Clinical record
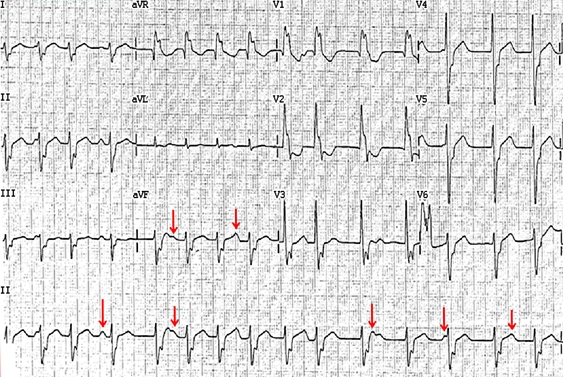
A 64-year-old man with no significant past medical history presented to a district hospital in June 2012 with a 3-week history of palpitations and breathlessness. The electrocardiogram (ECG) showed an irregularly irregular wide complex tachycardia at a rate of 150 beats/min with right bundle branch block-like morphology (Box 1). A transthoracic echocardiogram showed moderate segmental left ventricular dysfunction. Coronary angiography showed no evidence of significant coronary artery disease to account for his left ventricular impairment. A diagnosis of atrial fibrillation (AF) with a rapid ventricular response and tachycardia-mediated cardiomyopathy was made.
Therapy with diuretics and antiarrhythmic medications was commenced. Despite substantial doses of amiodarone (600 mg daily), metoprolol (200 mg daily), verapamil (240 mg daily) and digoxin (250 µg daily) over 2 weeks, his heart rate remained uncontrolled at between 100 and 200 beats/min. A transoesophageal echocardiogram-guided cardioversion was performed, but failed to restore normal rhythm. He was subsequently referred to our tertiary cardiac centre for further management.
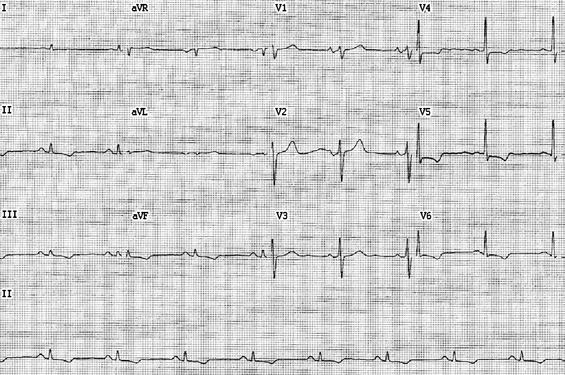
The patient was haemodynamically stable on arrival. He had mild renal impairment (creatinine level, 114 µmol/L [reference interval (RI), 60–110 µmol/L]; estimated glomerular filtration rate, 56 mL/min/1.73 m2 [RI, > 90 mL/min/1.73 m2]), normal levels of troponin I (0.02 µg/L [RI, 0–0.08 µg/L]), creatine kinase (100 U/L [RI, 52–336 U/L]) and electrolytes (sodium, 139 mmol/L [RI, 135–145 mmol/L]; potassium, 4.2 mmol/L [RI, 3.5–5.0 mmol/L]), and normal findings on thyroid function tests. Although his ECG showed an irregularly irregular broad complex tachycardia suggestive of AF, closer inspection of the ECG showed P waves of probable sinus bradycardia with atrioventricular dissociation (Box 1, red arrows) indicative of ventricular tachycardia (VT). A repeat echocardiogram showed moderately impaired left ventricular function (ejection fraction, 35%–40% [RI, 55%–75%]) due to global hypokinesis. The patient had incessant VT throughout an electrophysiology study that was performed. Three-dimensional electro-anatomical mapping (Ensite NavX, St Jude Medical) identified a VT focus emanating from the base of the posteromedial papillary muscle of the left ventricle. Ablation at this focus terminated the VT with no further ectopic activity. His ECG after the ablation showed sinus rhythm (Box 2). He has remained well since discharge, taking only a low daily dose of bisoprolol (1.25 mg). Six months after the ablation, a 24-hour Holter monitor has not detected any recurrence of VT, and a repeat echocardiogram showed normalisation of left ventricular function.
The differential diagnoses of broad complex tachycardia include ventricular tachycardia (VT), supraventricular tachycardia with aberrancy and a ventricular paced rhythm. The diagnosis of broad complex tachycardia remains challenging despite various criteria having been established to differentiate VT from supraventricular tachycardia with aberrancy.1,2 The patient's initial presenting electrocardiogram (ECG) was misdiagnosed as atrial fibrillation (AF) because of the irregularly irregular rhythm. In VT, the rhythm is usually regular or almost regular but beat-to-beat variations can occur in the presence of captured beats (when an atrial impulse causes depolarisation via the normal conduction system, resulting in a narrow QRS complex occurring earlier than expected) or fusion beats (when an appropriately timed sinus impulse fuses with the wide QRS complex from VT to produce a relatively narrowed QRS complex). In addition to an irregularly irregular rhythm, however, the diagnosis of AF requires the absence of P waves, and fibrillation of the baseline (f waves); neither feature was evident on the patient's initial ECG.
The 12-lead ECG provides important clues in differentiating VT from supraventricular tachycardia. Atrioventricular (AV) dissociation with more ventricular impulses than atrial is one of the most useful criteria for distinguishing VT from supraventricular tachycardia.3 It occurs in 20%–50% of cases of VT and almost never in supraventricular tachycardia, with the rare exception of junctional ectopic tachycardia.4 Absence of AV dissociation does not exclude the diagnosis of VT. Importantly, beat-to-beat differences (especially of the ST segment and T waves) may raise the possibility of obscured independent P wave activity (red arrows in Box 1).
The absence of an RS complex in any precordial lead during a tachycardia with a wide QRS complex makes the diagnosis of a VT highly specific.5 If an RS complex is present in one or more precordial leads, the next step is to measure the longest RS interval. This is the intrinsic deflection, measured from the onset of the R wave to the deepest part of the S wave, and should be longer in VT (> 100 ms) than in supraventricular tachycardia, irrespective of the QRS morphology.5
In our patient, there was extreme axis deviation (“north-west” axis) during tachycardia with predominantly negative QRS complexes in leads I, II and III (Box 1). A frontal axis between − 90° to ±180° cannot be achieved by any combination of bundle branch block and therefore suggests VT.3 Also QRS duration greater than 160 ms (not applicable in this case) is strongly suggestive of VT.
VT and supraventricular tachycardia with bundle branch block may produce similar ECGs. If a previous ECG shows a bundle branch block pattern during sinus rhythm that is similar or identical to that during the tachycardia, the origin of the tachycardia is likely to be supraventricular.3 However, if the QRS morphology changes during tachycardia, VT is more likely.
In general, all broad complex tachycardias should be treated as if the rhythm was VT until proven otherwise. Delay or misdiagnosing VT with an inappropriate treatment can lead to fatal or almost fatal outcomes.6 Twelve-lead electrocardiography remains an important tool in the diagnosis of VT; if there is any doubt, an expert opinion should be obtained to prevent any delay in management.
Traditional understanding held that ventricular arrhythmias are a consequence of an underlying cardiomyopathy. However, more recent evidence shows that frequent premature ventricular beats or sustained VT can precipitate left ventricular impairment in otherwise normal hearts.7 Numerous ventricular foci for these arrhythmias have been reported.7 Although it is uncommon, papillary muscles can give rise to ventricular arrhythmias in normal hearts without previous infarcts.8,9 The mechanism of this VT is postulated to be either due to triggered activity (delayed after depolarisations) or abnormal automaticity (non-re-entrant), which might account for the irregularity of the VT.7,9 Importantly, ventricular dysfunction is reversible with appropriate treatment, and excellent clinical outcomes from radiofrequency catheter ablation for papillary muscle VT have been reported, as was the case in our patient.10
- 1. Wellens HJ, Bar FW, Lie KI. The value of the electrocardiogram in the differential diagnosis of a tachycardia with a widened QRS complex. Am J Med 1978; 64: 27-33.
- 2. Kindwall KE, Brown J, Josephson ME. Electrocardiographic criteria for ventricular tachycardia in wide complex left bundle branch block morphology tachycardias. Am J Cardiol 1988; 61: 1279-1283.
- 3. Eckardt L, Breithardt G, Kirchhof P. Approach to wide complex tachycardias in patients without structural heart disease. Heart 2006; 92: 704-711.
- 4. Liu CF, Ip JE, Lin AC, Lerman BB. Mechanistic heterogeneity of junctional ectopic tachycardia in adults. Pacing Clin Electrophysiol 2013; 36: e7-e10.
- 5. Brugada P, Brugada J, Mont L, et al. A new approach to the differential diagnosis of a regular tachycardia with a wide QRS complex. Circulation 1991; 83: 1649-1659.
- 6. Stewart RB, Bardy GH, Greene HL. Wide complex tachycardia: misdiagnosis and outcome after emergent therapy. Ann Intern Med 1986; 104: 766-771.
- 7. Baman TS, Lange DC, Ilg KJ, et al. Relationship between burden of premature ventricular complexes and left ventricular function. Heart Rhythm 2010; 7: 865-869.
- 8. González H, Torres A, Lerma C, et al. [Arrhythmic activity of the papillary muscle induced by high frequency stimulation: n1 rhythms, transition forms and hysteresis] [Spanish]. Arch Cardiol Mex 2004; 74: 11-24.
- 9. Doppalapudi H, Yamada T, McElderry HT, et al. Ventricular tachycardia originating from the posterior papillary muscle in the left ventricle: a distinct clinical syndrome. Circ Arrhythm Electrophysiol 2008; 1: 23-29.
- 10. Bogun F, Crawford T, Reich S, et al. Radiofrequency ablation of frequent, idiopathic premature ventricular complexes: comparison with a control group without intervention. Heart Rhythm 2007; 4: 863-867.





No relevant disclosures.