presentation of multiple facial fibrous papules occurring on a background of unexplained pneumothoraces was suggestive of the genetic condition, Birt-Hogg-Dubé syndrome (BHD). Repeat punch biopsy of a lesion revealed an infundibulum with perifollicular fibrosis suggestive of a trichodiscoma, supportive of BHD.
The patient was referred to a cancer genetic clinic for counselling, genetic testing and screening. Renal ultrasound revealed a left renal hypoechoic lesion measuring 2.5 × 2.1 × 2.4 cm. The patient underwent robotic left partial nephrectomy, and pathology revealed a hybrid oncocytic/chromophobe tumour. Although this tumour was growing in a benign manner, it displayed low-grade renal cell carcinoma features. However, as the tumour was completely excised, no further treatment was required.
Genetic testing of blood revealed a heterozygous FLCN c.853C>T mutation on chromosome 17. Genetic counselling and radiographic renal screening of family members is planned. As per suggested guidelines, our patient will undergo lifelong medical surveillance by periodic renal ultrasound and/or magnetic resonance imaging.1
BHD is a rare, autosomal dominant, hereditary cancer syndrome due to germline mutations in the folliculin gene (FLCN). The incidence of BHD is about one in 200 000 of the population; however, it is likely underdiagnosed because of low clinical awareness.1,2 Folliculin is a protein expressed on keratinocytes in the basal and spinous layer of the epidermis, dermal fibroblasts, nerve cells, lymphocytes, macrophages and mast cells. Extracutaneously, folliculin is expressed on pulmonary type-1 alveolar epithelial cells and distal nephrons.3 Folliculin is a tumour suppressor protein, important in cell signalling pathways that regulate cell growth. It is proposed that genetic mutation results in loss of a functional protein in cells, resulting in unchecked tumour growth.4 The pattern of folliculin expression correlates with the clinical features of BHD, including skin papules of varying pathologies, basal lung cysts, spontaneous pneumothorax and renal cell carcinomas.
Proposed diagnostic criteria for BHD include the presence of one major or two minor features.2 Major features are at least five adult onset fibrofollliculomas or trichodiscomas, with histological confirmation, or a pathogenic FLCN mutation. Fibrofolliculomas and trichodiscomas present as multiple small flesh-coloured or white dome-shaped papules on the face, neck and upper trunk. Angiofibromas have also been associated with BHD; however, the presence of multiple angiofibromas is more suggestive of tuberous sclerosis.5 Minor features include a history of bilateral basal lung cysts, with or without spontaneous pneumothorax, early onset (age < 50 years) renal carcinoma with multifocal or bilateral carcinomas or a mixed chromophobe/oncocytic histology, and a first-degree relative with BHD.6
Patients with BHD have a 50-fold increased risk of primary spontaneous pneumothorax development and more than 80% of affected individuals have multiple pulmonary cysts visible on a computed tomography scan, with the less common basal rather than apical predilection.6,7 Renal cell carcinomas occur in 27% of affected individuals. A wide range of renal carcinomas have been reported, with the most common pathology being the unusual mixed oncocytic/chromophobe tumour. More than 65% of patients with BHD and renal carcinoma present with multifocal, bilateral or recurrent tumours.
Early recognition of BHD is crucial, given the high risk of renal neoplasm development which, if detected early, is curable. Thus the general practitioner and dermatologist are uniquely placed to consider the diagnosis of BHD when consulted by a patient requesting removal of multiple facial papules. Unexplained spontaneous pneumothorax and basal lung cysts should also raise suspicion of BHD. Referral for genetic testing and multidisciplinary care is essential. Routine renal radiographic screening is recommended for affected individuals > 40 years and, given the likelihood of multiple tumours, nephron-sparing surgery is preferred.8
Treatment of skin lesions associated with BHD is elective. In particular, laser ablation of individual lesions may improve the appearance for cosmetic reasons.Lessons from practice
Birt-Hogg-Dubé syndrome (BHD) is an autosomal dominant condition caused by germline mutations in the folliculin gene.
Phenotypical features of this rare syndrome include multiple white dome-shaped facial papules and bilateral basal lung cysts, predisposing to spontaneous pneumothorax.
Diagnosing BHD early is important, as the genetic defect is also associated with early onset renal cell carcinomas, of varying pathology.
As there are variations in presentation, a combination of multiple facial papules, spontaneous pneumothorax and a personal or family history of renal cell carcinoma should trigger consideration of BHD.
- Ludi Ge
- Patricia Lowe
- Royal Prince Alfred Hospital, Sydney, NSW
No relevant disclosures.
- 1. Haas NB. Nathanson KL. Hereditary kidney cancer syndromes. Adv Chronic Kidney Dis 2014; 21: 81-90.
- 2. Menko FH, van Steensel MA, Giraud S, et al. Birt-Hogg-Dubé syndrome: diagnosis and management. Lancet Oncol 2009; 10: 1199-1206.
- 3. Warren MB, Torres-Cabala CA, Turner ML, et al. Expression of Birt-Hogg-Dube gene mRNA in normal and neoplastic human tissues. Mod Pathol 2004; 17: 998-1011.
- 4. Possik E, Jalali Z, Nouet Y, et al. Folliculin regulates AMPK-dependent autophagy and metabolic stress survival. PLOS Genet 2014; 10: e1004273.
- 5. Schaffer JV, Gohara MA, McNiff JM, et al. Multiple facial angiofibromas: a cutaneous manifestation of Birt-Hogg-Dube syndrome. J Am Acad Dermatol 2005; 53: 108-111.
- 6. Houweling AC, Gijezen LM, Jonker MA, et al. Renal cancer and pneumothorax risk in Birt-Hogg-Dubé syndrome; an analysis of 115 FLCN mutation carriers from 35 BHD families. Br J Cancer 2011; 105: 1912-1919.
- 7. Toro JR, Wei MH, Glenn GM, et al. BHD mutations, clinical and molecular genetic investigations of Birt-Hogg-Dubé syndrome: a new series of 50 families and a review of published reports. J Med Genet 2008; 45: 321-331.
- 8. Pavlovich CP, Grubb RL, Hurley K, et al. Evaluation and management of renal tumors in the Birt-Hogg-Dubé syndrome. J Urol 2005; 173: 1482-1486.






Deborah HelwenYates
Deborah H Yates
Director, Multiple Cystic Lung/LAM Clinic, St Vincent's Hospital, Sydney 2010.
References:
1. Gupta N1, Seyama K, McCormack FX. Pulmonary manifestations of Birt-Hogg-Dubé syndrome. Fam Cancer. 2013 Sep;12(3):387-96.
2. Menko FH, van Steensel MA, Giraud S, et al. Birt-Hogg-Dubé syndrome: diagnosis and management. Lancet Oncol. 2009;10(12):1199-206.
3. Schmidt LS, Linehan WM. Clinical features, genetics and potential therapeutic approaches for Birt-Hogg-Dube´syndrome. Expert Opin Orphan Drugs. 2015; 3(1):15-29.
Competing Interests: No relevant disclosures
Assoc Prof Deborah HelwenYates
St Vincent's Hospital, Sydney
Ludi Ge
As noted, our patient had a history of recurrent pneumothoraces requiring pleurodesis. Birt-Hogg-Dubé syndrome was not identified at the time of respiratory presentation. We reiterate the importance of considering Birt-Hogg-Dubé syndrome when a patient presents with either pneumothoraces with multiple pulmonary cysts or in later years, multiple facial papules.
Competing Interests: No relevant disclosures
Dr Ludi Ge
Dermatology Department Royal Prince Alfred Hospital