Chlamydia, caused by the bacteria Chlamydia trachomatis, is a sexually transmitted infection (STI) and the most commonly notified disease in Australia and in Western Australia.1 Between 2001 and 2010, the number of chlamydia infections reported to the Department of Health, WA (DoHWA) increased more than threefold, from 2707 notifications in 2001 to 10 249 in 2010.2 As in previous years, 84% of the chlamydia notifications in WA in 2010 were among young people (age, < 30 years), with peaks in those aged 20–24 and 15–19 years (36% and 28% of notifications, respectively).2 As asymptomatic chlamydia infection is common among men and women, infections may not be detected or treated in a timely fashion. This increases the likelihood of disease transmission and the development of complications, such as pelvic inflammatory disease and infertility.3
Increasing the number of people aged 16–25 years being tested for chlamydia infection is a key objective of Australia’s Second national sexually transmissible infections strategy 2010–2013.4 However, several barriers to achieving this increase have been identified, especially among young people with asymptomatic infections. These barriers include costs associated with testing, clinic waiting times, inconvenience, fear of medical procedures, stigma and lack of privacy.5-8 In addition, not all general practitioners in Australia routinely offer chlamydia testing to young people; in particular, men as well as young people in rural settings may be missing out on testing.9
Home-based chlamydia testing has been trialled in several countries as a means of overcoming traditional barriers to testing, with kits advertised and ordered online, or distributed by mail or in the community.10-18 In these models, vaginal and penile swabs or urine samples are taken at home and returned via post. However, uptake has generally been low, limiting the effectiveness of home-based testing. A potential reason for this may be that young people living with their parents, a sexual partner or in shared accommodation are less likely to order or use a chlamydia testing kit at home for fear of arousing suspicion; for example, when receiving an unmarked package in the mail.18
In 2010, the DoHWA established an online chlamydia testing program (OLC) that allows participants to complete a risk self-assessment for chlamydia online and submit a sample for testing at a laboratory without visiting a doctor. The OLC is described in detail in Box 1. Here, we evaluate the OLC from February 2010 to June 2011.
Pathology form download data were obtained from Google Analytics (http://www.google.com/analytics/index.html). All other clinical data were obtained from the dedicated OLC database at the B2 Sexual Health Clinic at Fremantle Hospital (Box 1).
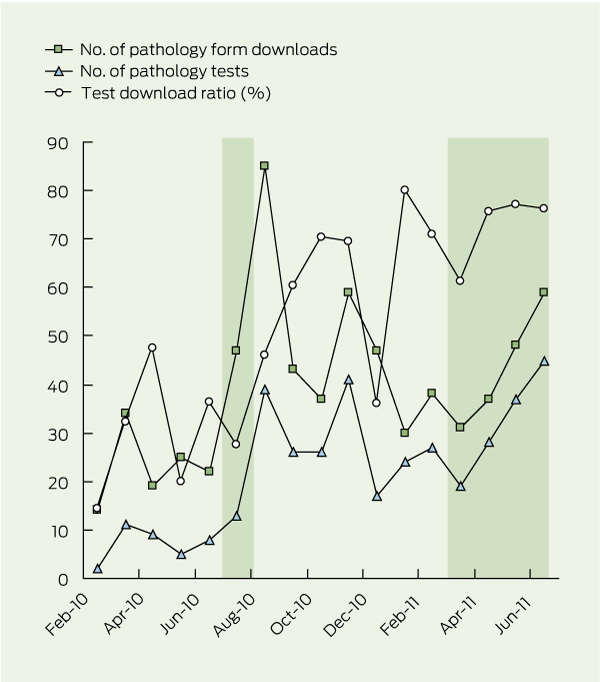
Between February 2010 and June 2011, there were 675 pathology form downloads and 377 pathology tests performed. While the frequency of pathology form downloads tended to increase with time, the effect was not statistically significant (monthly percentage change, 3.5%; 95% CI, −0.8% to 8.0%); however, the number of pathology tests increased significantly (monthly percentage change, 9.5%; 95% CI, 4.3%–14.9%) (Box 2). Fifty-six per cent (n = 377) of downloaded pathology forms resulted in a test, and this proportion increased over time (χ2 test for trend, 67.81; P < 0.001).
Demographic characteristics of the 377 participants tested, who were aged between 16 and 63 years, are shown in Box 3; 71% (n = 267) were aged < 30 years, men outnumbered women, and 37% (n = 141) reported current perceived STI symptoms, the presence of an STI in a sexual contact(s) and/or a past history of an STI. Chlamydia prevalence was 18% (66/377; 95% CI, 14%–21%) overall, and 47% (21/45; 95% CI, 32%–61%) and 68% (27/40; 95% CI, 53%–82%) in participants reporting current perceived STI symptoms and the presence of an STI in sexual contact(s), respectively.
The observed proportions of pathology form downloads resulting in a test (56%) and positive tests (18%) were higher than those reported in many other comparable internet-based testing strategies, in which test return rates ranged from 34% to 62%13,19 and positive test results from 3% to 14%.10,13,15,17,19,20 Our results, coupled with the fact that 71% of OLC participants were < 30 years of age, indicate that this service is being used by young people who are actually at risk of STI, rather than by the “worried well”. They also suggest that the OLC method of internet-based testing may be more appealing to young people, as it eliminates some of the concerns preventing them from accessing traditional STI testing strategies,5-8 and therefore is an effective means of increasing testing rates among this cohort.
Another strength of the OLC is its potential to reach traditionally difficult-to-access populations for chlamydia testing and sexual health education. In Australia, only 1.6% and 6.3% of 15–24-year-old men and women, respectively, are opportunistically tested for chlamydia by their GP.9 The relative overrepresentation of males among OLC participants suggests that this method of accessing testing is acceptable to young men. The requirement to complete an online risk self-assessment before accessing the test request form also provides an opportunity for participants, especially those who are less likely to access health care (such as young men), to learn about, or be reminded of, behaviours and symptoms associated with chlamydia and other STIs.
Completeness of clinical management for all participants with positive test results indicates that participants were serious about getting tested and willing to provide their correct contact details on an online pathology form. The median time from specimen collection to treatment of 7 days was comparable with the range of 5–7 days reported from Australian and overseas sexual health clinics.21,22
The internet is an important source of sexual health information among young people in Australia,23 and 45% of OLC participants found out about the program through an internet search. Internet-based chlamydia screening strategies are competitively cost-effective in comparison with traditional clinic-based screening approaches.24 However, a cost-effectiveness analysis was outside the scope of our study.
1 Online chlamydia testing program (OLC) of the Western Australia Department of Health (DoHWA)
2 Online chlamydia testing program (OLC) — number of downloads of test request forms and pathology tests performed, and proportion of downloaded forms resulting in a test, by month, February 2010 to June 2011*
Received 28 November 2011, accepted 10 April 2012
- Kellie S H Kwan1
- Edwina A Jachimowicz2
- Lisa Bastian1
- Lewis Marshall2
- Donna B Mak1
- 1 Communicable Disease Control Directorate, Department of Health, Western Australia, Perth, WA.
- 2 Fremantle Hospital, Perth, WA.
We thank Melanie Lau for undertaking the Poisson regression component of data analysis.
No relevant disclosures.
- 1. The Kirby Institute. HIV/AIDS, viral hepatitis and sexually transmissible infections in Australia annual surveillance report 2011. Sydney: The Kirby Institute, The University of New South Wales, 2011. http://www.med.unsw.edu.au/NCHECRweb.nsf/resources/2011/$file/KIRBY_ASR2011.pdf (accessed Nov 2011).
- 2. Government of Western Australia Department of Health. The epidemiology of notifiable sexually transmitted infections and blood-borne viruses in Western Australia 2010. Perth: DoH, WA, 2011. http://www.public.health.wa.gov.au/cproot/4221/2/2010_Annual_STI_BBV_Report.pdf (accessed Nov 2011).
- 3. Workowski KA, Berman S; Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep 2010; 59: 1-110.
- 4. Australian Government Department of Health and Ageing. Second national sexually transmissible infections strategy 2010–2013. Canberra: DoHA, 2010. http://www.health.gov. au/internet/main/publishing.nsf/Content/ohp-national-strategies-2010-sti/$File/sti.pdf (accessed Sep 2011).
- 5. Tilson EC, Sanchez V, Ford CL, et al. Barriers to asymptomatic screening and other STD services for adolescents and young adults: focus group discussions. BMC Public Health 2004; 4: 21.
- 6. Pavlin NL, Gunn JM, Parker R, et al. Implementing chlamydia screening: what do women think? A systematic review of the literature. BMC Public Health 2006; 6: 221.
- 7. Rose SB, Smith MC, Lawton BA. “If everyone does it, it’s not a big deal.” Young people talk about chlamydia testing. N Z Med J 2008; 121: 33-42.
- 8. Balfe M, Brugha R. What prompts young adults in Ireland to attend health services for STI testing? BMC Public Health 2009; 9: 311.
- 9. Kong FYS, Guy R, Boyle DJ, et al. Chlamydia testing rates in general practices across Australia: the Australian Collaboration for Chlamydia Enhanced Sentinel Surveillance (ACCESS). Australasian Sexual Health Conference; 2008 Sep 15-17; Perth, Australia. https://secure.ashm.org.au/ei/viewpdf.esp?id=37&file=c%3A%5CCertain%5CEventwin%5Cdocs% 5Cpdf%5Cashm08Abstract00382%2Epdf (accessed Sep 2011).
- 10. Ford CA, Viadro CI, Miller WC. Testing for chlamydial and gonorrhoeal infections outside of clinic settings: a summary of the literature. Sex Transm Dis 2004; 31: 38-51.
- 11. Tebb KP, Paukku MH, Pai-Dhungat MR, et al. Home STI testing: the adolescent female’s opinion. J Adolesc Health 2004; 35: 462-467.
- 12. van Bergen JE, Postma MJ, Peerbooms PG, et al. Effectiveness and cost-effectiveness of a pharmacy-based screening programme for Chlamydia trachomatis in a high-risk health centre population in Amsterdam using mailed home-collected urine samples. Int J STD AIDS 2004; 15: 797-802.
- 13. Novak DP, Karlsoon RB. Simplifying chlamydia testing: an innovative Chlamydia trachomatis testing approach using the internet and a home sampling strategy: population based study. Sex Transm Infect 2006; 82: 142-147.
- 14. Jones HE, Altini L, de Kock A, et al. Home-based versus clinic-based self-sampling and testing for sexually transmitted infections in Gugulethu, South Africa: randomised controlled trial. Sex Transm Infect 2007; 83: 552-557.
- 15. Lippman SA, Jones HE, Luppi CG, et al. Home-based self-sampling and self-testing for sexually transmitted infections: acceptable and feasible alternatives to provider-based screening in low-income women in São Paulo, Brazil. Sex Transm Dis 2007; 34: 421-428.
- 16. Marrazzo JM, Scholes D. Acceptability of urine-based screening for Chlamydia trachomatis in asymptomatic young men: a systematic review. Sex Transm Dis 2008; 35 (11 Suppl): S28-S33.
- 17. Buhrer-Skinner M, Muller R, Bialasiewicz S, et al. The check is in the mail: piloting a novel approach to Chlamydia trachomatis testing using self-collected, mailed specimen. Sex Health 2009; 6: 163-169.
- 18. Sacks-Davis R, Gold J, Aitken CK, Hellard ME. Home-based testing of young people attending a music festival — who will pee and post? BMC Public Health 2010; 10: 376.
- 19. Gaydos CA, Dwyer, K, Barnes M, et al. Internet-based screening for Chlamydia trachomatis to reach non-clinic populations with mailed self-administered vaginal swabs. Sex Transm Dis 2006; 33: 451-457.
- 20. Martin L, Freedman E, Burton L, et al. The C-project: use of self-collection kits to screen for Chlamydia trachomatis in young people in a community-based health promotion project. Sex Health 2009; 6: 157-162.
- 21. Malik AI, Huppert JS. Interval to treatment of sexually transmitted infections in adolescent females. J Pediatr Adolesc Gynecol 2007; 20: 275-279.
- 22. Welch J. Follow-up of clients with chlamydia at Clinic 275 in 2001. Adelaide: Royal Adelaide Hospital, 2009. http://www.stdservices.on.net/stats/qsr200203/Follow%20up%20of%20 clinic%20clients%20with%20chlamydia.htm (accessed Nov 2011).
- 23. Smith A, Agius P, Mitchell A, et al. Secondary students and sexual health 2008. Monograph Series No. 70. Melbourne: Australian Research Centre in Sex, Health & Society, La Trobe University, 2009. http://www.latrobe.edu.au/arcshs/downloads/arcshs-research-publications/secondary-students-and-sexual-health-2008.pdf (accessed Oct 2011).
- 24. Huang W, Gaydos CA, Barnes MR, et al. Cost-effectiveness analysis of Chlamydia trachomatis screening via internet-based self-collected swabs compared with clinic-based sample collection. Sex Transm Dis 2011; 38: 815-820.





Abstract
Objective: To evaluate data from an online chlamydia testing program (OLC) developed to increase young people’s access to testing for chlamydia, the most commonly notified disease in Australia and Western Australia, with a high proportion of notifications among young people (< 30 years).
Design and setting: The OLC was launched in February 2010, and our study covers the period February 2010 to June 2011. Without needing to first visit a doctor, OLC participants receive risk self-assessment, education, testing, and, if necessary, referral for treatment, and can complete an online satisfaction survey.
Main outcome measures: Number and proportion of downloaded pathology forms that resulted in a test; demographic characteristics of participants; prevalence of chlamydia; completeness and timeliness of follow-up of positive test results; and participant satisfaction.
Results: More than half (56%) of the 675 OLC pathology form downloads resulted in a test, and chlamydia was detected in 18% (66/377). Of those tested, over half were men (55%), and 71% were aged < 30 years. All participants with a positive test result received appropriate clinical management, with 50% being treated within 7 days of specimen collection. Of the 17% (55/332) who completed an online satisfaction survey, almost all said they would recommend the service to a friend.
Conclusion: Internet-based screening for chlamydia is an effective means of increasing access to testing for young people at risk of sexually transmitted infections and is a valuable addition to opportunistic, clinic-based strategies.