Lipid-lowering drugs (LLD), especially statins, are of proven benefit in preventing future coronary heart disease (CHD), both recurrent events and first events in those at high coronary risk.1-3 The Organisation for Economic Co-operation and Development (OECD) noted that consumption of LLD in Australia in 2011 was the highest of 23 countries reported.4 The rate was 50% higher than the OECD average and had risen more than 300% since 2000.4
Given this high level of use, it is important to know whether LLD are being prescribed for the correct mix of patients. The Australian ACACIA registry reported that statins were prescribed for 75%–89% of patients with acute coronary syndrome in 2005–2007, with the rate varying depending on the clinical presentation.5 Similarly, a large European survey of patients with CHD reported that 89% had been prescribed statins in 2006–2007,6 while a companion survey in the general practice setting found that 47% of “high-risk” patients with hypercholesterolaemia had been prescribed statins.7
The AusHEART study, an Australian general practice survey of risk factor perception and management in 2008, found that 50% of patients with established cardiovascular disease were prescribed a combination of statin, antihypertensive and antiplatelet therapy.8 Only a third of patients without established cardiovascular disease but at high risk of a first event were prescribed statin and antihypertensive medication.8 The AusDiab Study in 2011–2012 reported that 60% of people with diabetes were using statins.9 None of these outcomes take into account the poor long-term persistence in patients prescribed these and other cardiovascular drugs.10-12
In previous studies, we have used the Pharmaceutical Benefits Scheme (PBS) database to explore patient behaviour in those prescribed various medications.10-12 The database also contains information on co-prescriptions, which can be used as a surrogate for accompanying medical conditions. Here, we used the PBS database to explore whether patients arbitrarily defined as being at high coronary risk (those with prior CHD, diabetes or hypertension) are receiving LLD as they should, according to contemporary prevention guidelines.2,3
Methods
Data source
Dispensing is only recorded in the PBS database for patients classified as concession card holders, who are nevertheless estimated to represent 65% of all patients receiving statins.13 We analysed PBS pharmacy payment claim records for a 10% random sample of the included population. The data were drawn from de-identified records held by Medicare Australia, via the Department of Human Services, for the period January 2006 through May 2013, inclusive. Various statin drugs were priced below the general patient copayment threshold for some or all of this period, and no record of their prescription would have been sent to the PBS. Hence, our study was limited to patients who had received > 90% of their PBS prescriptions on a concessional basis during the study period, indicating that they were long-term concession card holders. Prescriptions for LLD included statins, fibrates and ezetimibe, although statin drugs were predominant.
Definition of surrogates
Groups of patients at high risk of future CHD were arbitrarily defined by the following co-prescriptions:
- CHD: antiplatelet drugs (clopidogrel, prasugrel, not solo aspirin) and anti-anginal drugs (nitrates, nicorandil, perhexiline)
- Diabetes: all standard drugs
- Hypertension: all standard drugs (not solo diuretics).
To be classified in a high-risk group, patients needed to have three prescriptions for the specified drugs within 6 months at any time during the study period. Patients could belong to multiple groups.
Ethics approval
Patient identities remained anonymous during this investigation. Ethics and publication approval was obtained from the External Request Evaluation Committee of Medicare Australia.
Results
We extracted information from the PBS claims database on 853 836 concessional patients who had received PBS drugs during the study period (representative of 8 538 360 patients nationally). Of these, we classified 276 212 (32%) as being at high coronary risk. A comparison of the Australian population distribution with the concessional and high coronary risk populations is shown in Box 1. Compared with the Australian population, the distribution of concessional patients was shifted towards older age groups. High coronary risk patients were older than the overall concessional group (mean age, 66.1 [SD, 14.8] years, 44% male v 47.9 [SD, 28.0] years, 45% male).
Of the total concessional group, 657 454 patients (77%) were not prescribed any LLD during the study period. Of the total high coronary risk group, 115 477 (42%) were not prescribed any LLD.
Among the clinical groups of high-risk patients not receiving LLD, there were minor variations by age and sex (Box 2). For patients in a single risk-factor group, the proportion not receiving LLD was lowest in the CHD group (40%). For patients in multiple risk-factor groups, the proportions not receiving LLD were lower, down to 8% in the CHD + diabetes + hypertension group. Among all CHD groups combined, 19% of patients were not receiving LLD.
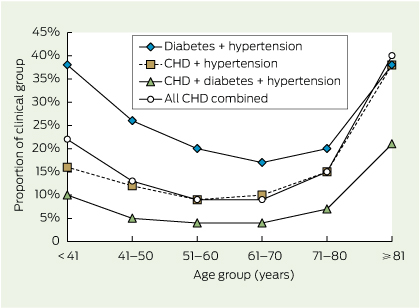
The proportions of patients in high-risk groups not receiving LLD are shown by age groups in Box 3. Across all risk groups, the proportions not receiving LLD were generally higher in the youngest and oldest age groups and lowest in those aged 51–70 years. This U-shaped relationship in the proportions not receiving LLD by age is clearly apparent for the largest multiple risk-factor groups in Box 4.
Discussion
Australia's national guidelines for the primary or secondary prevention of CHD provide a general framework for appropriate management of all risk factors.2,3 However, such therapy needs to be individualised according to background risk, prognosis, comorbidities, drug tolerance, lifestyle and living circumstances, and personal choices.2,3 Hence, there can be no simple threshold for the proportion of people not treated that would signify undertreatment. Using conservative definitions for high coronary risk, we identified that the proportions of patients with multiple risk factors who were not receiving LLD are generally low, particularly in the CHD + diabetes + hypertension risk group.
Our findings are broadly consistent with Australian data for patients with CHD5 or diabetes,9 as well as data from Europe.6,7 The AusHEART study reported much higher proportions of patients with cardiovascular disease or at high risk of disease who were not receiving statins, antihypertensive therapy or antiplatelet drugs,8 but the findings were derived from general practice surveys and are not strictly comparable with administrative data from the PBS database.
We found that the concessional patient population was older than the Australian population and, not surprisingly, that the high coronary risk population was older still. The proportions of patients aged 71–80 and ≥ 81 years in the high-risk population were about fivefold those in the Australian population, reflecting a greater presence or risk of disease. The finding that greater proportions of those aged ≥ 81 years, and to a lesser extent those under 41 years, were not receiving LLD across all clinical groups is intriguing. This may represent a form of age discrimination and may not be consistent with national guidelines.2,3 The PBS database contains no further clinical information that might explain the behaviour of prescribers, but if there is a genuine bias against lipid-lowering therapy in these age groups, further research and education will be required.
There are limitations in our analysis. It was restricted to concessional patients; however, we have previously noted that concession card holders account for two-thirds of statin use.13 As the PBS database is administrative, with no relevant clinical information, we had no information on how well risk factors are controlled in these patients. The clinical definitions of high coronary risk we employed were conservative and would have good ability to identify high-risk patients, but would be less reliable in identifying those not at high risk. Very few patients using the nominated drugs would be misclassified as having CHD. There is minimal use of metformin in patients without diabetes (much less so in older patients), while some antihypertensive drugs are used for other indications, notably CHD. The major strength of our analysis is the use of a large, nationwide database.
Despite our study's limitations, we also examined the reciprocal question of whether too many “low-risk” patients are receiving LLD. After subtracting data for the high-risk group from the total dataset of 853 836 concessional patients, we calculated that only 7% of those not identified as being at high coronary risk were receiving LLD. At limited face value, this is an encouraging statistic, given the high use of statin drugs in Australia.4
Our study suggests a large proportion of patients at high coronary risk, especially those with CHD and multiple risk factors, are being appropriately prescribed LLD in Australia. However, long-term persistence of therapy remains problematic10 and we have no information on how well risk factors are controlled. While use of LLD in Australia may be very high, it appears that middle-aged concession card holders at high coronary risk are being well managed.
1 Comparison of Australian population distribution with concessional and high coronary risk populations, by age*
Age group (years) | |||||||||||||||
Population | < 41 | 41–50 | 51–60 | 61–70 | 71–80 | ≥ 81 | |||||||||
Australian population (n = 22 710 352) | 12 546 208 (55%) | 3 143 550 (14%) | 2 827 714 (12%) | 2 165 462 (10%) | 1 255 465 (6%) | 771 953 (3%) | |||||||||
Concessional patients (n = 853 836) | 367 141 (43%) | 73 628 (9%) | 63 695 (7%) | 90 591 (11%) | 135 129 (16%) | 123 618 (14%) | |||||||||
High coronary risk patients (n = 276 212) | 11 429 (4%) | 17 122 (6%) | 35 793 (13%) | 88 210 (32%) | 82 816 (30%) | 40 842 (15%) | |||||||||
* Estimated Australian population at 30 June 2012.14 The other two groups are based on a 10% random sample of the Pharmaceutical Benefits Scheme database. Percentages refer to proportion of the population group (eg, 55% of the Australian population were aged < 41 years). | |||||||||||||||
2 Mean age, sex and proportions of high coronary risk patients not receiving lipid-lowering drugs (LLD), by clinical group
Clinical group | No. of patients | Mean age (SD), years | Male | Not receiving LLD | |||||||||||
CHD alone | 6 696 | 74 (13) | 3 375 (50%) | 2 676 (40%) | |||||||||||
Diabetes alone | 12 713 | 68 (13) | 6 191 (49%) | 7 007 (55%) | |||||||||||
Hypertension alone | 166 094 | 53 (20) | 66 105 (40%) | 88 942 (54%) | |||||||||||
Diabetes + hypertension | 39 772 | 65 (12) | 18 971 (48%) | 8 543 (21%) | |||||||||||
CHD + diabetes | 853 | 74 (11) | 465 (55%) | 215 (25%) | |||||||||||
CHD + hypertension | 35 827 | 71 (13) | 17 161 (48%) | 6 983 (19%) | |||||||||||
CHD + diabetes + hypertension | 14 257 | 70 (10) | 7 884 (55%) | 1 111 (8%) | |||||||||||
All CHD groups | 57 633 | 66 (15) | 28 817 (50%) | 10 985 (19%) | |||||||||||
CHD = coronary heart disease. | |||||||||||||||
3 Numbers and proportions of high coronary risk patients not receiving lipid-lowering drugs, by clinical and age groups*
Age group (years) | |||||||||||||||
Clinical group | < 41 | 41–50 | 51–60 | 61–70 | 71–80 | ≥ 81 | |||||||||
CHD alone | |||||||||||||||
No. (%) | 56/104 (54%) | 88/239 (37%) | 141/512 (28%) | 312/1480 (21%) | 627/2023 (31%) | 1452/2338 (62%) | |||||||||
P | 0.000 | 0.000 | 0.003 | reference | 0.000 | 0.000 | |||||||||
Diabetes alone | |||||||||||||||
No. (%) | 2680/3272 (82%) | 981/1894 (52%) | 871/2118 (41%) | 1131/2822 (40%) | 795/1800 (44%) | 549/807 (68%) | |||||||||
P | 0.000 | 0.000 | ns | reference | 0.006 | 0.000 | |||||||||
Hypertension alone | |||||||||||||||
No. (%) | 4981/6173 (81%) | 7537/10 579 (71%) | 12 297/21 806 (56%) | 27 210/56 274 (48%) | 22 310/48 471 (46%) | 14 607/22 791 (64%) | |||||||||
P | 0.000 | 0.000 | 0.000 | ns | reference | 0.000 | |||||||||
Diabetes + hypertension | |||||||||||||||
No. (%) | 546/1451 (38%) | 794/3049 (26%) | 1429/7147 (20%) | 2394/14 120 (17%) | 2207/10 901 (20%) | 1173/3104 (38%) | |||||||||
P | 0.000 | 0.000 | 0.000 | reference | 0.000 | 0.000 | |||||||||
CHD + diabetes | |||||||||||||||
No. (%) | 4/17 (24%) | 7/41 (17%) | 13/109 (12%) | 27/201 (13%) | 65/275 (24%) | 99/210 (47%) | |||||||||
P | ns | ns | reference | ns | 0.010 | 0.000 | |||||||||
CHD + hypertension | |||||||||||||||
No. (%) | 45/279 (16%) | 97/823 (12%) | 221/2418 (9%) | 864/8789 (10%) | 2098/13 918 (15%) | 3658/9600 (38%) | |||||||||
P | 0.000 | 0.028 | reference | ns | 0.000 | 0.000 | |||||||||
CHD + diabetes + hypertension | |||||||||||||||
No. (%) | 13/133 (10%) | 23/497 (5%) | 64/1683 (4%) | 180/4524 (4%) | 402/5428 (7%) | 428/1992 (21%) | |||||||||
P | 0.001 | ns | reference | ns | 0.000 | 0.000 | |||||||||
All CHD combined | |||||||||||||||
No. (%) | 118/533 (22%) | 215/1600 (13%) | 439/4722 (9%) | 1384/14 994 (9%) | 3192/21 644 (15%) | 5637/14 140 (40%) | |||||||||
P | 0.000 | 0.000 | reference | ns | 0.000 | 0.000 | |||||||||
CHD = coronary heart disease. ns = not significant (P > 0.05). * Percentages refer to the proportion of the clinical group. There was a pairwise comparison in each clinical group with the reference age category. The age category with the smallest percentage was used as the reference, employing a two-tailed Z test. | |||||||||||||||
Received 24 February 2014, accepted 26 May 2014
- Leon A Simons1
- Eric Chung2
- 1 Lipid Research Department, University of New South Wales and St Vincent's Hospital, Sydney, NSW.
- 2 Prospection Pty Ltd, Sydney, NSW.
This work was supported by a grant from Amgen Australia. Raw data for the study were supplied by Medicare Australia.
No relevant disclosures.
- 1. Cholesterol Treatment Trialists' (CTT) Collaboration; Baigent C, Blackwell L, Emberson J, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 2010; 376: 1670-1681.
- 2. National Heart Foundation of Australia, Cardiac Society of Australia and New Zealand. Reducing risk in heart disease: an expert guide to clinical practice for secondary prevention of coronary heart disease. Melbourne: NHF, 2012. http://www.heartfoundation.org.au/SiteCollectionDocuments/Reducing-risk-in-heart-disease.pdf (accessed May 2014).
- 3. National Vascular Disease Prevention Alliance. Absolute cardiovascular disease risk management. Quick reference guide for health professionals. National Stroke Foundation, 2012. http://strokefoundation.com.au/site/media/NVDPA-Managment-Guideline-Quick-Reference-Guide.pdf (accessed May 2014).
- 4. Organisation for Economic Co-operation and Development. Health at a glance 2013: OECD indicators. OECD Publishing, 2013. http://dx.doi.org/10.1787/health_glance-2013-en (accessed Apr 2014).
- 5. Chew DP, Amerena JV, Coverdale SG, et al. Invasive management and late clinical outcomes in contemporary Australian management of acute coronary syndromes: observations from the ACACIA registry. Med J Aust 2008; 188: 691-697. <MJA full text>
- 6. Reiner Ž, De Bacquer D, Kotseva K, et al. Treatment potential for dyslipidaemia management in patients with coronary heart disease across Europe: findings from the EUROASPIRE III survey. Atherosclerosis 2013; 231: 300-307.
- 7. Kotseva K, Wood D, De Backer G, et al. EUROASPIRE III. Management of cardiovascular risk factors in asymptomatic high-risk patients in general practice: cross-sectional survey in 12 European countries. Eur J Cardiovasc Prev Rehabil 2010; 17: 530-540.
- 8. Heeley EL, Peiris DP, Patel AA, et al. Cardiovascular risk perception and evidence–practice gaps in Australian general practice (the AusHEART study). Med J Aust 2010; 192: 254-259. <MJA full text>
- 9. Tanamas SK, Magliano DJ, Lynch B, et al. AusDiab 2012: the Australian Diabetes, Obesity and Lifestyle Study. Melbourne: Baker IDI Heart and Diabetes Institute, 2013. http://www.bakeridi.edu.au/Assets/Files/Baker%20IDI%20Ausdiab%20Report_interactive_FINAL.pdf (accessed May 2014).
- 10. Simons LA, Ortiz M, Calcino G. Persistence with antihypertensive medication: Australia-wide experience, 2004-2006. Med J Aust 2008; 188: 224-227. <MJA full text>
- 11. Simons LA, Ortiz M, Calcino G. Long term persistence with statin therapy – experience in Australia 2006-2010. Aust Fam Physician 2011; 40: 319-322.
- 12. Simons LA, Ortiz M, Germanos P, Calcino G. Persistence on warfarin in patients with atrial fibrillation: experience in Australia 2006-2009. Aust Fam Physician 2013; 42: 659-661.
- 13. Drug Utilisation Sub-committee, Pharmaceutical Benefits Advisory Committee. Pharmaceutical Benefits Scheme under copayment prescription data (data available on request). Canberra: Department of Health and Ageing, 2010.
- 14. Australian Bureau of Statistics. Australian demographic statistics, Dec 2012. Data cubes, population by age and sex tables, table 8. (ABS Cat. No. 3101.0.) http://ww.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3101.0Dec%202012 (accessed May 2014).





Abstract
Objective: To examine whether high coronary risk patients in Australia, where use of lipid-lowering drugs (LLD) is very high by international standards, are receiving LLD.
Design, setting and patients: Assessment of Pharmaceutical Benefits Scheme pharmacy payment claim records between January 2006 and May 2013 for a 10% random sample of Australian concession card holders. Co-prescriptions were used as a surrogate for high coronary risk groups — coronary heart disease (CHD): antiplatelet drugs (not including solo aspirin) and anti-anginal drugs; diabetes: all standard drugs; hypertension: all standard drugs (not including solo diuretics).
Main outcome measure: Proportions of patients in high-risk groups not receiving LLD (statins, fibrates or ezetimibe).
Results: The database yielded information on 276 212 patients defined as being at high coronary risk (mean age, 66.1 [SD, 14.8] years; 44% male). Of this group, 115 477 patients (42%) had not received any LLD during the study period. For patients in the risk group for CHD in combination with diabetes and hypertension, only 8% (1111/14 257) were not receiving LLD. Across all risk groups, the proportions not receiving LLD were generally highest in those aged ≥ 81 years and, to a lesser extent, < 41 years, and were lowest in those aged 51–70 years.
Conclusion: A large proportion of concession card holders at high coronary risk, especially those in middle age with CHD and multiple risk factors, are being appropriately prescribed LLD in Australia.