A 72-year-old man developed septic arthritis in a prosthetic shoulder after intra-articular injection of radiographic contrast. This is the first published case in which molecular techniques matched oral commensal organisms cultured from joint aspirate with oral flora from the proceduralist, who was not wearing a mask.
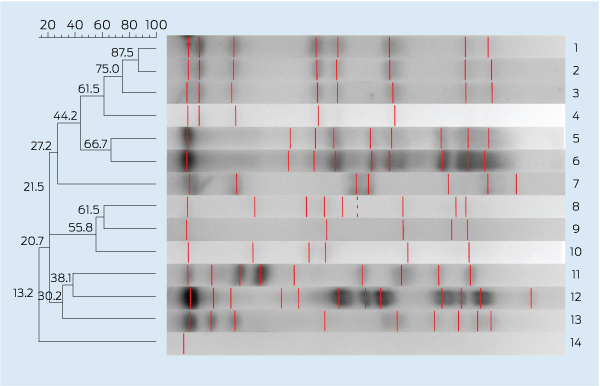
Shortly after the patient presented, the proceduralist agreed to provide an oropharyngeal swab. Several organisms were cultured, including multiple viridans Streptococcus species. Pulsed-field gel electrophoresis (PFGE) was performed according to the method of Lefevre et al, with modifications.1 Using two different restriction enzymes (SmaI, ApaI), we found that the patient’s organism and a strain of S. mitis recovered from the proceduralist’s throat showed indistinguishable fragment patterns (Box). This strongly suggested droplet transmission of the proceduralist’s oral flora onto the needle or skin, with subsequent inoculation into the shoulder joint.
Australian Medicare data for the period 2006–2009 show that an average of 516 562 claims were made annually for joint injections or aspirations.2 The estimated incidence of septic arthritis after intra-articular corticosteroid injection into a native joint is estimated to be between 1 per 3000 and 1 per 16 000 injections.3 Applying these incidence rates to Australian data, we would estimate that between 30 and 180 instances of iatrogenic septic arthritis per year are a result of joint injection or aspiration. It could be safely assumed that even fewer of these could be attributed to omission of a surgical mask. Given this apparently low burden of disease, should a surgical mask be a mandatory requirement of an aseptic technique for this procedure?
Infection control practices during the injection of sterile sites vary substantially across specialties and depend on the type of procedure and where it is performed (general practice, wards, operating theatres). Several studies confirm the anecdotal evidence that mask-wearing while injecting into sterile sites is not standard practice across a number of specialties, including rheumatology,4 obstetric anaesthesia5 and general practice.6 In some series, the rate is as low as 11%, and a debate exists in the surgical literature about whether surgical masks should be used at all in operating theatres.6
However, there is good microbiological evidence that oral bacterial flora, of which oral (viridans) streptococci predominate, can be deposited on an agar plate held at 30 cm from a speaking subject’s mouth for a period of 5 minutes.7 Thus, if a mask is omitted, procedures such as spinal anaesthesia, or any teaching procedure that can involve speaking to the patient or observers, may result in increased risk of contamination of the sterile field.
In the context of iatrogenic septic arthritis, viridans streptococci are infrequently identified as pathogens.8 They are regarded as low virulence organisms and are often dismissed as contaminants when recovered from joint aspirates. This may lead to an underestimation of their significance as pathogens in this context.
However, viridans streptococci have been implicated in other settings as nosocomial pathogens, most spectacularly with bacterial meningitis after spinal anaesthesia or myelography. A review of 179 cases of iatrogenic meningitis provides corroborative evidence that low virulence organisms can be dispersed from the oropharynx to sterile sites and cause infection.9 The evidence indicates that the risk of meningitis is far higher when there is inoculation into a sterile site (eg, spinal anaesthesia) than simple needle puncture of the site (eg, lumbar puncture). Similarly, the risk of iatrogenic septic arthritis is likely to be greater with inoculation than aspiration alone. That a low virulence organism can cause such morbidity, and occasionally death from meningitis, likely relates to the breach of usual host immune defences by direct inoculation into the site of infection. On rare occasions molecular confirmation of the source, using either PFGE or polymerase chain reaction, has been documented after recovery of identical organisms from the oropharynx of the proceduralist.10
It is always challenging to prove relatedness of bacterial strains, as typing techniques are often dependent on the specific bacterial species. PFGE has been shown to be a reliable technique for differentiating strains of S. mitis in other studies.11,12 In our case, the use of two different restriction endonucleases with identical results adds robustness to the data. While molecular methods can only ever prove two bacterial strains are different, there are established criteria for relatedness.13 The combination of our two pulsed-field gels satisfies the Tenover criteria for indistinguishable strains.
Some authors have suggested that the efficacy of surgical masks is unproven, and that viridans streptococci may be introduced in ways other than direct contamination from the oropharynx.14 In particular, it has been suggested that transmission could be explained by more general deficiencies in aseptic technique, including contamination of the equipment during set-up or improper skin sterilisation. However, the compelling evidence that oral commensal bacteria can be aerosolised, and molecular confirmation of the source in several cases, including our own, would suggest that a surgical mask serves a role in aseptic technique.
Pulsed-field gel electrophoresis dendrogram: Streptococcus mitis isolates from the patient’s joint fluid (Lane 1), and the proceduralist’s oropharynx (Lane 2 and Lane 3), showing an indistinguishable restriction fragment pattern. The lanes below are other oral Streptococcus isolates from the proceduralist along with control organisms
- 1. Lefevre JC, Faucon G, Sicard AM, Gasc AM. DNA fingerprinting of Streptococcus pneumoniae strains by pulsed-field gel electrophoresis J Clin Microbiol 1993; 31: 2724-2728.
- 2. Australian Government Department of Health and Ageing. Medicare Australia Statistics 2013 [updated 25 Jan 2013]. https://www.medicareaustralia.gov.au/cgi-bin/broker.exe?_PROGRAM=sas.mbs_item_standard_report.sas&_SERVICE=default&DRILL=ag&_DEBUG=0&group=50124%2C+50125&VAR=services&STAT=count&RPT_FMT=by+state&PTYPE=finyear&START_DT=200607&END_DT=200906 (accessed Feb 2013).
- 3. Von Essen R, Savolainen HA. Bacterial infection following intra-articular injection: a brief review. Scand J Rheumatol 1989; 18: 7-12.
- 4. Haslock I, Macfarlane D, Speed C. Intra-articular and soft tissue injections: a survey of current practice. Br J Rheumatol 1995; 34: 449-452.
- 5. Panikkar KK, Yentis SM. Wearing of masks for obstetric regional anaesthesia: a postal survey. Anaesthesia 1996; 51: 398-400.
- 6. Davis P, Spady D, Forgie SE. A survey of Alberta physicians’ use of and attitudes toward face masks and face shields in the operating room setting. Am J Infect Control 2007; 35: 455-459.
- 7. Philips BJ, Fergusson P, Armstrong P, et al. Surgical face masks are effective in reducing bacterial contamination caused by dispersal from the upper airway. Br J Anaesth 1992; 69: 407-408.
- 8. Armstrong RW, Bolding F, Joseph R. Septic arthritis following arthroscopy: clinical syndromes and analysis of risk factors. Arthroscopy 1992; 8: 213-223.
- 9. Baer ET. Post-dural puncture bacterial meningitis. Anesthesiology 2006; 105: 381-393.
- 10. Veringa E, Van Belkum A, Schellekens H. Iatrogenic meningitis by Streptococcus salivarius following lumbar puncture. J Hosp Infect 1995; 29: 316-318.
- 11. Wisplinghoff H, Reinert RR, Cornely O, Seifert H. Molecular relationships and antimicrobial susceptibilities of viridans group streptococci isolated from blood of neutropenic cancer patients. J Clin Microbiol 1999; 37: 1876-1880.
- 12. Lu H, Weng X, Zhu B, et al. Major outbreak of toxic shock-like syndrome caused by Streptococcus mitis. J Clin Microbiol 2003; 41: 3051-3055.
- 13. Tenover FC, Arbeit RD, Goering RV, et al. Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J Clin Microbiol 1995; 33: 2233-2239.
- 14. Black SR, Weinstein RA. The case for face masks — Zorro or zero? Clin Infect Dis 2000; 31: 522-523.





No relevant disclosures.