The concept of triage can be used to allocate medical resources in mass casualty events, such as a natural disaster, where the volume of patients presenting for medical attention exceeds the capacity to provide effective health care.1,2 Ethical issues surrounding the use of triage to prioritise patient management are challenging.1-3 Triage systems to allocate critical care resources have not yet been used in an influenza pandemic.
The outbreak of pandemic (H1N1) 2009 influenza required the provision of critical care services to large numbers of patients in Australia and New Zealand.4 In New South Wales, there were 519 intensive care unit (ICU) beds available to service a population of 7.2 million people.5,6 Equipment stockpiles could increase statewide ventilation capacity in a pandemic, but only by an additional 70%.5
Towards the end of the pandemic, in July 2009, the NSW Department of Health instituted a triage protocol to manage ICU resources during an influenza crisis when the surge in demand exceeded capacity by 50% (Box 1).5 The NSW triage protocol predominantly used criteria from a Minnesota protocol and added an element from a Canadian protocol, the Ontario Health Plan for an Influenza Pandemic (OHPIP, Box 2).7,8
As the NSW triage protocol was instituted as a mandatory policy directive,5 our primary objective was to determine the increase in ICU bed availability that would result from its use. Our second objective was to compare this increase in bed availability with that from use of the OHPIP triage protocol.
The triage protocols are described in Box 1 and Box 2. In brief, the NSW triage protocol had three tiers, which could be activated in a stepwise, time-based fashion as demand for critical care services increased. Tier 1 excluded patients from ICU admission if they had significant multiple organ failure, and discharged patients after 12 or 72 hours if they failed to respond to treatment. Tier 2 excluded patients with clinical conditions perceived to be associated with a poor prognosis, in addition to patients already excluded by Tier 1. Tier 3 was designed to expand on Tier 2’s list of clinical exclusion criteria, but at the time of the policy’s introduction, only the Sequential Organ Failure Assessment (SOFA) scoring system from the OHPIP triage protocol had been incorporated.8,9
The OHPIP triage protocol had one tier and differed from the NSW protocol in its patient selection criteria. It only admitted patients who required mechanical ventilation or haemodynamic support, on the basis that these forms of support fundamentally differentiate ICUs from other acute care areas. It excluded patients on the basis of advanced age and the requirement for resources that could not realistically be provided in a pandemic (eg, care for severe burns). Patients were also excluded at admission or discharged after 48 hours or 120 hours using criteria based on their SOFA score.8,9
At ICU admission, data were collected on patients’ age, sex, APACHE II (Acute Physiology and Chronic Health Evaluation) score (higher scores indicate greater severity of illness),10 and diagnosis (as defined by the Australian and New Zealand Intensive Care Society Centre for Outcome and Resource Evaluation Adult Patient Database).11 Patients were followed up to discharge from or death in the ICU.
There were 135 beds available for use in the eight ICUs during the study period (mean, 16.9 ± 5.2 beds per day per ICU). Demographic data of the patients are shown in Box 3. Patients had a mean length of stay in the ICU of 5.4 ± 7.8 days and occupied 4350 bed-days (76.7% of 5670 total available bed-days). The overall ICU mortality rate was 11.7% (94 deaths).
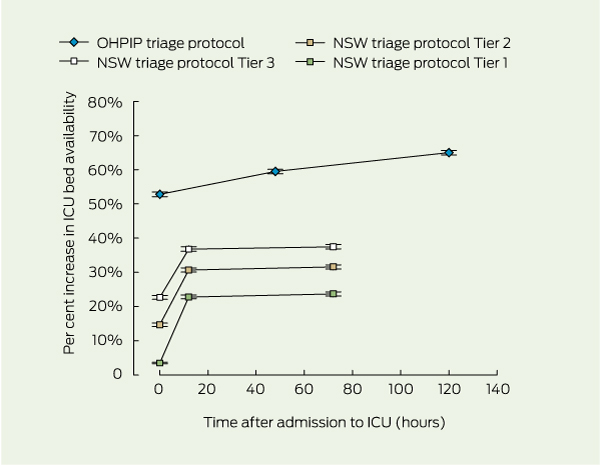
Box 4 shows the cumulative increase in ICU bed availability resulting from evaluating patients using each tier of the NSW triage protocol at admission, 12 hours and 72 hours, and using the OHPIP protocol at admission, 48 hours and 120 hours. There were significant differences in the increase in ICU bed availability at admission between all tiers of the NSW triage protocol and the OHPIP protocol (P < 0.001).
Using the NSW triage protocol, all three tiers provided significant increases in ICU bed availability when patients were re-evaluated at 12 hours, but the maximal cumulative increase in ICU bed availability occurred with Tier 3. The OHPIP triage protocol provided the greatest increase in ICU bed availability overall, with a cumulative increase greater than any tier in the NSW triage protocol. Our results for the OHPIP protocol are similar to those from a retrospective study of two ICUs, which demonstrated that total ICU days would decrease by 52.6% with use of the protocol.12
The justification for excluding patients with high predicted mortality rates from ICU care in a triage protocol is that they are less likely to survive, and therefore less likely to have outcomes improved by ICU care. However, selective application of triage criteria may be considered ethically unjust if patients with similar ICU mortality rates are treated differently.1 It is therefore important that mortality rates for patients excluded by triage protocols are accurately determined.
Future studies should evaluate influenza pandemic triage protocols in real pandemic situations and determine whether they can be improved. Complex computerised simulation may represent an alternative, although less rigorous, evaluation method.13 Future studies should evaluate these protocols in different medical jurisdictions. Research also needs to determine whether such restrictive measures are acceptable to the communities in which they will be used in a public health crisis.
1 New South Wales influenza pandemic triage protocol*
Do not offer AND withdraw life-sustaining therapy from patients with any of the following:
3. Laboratory or clinical evidence of ≥ 4 organ systems failing:
a. Pulmonary (acute respiratory distress syndrome, ventilatory failure, refractive hypoxia)
b. Cardiovascular (left ventricular failure, hypotension, new ischaemia)
c. Renal (hyperkalaemia, oliguria despite fluid resuscitation, increasing creatinine level)
d. Hepatic (transaminase > 2 times normal upper limit, increased bilirubin or ammonia levels)
f. Haematological (clinical or laboratory evidence of disseminated intravascular coagulation)
g. Cirrhosis with ascites, history of variceal bleeding, fixed coagulopathy, or encephalopathy†
2. Acute renal failure requiring haemodialysis
3. Severe chronic lung disease requiring home oxygen therapy†
5. Active malignancy with poor potential for survival
6. Acute hepatic failure with hyperammonaemia
Specific triage protocols developed centrally and advised by specialist clinical groups:
2. Expansion of pre-existing disease classes that will not be offered ventilatory support
3. Applying SOFA scoring to the triage process, establishing a cut-off score‡
SOFA = Sequential Organ Failure Assessment. * Reproduced with permission.5,7 The triage protocol applies to all patients undergoing assessment for possible critical care and not only those with influenza-like symptoms. Tier 1 is used initially; Tiers 2 and 3 can be sequentially activated later, as demand for intensive care unit resources escalates. † Denotes criteria in the NSW triage protocol5 that were modified from the original triage criteria.7 ‡ Refers to the prioritisation tool in the Ontario Health Plan for an Influenza Pandemic triage protocol (see Box 2).
2 Ontario Health Plan for an Influenza Pandemic triage protocol*
Received 19 July 2011, accepted 17 February 2012
- Winston K Cheung1,2
- John Myburgh3,4
- Ian M Seppelt5,2
- Michael J Parr6,3
- Nikki Blackwell7,8
- Shannon DeMonte7
- Kalpesh Gandhi9
- Larissa Hoyling5
- Priya Nair10
- Melissa Passer11,12
- Claire Reynolds10
- Nicholas M Saunders12,13
- Manoj K Saxena14,4
- Govindasamy Thanakrishnan1
- on behalf of the Influenza Pandemic ICU Triage (iPIT) Study Investigators
- 1 Concord Repatriation General Hospital, Sydney, NSW.
- 2 University of Sydney, Sydney, NSW.
- 3 University of New South Wales, Sydney, NSW.
- 4 The George Institute for Global Health, Sydney, NSW.
- 5 Nepean Hospital, Sydney, NSW.
- 6 Liverpool Hospital, Sydney, NSW.
- 7 Prince Charles Hospital, Brisbane, QLD.
- 8 University of Queensland, Brisbane, QLD.
- 9 Blacktown Hospital, Sydney, NSW.
- 10 St Vincent’s Hospital, Sydney, NSW.
- 11 Ramsay Health Care, Sydney, NSW.
- 12 Royal North Shore Hospital, Sydney, NSW.
- 13 Norfolk and Norwich University Hospital NHS Foundation Trust, Norwich, UK.
- 14 St George Hospital, Sydney, NSW.
We thank Jennifer Peat, Concord Repatriation General Hospital, for her help with the statistical analysis, and the George Institute NSW ICU Research Group. We are indebted to the other investigators and participating hospitals — Blacktown Hospital: Dhaval Ghelani, Kiran Nand, Treena Sara; Concord Repatriation General Hospital: Helen Wong; Liverpool Hospital: Sharon Micallef; Prince Charles Hospital: Daniel Mullany; Royal North Shore Hospital: Simon Bird, Jane Bowey, Anthony Delaney; St George Hospital: Deborah Inskip, Rebecca Sidoli; Nepean Hospital and St Vincent’s Hospital — and the dedicated medical and nursing staff at all the hospitals for their help with this study. This study was funded solely by the participating ICUs.
No relevant disclosures.
- 1. Sztajnkrycer MD, Madsen BE, Báez AA. Unstable ethical plateaus and disaster triage. Emerg Med Clin North Am 2006; 24: 749-768.
- 2. White DB, Katz MH, Luce JM, Lo B. Who should receive life support during a public health emergency? Using ethical principles to improve allocation decisions. Ann Intern Med 2009; 150: 132-138.
- 3. Kaposy C. Accounting for vulnerability to illness and social disadvantage in pandemic critical care triage. J Clin Ethics 2010; 21: 23-29.
- 4. ANZIC Influenza Investigators. Critical care services and 2009 H1N1 influenza in Australia and New Zealand. N Engl J Med 2009; 361: 1925-1934.
- 5. NSW Health. Influenza pandemic – providing critical care. Policy Directive PD2010_028. Sydney: NSW Health, 2010. http://www.health.nsw.gov.au/policies/pd/2010/PD2010_028.html (accessed Nov 2010).
- 6. Australian Bureau of Statistics. Australian demographic statistics, Mar 2011. Canberra: ABS, 2011. (ABS Cat. No. 3101.0.) http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3101.0Mar%202011?OpenDocument (accessed Feb 2012).
- 7. Hick JL, O’Laughlin DT. Concept of operations for triage of mechanical ventilation in an epidemic. Acad Emerg Med 2006; 13: 223-229.
- 8. Christian MD, Hawryluck L, Wax RS, et al. Development of a triage protocol for critical care during an influenza pandemic. CMAJ 2006; 175: 1377-1381.
- 9. Vincent JL, Moreno R, Takala J, et al; Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med 1996; 22: 707-710.
- 10. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med 1985; 13: 818-829.
- 11. Australian and New Zealand Intensive Care Society Centre for Outcome and Resource Evaluation (CORE). CORE data collection tools. http://www.anzics.com.au/core/data-collection-tools (accessed Mar 2011).
- 12. Christian MD, Hamielec C, Lazar NM, et al. A retrospective cohort pilot study to evaluate a triage tool for use in a pandemic. Crit Care 2009; 13: R170. doi: 10.1186/cc8146.
- 13. Burton A, Altman DG, Royston P, Holder RL. The design of simulation studies in medical statistics. Stat Med 2006; 25: 4279-4292. doi: 10.1002/sim.2673.





Abstract
Objective: To determine the increase in intensive care unit (ICU) bed availability that would result from the use of the New South Wales and Ontario Health Plan for an Influenza Pandemic (OHPIP) triage protocols.
Design, setting and patients: Prospective evaluation study conducted in eight Australian, adult, general ICUs, between September 2009 and May 2010. All patients who were admitted to the ICU, excluding those who had elective surgery, were prospectively evaluated using the two triage protocols, simulating a pandemic situation. Both protocols were originally developed to determine which patients should be excluded from accessing ICU resources during an influenza pandemic.
Main outcome measure: Increase in ICU bed availability.
Results: At admission, the increases in ICU bed availability using Tiers 1, 2 and 3 of the NSW triage protocol were 3.5%, 14.7% and 22.7%, respectively, and 52.8% using the OHPIP triage protocol (P < 0.001). Re-evaluation of patients at 12 hours after admission using Tiers 1, 2 and 3 of the NSW triage protocol incrementally increased ICU bed availability by 19.2%, 16.1% and 14.1%, respectively (P < 0.001). The maximal cumulative increases in ICU bed availability using Tiers 1, 2 and 3 of the NSW triage protocol were 23.7%, 31.6% and 37.5%, respectively, at 72 hours (P < 0.001), and 65.0% using the OHPIP triage protocol, at 120 hours (P < 0.001).
Conclusion: Both triage protocols resulted in increases in ICU bed availability, but the OHPIP protocol provided the greatest increase overall. With the NSW triage protocol, ICU bed availability increased as the protocol was escalated.