Understanding the factors that contribute to hospital readmission for patients who have had acute stroke could improve outcomes for these people. Estimates of the frequency of readmission to hospital within the first year of onset vary widely from 13% to 62%, in part depending on whether readmission is for any cause or for a stroke-specific diagnosis.1,2 Hospital readmission is also frequent (36%–48%) after transient ischaemic attack (TIA).3,4 Predictors of hospital readmission after a stroke include older age, multiple comorbidities, diabetes mellitus, longer length of stay, physician specialty for the index admission, and size and type of hospital.5 To our knowledge, no study has specifically examined predictors of hospital readmission after TIA.
The Australian Stroke Clinical Registry (AuSCR) was established in 2009 to collect prospective, continuous, patient-level data on the quality of acute stroke care and patient outcomes (http://www.auscr.com.au).6 Linkage of AuSCR data to routinely collected hospital data can provide a powerful quality improvement tool, giving the ability to understand variations in care and predictors of important outcomes. These data can then be used to design interventions to reduce variations in care delivery and improve recovery after stroke.
We aimed to assess the feasibility of linking data from AuSCR to routine hospital datasets in Victoria, and to determine the frequency of and factors associated with hospital readmission during the year after acute stroke or TIA.
Methods
Datasets
Data from one Victorian hospital using AuSCR were linked to the Victorian Admitted Episodes Dataset (VAED) and Victorian Emergency Minimum Dataset (VEMD). AuSCR includes information on all admitted patients with stroke or TIA at participating hospitals, based on a minimum dataset of personal information (eg, name, address, age, sex, type of stroke), quality of care indicators (eg, treated in a stroke unit) and outcomes between 90 and 180 days after a stroke (eg, quality of life).6 The VAED contains morbidity data on all admitted patients in Victorian public and private acute hospitals and includes a wide range of demographic, administrative and some clinical variables (eg, International Classification of Diseases, 10th revision, Australian modification [ICD-10-AM] diagnosis codes). The VEMD includes similar details for people who are treated at any 24-hour emergency department (ED) of a public hospital in Victoria.
Ethics approval for this project was obtained from the ethics committee at the participating hospital and the data custodians (AuSCR and the Victorian Department of Health).
Data linkage
Data from AuSCR were linked with the VAED and VEMD for the period from 15 June 2009 to 31 December 2010. Follow-up of patients in AuSCR continued to 30 June 2011.
Data were linked using a two-stage separation principle, whereby identifying AuSCR variables for patients at the participating hospital were submitted to the Victorian Department of Health. These variables included last name and first three letters of the first name, date of birth, sex, postcode, partial Medicare number, and hospital admission unit record number (as Victorian hospitals have separate patient identification numbering systems, individuals can have multiple hospital unit record numbers). The Victorian Data Linkages unit performed stepwise deterministic linkage of the AuSCR data to the VEMD and VAED, with a 3-year look-back period. The de-identified, linked Department of Health data were then returned to the hospital principal investigator (H D), and one of us (M K) merged the content data from AuSCR with the de-identified dataset using a unique project identifier for each patient.
Outcomes
The primary outcome was all-cause hospital readmission within 30 days, 6 months and 1 year from time of hospital discharge after the index admission for stroke or TIA (ie, the first registered event in AuSCR). Hospital readmission was defined as an admission to an acute care hospital in Victoria for any reason. All primary diagnoses recorded for presentation to an ED or hospital discharge were categorised using ICD-10-AM definitions.
Patient characteristics, social circumstances, health system factors, clinical processes of care and health outcomes derived from the datasets were compared by hospital readmission status, using the categories outlined elsewhere.7 Patient characteristics (eg, age, sex, place of birth), clinical processes of care (eg, admission to an acute stroke unit, use of thrombolysis) and health outcomes (eg, discharge destination) were obtained from AuSCR. Comorbidities were obtained from the VAED using ICD-10-AM codes (Appendix). The Charlson comorbidity index (CCI) score,8 which uses 19 conditions or diseases as a prognostic marker for poor outcome,9 was calculated from VAED data. Health system data were obtained from AuSCR (eg, length of stay), the VAED (eg, number of admissions before index event, prior stroke or TIA admission) and the VEMD (eg, number of ED presentations before index event, prior stroke or TIA presentation).
Statistical analysis
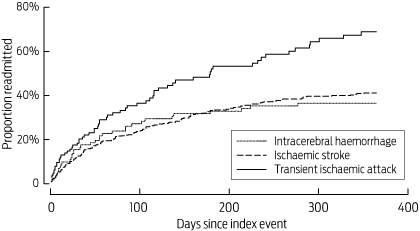
We used descriptive statistics to compare patients according to hospital readmission status, using the χ2 test for categorical variables and the Wilcoxon–Mann–Whitney rank-sum test for continuous variables. We used Nelson–Aalen cumulative hazard estimate curves to illustrate the timing of hospital readmission by stroke subtype.
Multivariable logistic regression models were used to explore factors associated with hospital readmission, which was defined as the dependent variable. The measure of stroke severity included whether a patient was able to walk on admission. Other independent variables were selected if they were statistically significant in univariable analyses, using P < 0.1 as the threshold. Assessments for collinearity were made and a condition index of 10–15 was considered acceptable.10 Multivariable results are reported as adjusted odds ratios (aORs) with 95% confidence intervals. Significance was set at P < 0.05. All analyses were undertaken with Stata (version 12.1, StataCorp).
Results
Of 788 patients registered in the AuSCR, 658 (83%) had a stroke (81% [534/658] ischaemic stroke; 18% [117/658] intracerebral haemorrhage; 1% [7/658] undetermined type) and 130 (17%) had a TIA. Their median age was 76 years (interquartile range, 66–84 years), 46% (359/781) were female, and 58% (427/738) were born in Australia. Of the AuSCR registrants, 655 (83%) were recorded as having their first-ever stroke or TIA event, while 133 (17%) had previously had a stroke or TIA.
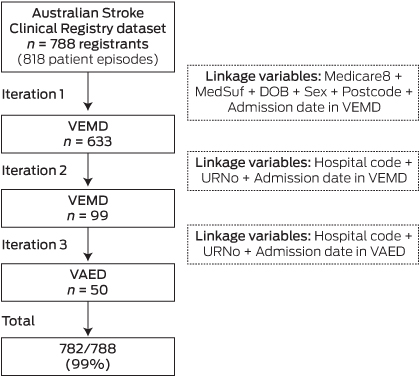
The availability of the linkage variables between datasets was excellent (Box 1). AuSCR data were linked to the VAED or VEMD over three iterations. As records were matched, they were removed from the source datasets (VAED or VEMD). The final overall matched linkage achieved was 93% of AuSCR registrants in the VAED (736/788) and the VEMD (731/788). Of the 788 AuSCR registrants, 782 (99%) were linked to at least one of the VAED and VEMD (Box 1).
Fifteen per cent of patients (108/715) had an all-cause hospital readmission within 30 days. Readmissions increased to 36% (247/694) within 6 months and 42% (291/685) within 1 year. Diseases of the circulatory system were the most common reason for hospital readmission within 1 year, occurring in 20% of patients (56/286), including stroke or TIA in 12% (35/286) (Box 2). Patients with an index TIA were more likely than patients with stroke diagnoses to be readmitted within 1 year (Box 3).
Many patient characteristics were similar for those with and without hospital readmission within 1 year (Box 4). However, readmitted patients were more likely to have stroke risk factors such as hypercholesterolaemia or diabetes mellitus and greater overall comorbidity as defined by their CCI scores.
Differences in health system, clinical care and health outcome factors between patients who were and were not readmitted within 1 year are shown in Box 5. Most patients were managed in a stroke unit for their index event, and clinical processes of care between those with and without hospital readmission were consistent. However, readmitted patients were more likely to have had more ED presentations before their index event, compared with patients who were not readmitted.
Results of multivariable analyses for each time period are shown in Box 6. The factors that remained significantly associated with hospital readmission within 1 year were ≥ 2 ED presentations before the index event, a higher CCI score, and TIA being the reason for the index hospitalisation. The same factors were associated with hospital readmission within 6 months. Higher CCI score and multiple ED presentations were associated with readmission within 30 days.
Discussion
Australian data on factors related to hospital readmission for patients with stroke or TIA are limited. We found that data linkage between the AuSCR and routine hospital datasets was feasible and can identify determinants of hospital readmission for patients who have had stroke or TIA.6,11
We found that patients with multiple ED presentations before their initial hospitalisation were more likely to be readmitted to hospital over the next year than those with fewer than two ED presentations. To our knowledge, there are no other studies with similar analyses that have explored factors associated with hospital readmission after stroke or TIA.
Our findings are consistent with data from the United States,4 where a study involving 2802 patients found that those discharged from hospital after a TIA had a greater risk of readmission within 1 year compared with patients with ischaemic stroke (hazard ratio, 1.20; 95% CI, 1.02–1.42). However, as the reason for hospital readmission was based on self-report by either patient or proxy,4 there are some concerns about the reliability of these data.12
A strength of our study is the use of ICD-10-AM coding to categorise diagnoses and outcomes, which showed that diseases of the circulatory system were the most common reason for readmission. There were no differences in the causes of readmission for patients discharged with ischaemic stroke and those with other stroke or TIA diagnoses, but the proportion of readmissions was lower than in the US study.4 Overall, we found that 42% of patients who survived an initial hospitalisation for stroke or TIA were readmitted within the first year, which falls within the range previously reported (13%–62%).1,2,13-21 However, only 12% of patients were readmitted due to another stroke or TIA. This result is similar to that from an Australian study that used data from 1075 patients in the Hunter Area Heart and Stroke Register (13%),1 but lower than in a US study of 1818 veterans with stroke, which used multiple health care plan data sources (31%).2
In our adjusted analyses, we found that increased frequency of comorbid conditions, as measured by the CCI, was independently associated with readmission within 1 year. This differs from the Hunter Area Heart and Stroke Register study, which found that people presenting with stroke had an increased number of comorbidities such as hypertension (38%), but found no association of CCI with readmission within 1 year.1 However, our results are similar to other studies which found that patients with more comorbidities (CCI score ≥ 3)13 or higher comorbidity summary scores2 were more likely to be readmitted within 1 year.
A major limitation of our study is that the data were derived from only one hospital, resulting in a small sample size (788) compared with other data linkage studies (≥ 16 000).22 This also meant that the clinical processes of care received during hospitalisation were similar for the included patients, as 98% were admitted to the same stroke unit. Frequency of readmission within 1 year and processes of care are likely to differ between health services, and our findings may not be generalisable to other health services. Further, coding quality in other hospitals was not assessed. Readmissions to hospitals outside Victoria were not captured in our study, but we believe this number would be small.
Nevertheless, we have shown that linkage of AuSCR data with routinely collected hospital data is feasible. A larger ongoing study (Stroke12311) will assess cross-jurisdictional data linkage involving over 17 000 Australian stroke patients registered in AuSCR between 2009 and 2013. These linked data will provide a richer data source across a broader range of hospitals and locations for validating our preliminary findings of the frequency and determinants of hospital readmission after stroke or TIA.
2 Primary diagnosis recorded for first readmission within 1 year,* by stroke subtype
Stroke subtype | |||||||||||||||
Cause of readmission (ICD-10-AM codes) | Total (n = 286)† | ICH (n = 37) | IS (n = 184) | TIA (n = 65) | |||||||||||
Certain infectious and parasitic diseases (A00–B99) | 7 (2.5%) | 0 | 4 (2.2%) | 3 (4.6%) | |||||||||||
Neoplasms (C00–D49) | 11 (3.9%) | 1 (2.7%) | 9 (4.9%) | 1 (1.5%) | |||||||||||
Diseases of the blood and blood-forming organs (D50–D89) | 7 (2.4%) | 0 | 7 (3.8%) | 0 | |||||||||||
Endocrine, nutritional and metabolic diseases (E00–E89) | 9 (3.2%) | 1 (2.7%) | 8 (4.3%) | 0 | |||||||||||
Mental, behavioural and neurodevelopmental (F01–F99) | 5 (1.8%) | 1 (2.7%) | 3 (1.6%) | 1 (1.5%) | |||||||||||
Diseases of the nervous system (G00–G99) | 21 (7.3%) | 2 (5.4%) | 8 (4.4%) | 11 (16.9%)‡ | |||||||||||
Diseases of the eye and adnexa (H00–H59) | 11 (3.9%) | 1 (2.7%) | 7 (3.8%) | 3 (4.6%) | |||||||||||
Diseases of the ear and mastoid process (H60–H95) | 1 (0.4%) | 0 | 1 (0.5%) | 0 | |||||||||||
Diseases of the circulatory system (I00–I99) | 56 (19.6%) | 10 (27.0%) | 30 (16.3%) | 16 (24.6%) | |||||||||||
Cerebrovascular disorders | 40 (13.9%) | 5 (13.5%) | 25 (13.6%) | 10 (15.4%) | |||||||||||
Stroke | 25 (8.7%) | 4 (10.8%) | 17 (9.2%) | 4 (6.2%) | |||||||||||
TIA | 10 (3.5%) | 0 | 5 (2.7%) | 5 (7.7%) | |||||||||||
Heart failure | 6 (2.1%) | 0 | 3 (1.6%) | 3 (4.6%) | |||||||||||
Myocardial infarction | 1 (0.4%) | 0 | 1 (0.5%) | 0 | |||||||||||
Atrial fibrillation | 5 (1.8%) | 0 | 2 (1.1%) | 3 (4.6%) | |||||||||||
Diseases of the respiratory system (J00–J99) | 10 (3.5%) | 1 (2.7%) | 9 (4.9%) | 0 | |||||||||||
Chronic pulmonary disease | 3 (1.1%) | 1 (2.7%) | 2 (1.1%) | 0 | |||||||||||
Diseases of the digestive system (K00–K95) | 21 (7.3%) | 1 (2.7%) | 14 (7.6%) | 6 (9.2%) | |||||||||||
Diseases of the skin and subcutaneous tissue (L00–L99) | 1 (0.4%) | 0 | 1 (0.4%) | 0 | |||||||||||
Diseases of the musculoskeletal system (M00–M99) | 10 (3.5%) | 1 (2.7%) | 7 (3.8%) | 2 (3.1%) | |||||||||||
Diseases of the genitourinary system (N00–N99) | 11 (3.9%) | 2 (5.4%) | 7 (3.8%) | 2 (3.1%) | |||||||||||
Congenital malformations and chromosomal (Q00–Q99) | 5 (1.8%) | 1 (2.7%) | 3 (1.6%) | 1 (1.5%) | |||||||||||
Symptoms, signs and abnormal clinical (R00–R99) | 44 (15.4%) | 8 (21.6%) | 28 (15.2%) | 8 (12.3%) | |||||||||||
Injury, poisoning and other consequences (S00–T88) | 23 (8.0%) | 0 | 17 (9.2%) | 6 (9.2%) | |||||||||||
Factors influencing health status and services (Z00–Z99) | 21 (7.3%) | 4 (10.8%) | 15 (8.2%) | 2 (3.1%) | |||||||||||
ICD-10-AM = International Classification of Diseases, 10th revision, Australian modification. ICH = intracerebral haemorrhage. IS = ischaemic stroke. TIA = transient ischaemic attack. * Patients may have had more than one readmission, but only the primary diagnosis for the first readmission is shown. † Excludes five patients with stroke of undetermined type. ‡ P < 0.05. | |||||||||||||||
4 Comparison of patient characteristics by hospital readmission within 1 year
Characteristic (data source) | Readmitted (n = 291) | Not readmitted (n = 394) | P | ||||||||||||
Patient characteristics (AuSCR) | |||||||||||||||
Median age, years (IQR) | 76 (65–83) | 75 (65–82) | 0.68 | ||||||||||||
Female | 135/288 (46.9%) | 166/390 (42.6%) | 0.26 | ||||||||||||
Born in Australia | 158/267 (59.2%) | 205/371 (55.3%) | 0.55 | ||||||||||||
Aboriginal and/or Torres Strait Islander | 3/289 (1.0%) | 3/392 (0.8%) | 0.10 | ||||||||||||
English spoken | 242/289 (83.7%) | 329/388 (84.8%) | 0.68 | ||||||||||||
Documented evidence of previous stroke | 52/291 (17.9%) | 55/394 (13.9%) | 0.37 | ||||||||||||
Pre-existing conditions (VAED)* | |||||||||||||||
Atrial fibrillation | 82/291 (28.2%) | 83/344 (24.1%) | 0.25 | ||||||||||||
Hypercholesterolaemia | 46/291 (15.8%) | 30/344 (8.7%) | 0.006 | ||||||||||||
Hypertension | 187/291 (64.3%) | 206/344 (59.9%) | 0.26 | ||||||||||||
Diabetes | 42/291 (14.4%) | 14/344 (4.1%) | < 0.001 | ||||||||||||
Angina | 20/291 (6.9%) | 13/344 (3.8%) | 0.08 | ||||||||||||
Smoking (current) | 38/291 (13.1%) | 49/344 (14.2%) | 0.67 | ||||||||||||
Obesity | 12/291 (4.1%) | 7/344 (2.0%) | 0.12 | ||||||||||||
Peripheral vascular disease | 11/291 (3.8%) | 3/344 (0.9%) | 0.01 | ||||||||||||
Congestive heart failure | 32/291 (11.0%) | 24/344 (6.9%) | 0.08 | ||||||||||||
Renal disease | 42/291 (14.4%) | 26/344 (7.6%) | 0.005 | ||||||||||||
Dementia | 18/291 (6.2%) | 24/344 (6.9%) | 0.69 | ||||||||||||
Mean Charlson comorbidity index score (SD) | 2.8 (1.9) | 2.4 (1.5) | 0.02 | ||||||||||||
Type of stroke (AuSCR) | |||||||||||||||
Intracerebral haemorrhage | 37/291 (12.7%) | 42/394 (10.6%) | 0.40 | ||||||||||||
Ischaemic stroke | 184/291 (63.2%) | 286/394 (72.6%) | 0.009 | ||||||||||||
Transient ischaemic attack | 65/291 (22.3%) | 64/394 (16.2%) | 0.04 | ||||||||||||
Undetermined | 5/291 (1.7%) | 2/394 (0.5%) | 0.12 | ||||||||||||
Stroke severity variables (AuSCR) | |||||||||||||||
Able to walk on admission | 83/236 (35.2%) | 125/358 (34.9%) | 0.95 | ||||||||||||
Cause of stroke (known) | 115/291 (39.5%) | 166/394 (42.1%) | 0.49 | ||||||||||||
Social circumstances (VAED) | |||||||||||||||
Married or with partner before admission | 186/291 (63.9%) | 226/370 (61.1%) | 0.46 | ||||||||||||
Private patient in public hospital | 92/291 (31.6%) | 109/370 (29.5%) | 0.55 | ||||||||||||
AuSCR = Australian Stroke Clinical Registry. IQR = interquartile range. VAED = Victorian Admitted Episodes Dataset. VEMD = Victorian Emergency Minimum Dataset. * According to International Classification of Diseases, 10th revision, Australian modification codes, before and at index event. | |||||||||||||||
5 Comparison of health system, clinical care and health outcome factors by hospital readmission within 1 year
Factor (data source) | Readmitted (n = 291) | Not readmitted (n = 394) | P | ||||||||||||
Health system (AuSCR) | |||||||||||||||
Median length of hospital admission, days (IQR) | 5 (2–10) | 5 (3–10) | 0.55 | ||||||||||||
Transfer from another hospital | 20/291 (6.9%) | 14/394 (3.6%) | 0.11 | ||||||||||||
Stroke occurred while in hospital for another condition | 6/291 (2.1%) | 2/394 (0.5%) | 0.09 | ||||||||||||
Health system (VAED and VEMD) | |||||||||||||||
Mean emergency presentations (SD)* | 0.9 (1.7) | 0.66 (1.1) | 0.05 | ||||||||||||
Two or more emergency presentations* | 67/291 (23.0%) | 66/394 (16.8%) | 0.04 | ||||||||||||
Two or more admissions* | 94/291 (32.3%) | 107/394 (27.1%) | 0.14 | ||||||||||||
Stroke emergency presentation* | 14/291 (4.9%) | 10/394 (2.5%) | 0.13 | ||||||||||||
TIA emergency presentation* | 7/291 (2.4%) | 8/394 (2.0%) | 0.28 | ||||||||||||
Stroke or TIA admission* | 15/164 (9.2%) | 13/158 (8.2%) | 0.77 | ||||||||||||
Clinical processes of care (AuSCR) | |||||||||||||||
Admitted to a stroke unit | 284/290 (97.9%) | 388/393 (98.7%) | 0.41 | ||||||||||||
Received thrombolysis | 22/184 (11.9%) | 40/283 (14.1%) | 0.49 | ||||||||||||
Taking an antihypertensive agent at discharge | 250/286 (87.4%) | 331/380 (87.1%) | 0.60 | ||||||||||||
Received a care plan at discharge | 56/286 (19.6%) | 69/379 (18.2%) | 0.07 | ||||||||||||
Health outcomes (AuSCR) | |||||||||||||||
Discharged to home | 135/286 (47.2%) | 160/378 (42.3%) | 0.21 | ||||||||||||
Discharged to aged care facility | 14/286 (4.9%) | 25/378 (6.6%) | 0.35 | ||||||||||||
Discharged to inpatient rehabilitation setting | 116/286 (40.6%) | 170/378 (44.9%) | 0.26 | ||||||||||||
AuSCR = Australian Stroke Clinical Registry. IQR = interquartile range. VAED = Victorian Admitted Episodes Dataset. VEMD = Victorian Emergency Minimum Dataset. TIA = transient ischaemic attack. * Before index event. | |||||||||||||||
6 Factors associated with all-cause hospital readmission within 30 days, 6 months and 1 year after stroke or transient ischaemic attack (TIA)
Adjusted odds ratio (95% CI)* | |||||||||||||||
Factor | 30 days | 6 months | 1 year | ||||||||||||
Female | 1.31 (0.83–2.07) | 1.22 (0.85–1.74) | 1.14 (0.80–1.62) | ||||||||||||
Higher Charlson comorbidity index score | 1.25 (1.11–1.42)† | 1.19 (1.07–1.32)† | 1.19 (1.07–1.32)† | ||||||||||||
Able to walk on admission | 1.46 (0.85–2.52) | 1.09 (0.72–1.67) | 1.04 (0.69–1.56) | ||||||||||||
Documented evidence of previous stroke | 0.89 (0.61–1.33) | 1.01 (0.80–1.27) | 1.01 (0.81–1.27) | ||||||||||||
TIA on index admission | 1.77 (0.93–3.40) | 1.98 (1.19–3.30)† | 2.15 (1.30–3.56)† | ||||||||||||
Two or more emergency presentations before index event | 2.09 (1.25–3.50)† | 1.69 (1.09–2.61)† | 1.57 (1.02–2.43)† | ||||||||||||
* Adjusted for all factors shown. † P < 0.05. | |||||||||||||||
Received 8 January 2015, accepted 1 May 2015
- Monique F Kilkenny1,2
- Helen M Dewey1
- Vijaya Sundararajan3
- Nadine E Andrew1
- Natasha Lannin4
- Craig S Anderson5,6
- Geoffrey A Donnan2
- Dominique A Cadilhac1,2
- 1 Monash University, Melbourne, VIC.
- 2 The Florey Institute of Neuroscience and Mental Health, Melbourne, VIC.
- 3 University of Melbourne, Melbourne, VIC.
- 4 La Trobe University, Melbourne, VIC.
- 5 The George Institute for Global Health, Sydney, NSW.
- 6 Royal Prince Alfred Hospital, Sydney, NSW.
We acknowledge Austin Health for the use of AuSCR data for the pilot project and the Victorian Department of Health for the data linkage of AuSCR to admissions and emergency datasets. Dominique Cadilhac holds a National Health and Medical Research Council (NHMRC) Research Fellowship co-funded by the National Heart Foundation (1063761), and Craig Anderson holds an NHMRC Senior Principal Research Fellowship. Nadine Andrew has an NHMRC Early Career Fellowship (1072053). The AuSCR is supported by funds from the Florey Institute of Neuroscience and Mental Health, the National Stroke Foundation, consumer donations, industry and allocations from the NHMRC Stroke123 Partnership grant.
No relevant disclosures.
- 1. Heller RF, Fisher JD, D'Este CA, et al. Death and readmission in the year after hospital admission with cardiovascular disease: the Hunter Area Heart and Stroke Register. Med J Aust 2000; 172: 261-265.
- 2. Jia H, Zheng Y, Reker DM, et al. Multiple system utilization and mortality for veterans with stroke. Stroke 2007; 38: 355-360.
- 3. Lichtman JH, Jones SB, Watanabe E, et al. Elderly women have lower rates of stroke, cardiovascular events, and mortality after hospitalization for transient ischemic attack. Stroke 2009; 40: 2116-2122.
- 4. Olson DM, Cox M, Pan W, et al. Death and rehospitalization after transient ischemic attack or acute ischemic stroke: one-year outcomes from the adherence evaluation of acute ischemic stroke-longitudinal registry. J Stroke Cerebrovasc Dis 2013; 22: e181-e188.
- 5. Lichtman JH, Leifheit-Limson EC, Jones SB, et al. Predictors of hospital readmission after stroke: a systematic review. Stroke 2010; 41: 2525-2533.
- 6. Cadilhac DA, Lannin NA, Anderson CS, et al. Protocol and pilot data for establishing the Australian Stroke Clinical Registry. Int J Stroke 2010; 5: 217-226.
- 7. Kilkenny MF, Longworth M, Pollack M, et al. Factors associated with 28-day hospital readmission after stroke in Australia. Stroke 2013; 44: 2260-2268.
- 8. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373-383.
- 9. Goldstein LB, Samsa GP, Matchar DB, Horner RD. Charlson Index comorbidity adjustment for ischemic stroke outcome studies. Stroke 2004; 35: 1941-1945.
- 10. Belsley DA, Kuh E, Welsch RE. Regression diagnostics: identifying influential data and sources of collinearity. Hoboken, NJ: John Wiley & Sons, 1980.
- 11. Cadilhac DA, Sundararajan V, Andrew N, et al. Using linked data to more comprehensively measure the quality of care for stroke – understanding the issues. Australasian Epidemiologist 2013; 20 (1): 15-19.
- 12. Norrish A, North D, Kirkman P, Jackson R. Validity of self-reported hospital admission in a prospective study. Am J Epidemiol 1994; 140: 938-942.
- 13. Lee HC, Chang KC, Huang YC, et al. Readmission, mortality, and first-year medical costs after stroke. J Chin Med Assoc 2013; 76: 703-714.
- 14. Bohannon RW, Lee N. Hospital readmissions and deaths during the first year after hospitalization for stroke. Conn Med 2003; 67: 535-539.
- 15. Sun Y, Toh MP. Impact of diabetes mellitus (DM) on the health-care utilization and clinical outcomes of patients with stroke in Singapore. Value Health 2009; 12 Suppl 3: S101-S105.
- 16. Langagergaard V, Palnum KH, Mehnert F, et al. Socioeconomic differences in quality of care and clinical outcome after stroke: a nationwide population-based study. Stroke 2011; 42: 2896-2902.
- 17. Li HW, Yang MC, Chung KP. Predictors for readmission of acute ischemic stroke in Taiwan. J Formos Med Assoc 2011; 110: 627-633.
- 18. Tseng MC, Lin HJ. Readmission after hospitalization for stroke in Taiwan: results from a national sample. J Neurol Sci 2009; 284: 52-55.
- 19. Bohannon RW, Lee N. Association of physical functioning with same-hospital readmission after stroke. Am J Phys Med Rehabil 2004; 83: 434-438.
- 20. Kennedy BS. Does race predict stroke readmission? An analysis using the truncated negative binomial model. J Natl Med Assoc 2005; 97: 699-713.
- 21. Camberg LC, Smith NE, Beaudet M, et al. Discharge destination and repeat hospitalizations. Med Care 1997; 35: 756-767.
- 22. Webster F, Saposnik G, Kapral MK, et al. Organized outpatient care: stroke prevention clinic referrals are associated with reduced mortality after transient ischemic attack and ischemic stroke. Stroke 2011; 42: 3176-3182.





Abstract
Objectives: To assess the feasibility of linking a national clinical stroke registry with hospital admissions and emergency department data; and to determine factors associated with hospital readmission after stroke or transient ischaemic attack (TIA) in Australia.
Design and setting: Data from the Australian Stroke Clinical Registry (AuSCR) at a single Victorian hospital were linked to coded, routinely collected hospital datasets for admissions (Victorian Admitted Episodes Dataset) and emergency presentations (Victorian Emergency Minimum Dataset) in Victoria from 15 June 2009 to 31 December 2010, using stepwise deterministic data linkage techniques.
Main outcome measures: Association of patient characteristics, social circumstances, processes of care and discharge outcomes with all-cause readmissions within 1 year from time of hospital discharge after an index admission for stroke or TIA.
Results: Of 788 patients registered in the AuSCR, 46% (359/781) were female, 83% (658/788) had a stroke, and the median age was 76 years. Data were successfully linked for 782 of these patients (99%). Within 1 year of their index stroke or TIA event, 42% of patients (291/685) were readmitted, with 12% (35/286) readmitted due to a stroke or TIA. Factors significantly associated with 1-year hospital readmission were two or more presentations to an emergency department before the index event (adjusted odds ratio [aOR], 1.57; 95% CI, 1.02–2.43), higher Charlson comorbidity index score (aOR, 1.19; 95% CI, 1.07–1.32) and diagnosis of TIA on the index admission (aOR, 2.15; 95% CI, 1.30–3.56).
Conclusions: Linking clinical registry data with routinely collected hospital data for stroke and TIA is feasible in Victoria. Using these linked data, we found that readmission to hospital is common in this patient group and is related to their comorbid conditions.