Although it is widely accepted that good handover is important for patient safety, there is only limited evidence that improved handover can lead to reduced patient risk.1,2
Written handover transmits information more reliably than informal communication, especially in conjunction with a verbal component.3 Before this initiative, written weekend handover in general medicine at Barwon Health was variable in content and non-standardised, and information was located in a variety of places. Such non-standardised handovers usually only comprised clinical summaries. We felt this was both a risk to our patients and inefficient for the organisation. It was difficult to ensure that key clinical messages were transmitted across multiple shifts of covering doctors. There was constant pressure for patients to be discharged on weekends, and this was difficult to organise unless instructions could be conveyed to the doctors covering the weekend shifts.
We sought to improve our doctor-to-doctor weekend shift handovers through a system where handover components could be entered electronically. We were aware of other systems such as SBAR (situation–background–assessment–recommendation), ISBAR (identify–situation–background–assessment–request) and ISoBAR (identify–situation–observations–background–agreed plan–read back), but felt these were better for direct person-to-person communication of time-critical information requiring immediate action or escalation.4-6 We required a system of communicating written information to multiple staff members, for actioning in the future (over multiple shifts) in a non-urgent and ongoing manner. None of these existing communication systems contained all of the components we required,4,5,7,8 so we set out to develop our own.
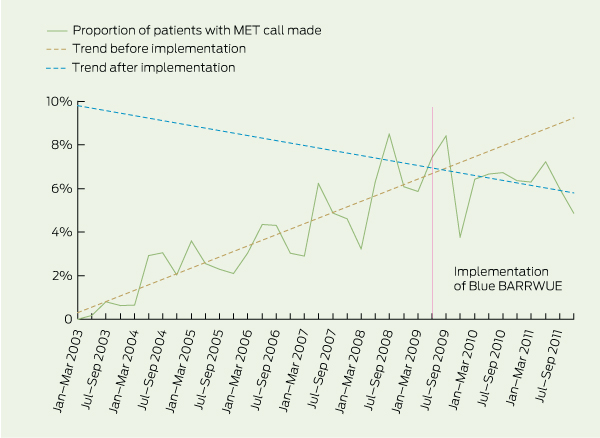
Barwon Health is committed to patient safety. A medical emergency team (MET) system was introduced in 2003 to identify patients with a deteriorating condition using standard criteria, and to prevent adverse events.9-11 Since 2007, the MET call rate has been stabilising at about 60 calls per 1000 admissions across Barwon Health, which is consistent with the rate of emergency calls expected in a mature established system,12-15 although the number of MET calls in general medicine had been increasing up to the time of this study. The intensive care registrar enters the details of all MET calls into SLIC, a locally developed comprehensive clinical information and data collection system for the intensive care unit.
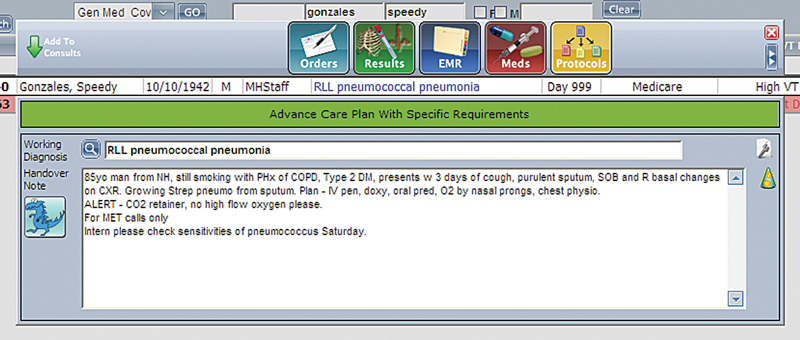
In April 2009, we held a brainstorming session with around 15 general medical interns, registrars and a physician. The session was focused on the components and order of the handover as well as a discussion on why doctors handed over certain patients and what messages they were trying to convey. The components of the handover were placed in an order that corresponded to the way that the handover was structured by experienced doctors at our institution. The acronym “Blue BARRWUE” was created from the initials of the components and a mascot was developed. Reminders about handover were put in place, including automatic paging on Fridays at 12 pm. Combined lists of inpatients belonging to all five general medical units (shared views) were developed to be printed by covering doctors at the beginning of their shift. Teams were encouraged to update their handovers daily as a shared responsibility between intern and registrar (Box 1). This task took about 5–10 minutes at the end of each day. Particular emphasis was placed on Friday handovers to ensure that plans were in place for the weekend for covering doctors to act on. Electronic reports were developed to monitor completion rates. Posters about the new handover system were displayed on the medical wards. New doctors received training in using the system alongside ISBAR. In addition, nurses on the medical wards began printing and reading the handovers to help them plan for weekends.
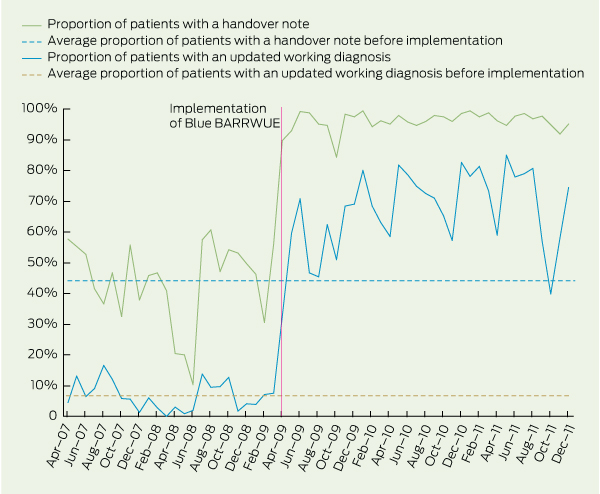
In the 12 months before implementation, 976 patients (47.98%) had a handover note in BOSSnet, versus 1646 patients (95.09%) in the 12 months after implementation (P < 0.001; rate ratio [RR], 20.75 for presence of a handover note after implementation; 95% CI, 16.33–26.44; Box 2).
In the 12 months before implementation, 167 patients (8.21%) had an updated working diagnosis in BOSSnet, versus 1000 patients (57.77%) in the 12 months after implementation (P < 0.001; RR, 15.29 for the presence of an updated working diagnosis after implementation; 95% CI, 12.66–18.48; Box 2).
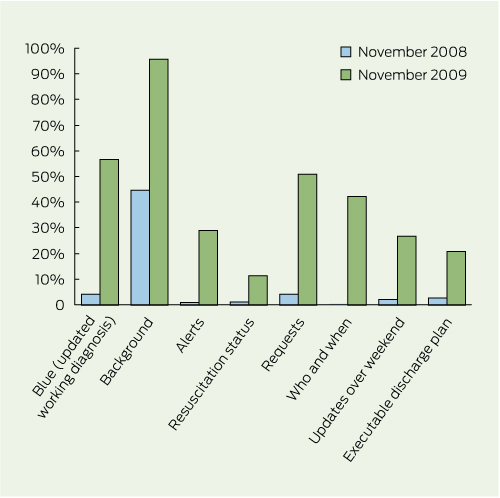
The presence of all components of the handover in November 2009 (6 months after implementation) increased in comparison with that in November 2008 (P < 0.001 for all components; Box 3).
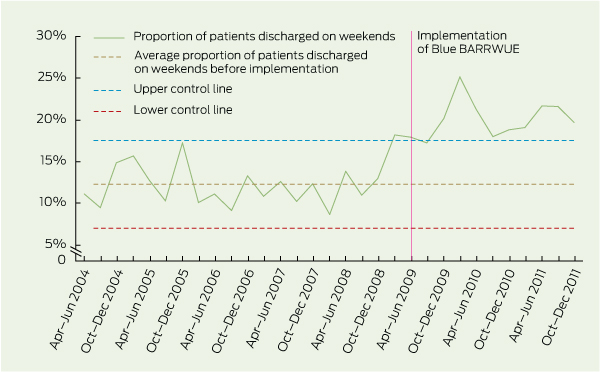
In the 12 months before implementation, 289 patients (14.21%) were discharged over weekends, versus 353 (20.39%) in the 12 months after implementation (P < 0.001; RR, 1.44 for weekend discharge after implementation; 95% CI, 1.25–1.65; Box 4).
There were 152 general medical patients for whom MET calls were made in the 12 months before implementation, (7.47%), versus 95 general medical patients (5.49%) for whom MET calls were made in the 12 months after implementation (P = 0.01; RR, 0.73 for MET calls after implementation; 95% CI, 0.57–0.94; Box 5).
Our brainstorming session led to a standardised but flexible format for written handover that was practical and easy to use and resulted in immediate and sustained uptake. Involving clinicians in the development of handover systems has been reported to be useful and certainly allowed us to identify components that we otherwise would have missed.16 As a result, the components of the handover have been remarkably stable — we have not identified any new components that we need to include nor found that any of the existing ones are not relevant — since the implementation of the Blue BARRWUE system.
We believe that the new handover system has had a high sustained uptake as a result of clinical championing by the Head of General Medicine and because of the high value it provides to junior doctors in their daily work.17 The handover is quick and easy to enter into the system, it is flexible and highly visible, and junior doctors use it as an aide-mémoire on their daily rounds and when referring patients, writing discharge summaries and covering difficult shifts. Junior doctors have said that covering without it is like “flying blind”.
1 Computer screen image showing the interface for entering the handover information in the BOSSnet clinical handover system (mock patient data)
2 Proportion of general medical inpatients with a handover note and an updated working diagnosis, and average proportions before implementation of the Blue BARRWUE electronic handover system*
3 Proportion of handover components present in the BOSSnet clinical handover system at 7 pm on Friday evenings in November 2008 and November 2009
4 Proportion of general medical inpatients discharged on weekends from Geelong Hospital before and after implementation of the Blue BARRWUE electronic handover system
Received 12 August 2011, accepted 26 July 2012
- Boloor S Rao1
- Gail O Lowe2
- Andrew J Hughes2
- 1 General Medicine, Flinders Medical Centre, Adelaide, SA.
- 2 Barwon Health, Geelong, VIC.
We would like to thank all the medical registrars and interns who helped create and have used the Blue BARRWUE handover system, Margaret Henry and Deb Friedman for statistical assistance and Ross Arblaster for creating the queries and reports for data analysis.
No relevant disclosures.
- 1. Van Eaton EG, Horvath KD, Lober WB, et al. A randomized, controlled trial evaluating the impact of a computerized rounding and sign-out system on continuity of care and resident work hours. J Am Coll Surg 2005; 200: 538-545.
- 2. Petersen LA, Orav EJ, Teich JM, et al. Using a computerized sign-out program to improve continuity of inpatient care and prevent adverse events. Jt Comm J Qual Improv 1998; 24: 77-87.
- 3. Bhabra G, Mackeith S, Monteiro P, Pothier DD. An experimental comparison of handover methods. Ann R Coll Surg Engl 2007; 89: 298-300.
- 4. Porteous JM, Stewart-Wynne EG, Connolly M, Crommelin PF. iSoBAR — a concept and handover checklist: the National Clinical Handover Initiative. Med J Aust 2009; 190 (11 Suppl): S152-S156.
- 5. Haig KM, Sutton S, Whittington J. SBAR: a shared mental model for improving communication between clinicians. Jt Comm J Qual Patient Saf 2006; 32: 167-175.
- 6. Finnigan MA, Marshall SD, Flanagan BT. ISBAR for clear communication: one hospital’s experience spreading the message. Aust Health Rev 2010; 34: 400-404.
- 7. Marshall S, Harrison J, Flanagan B. The teaching of a structured tool improves the clarity and content of interprofessional clinical communication. Qual Saf Health Care 2009; 18: 137-140.
- 8. Cheah LP, Amott DH, Pollard J, Watters DA. Electronic medical handover: towards safer medical care. Med J Aust 2005; 183: 369-372. <MJA full text>
- 9. Hodgetts TJ, Kenward G, Vlachonikolis IG, et al. The identification of risk factors for cardiac arrest and formulation of activation criteria to alert a medical emergency team. Resuscitation 2002; 54: 125-131.
- 10. Buist M, Bernard S, Nguyen TV, et al. Association between clinically abnormal observations and subsequent in-hospital mortality: a prospective study. Resuscitation 2004; 62: 137-141.
- 11. Cretikos M, Chen J, Hillman K, et al; MERIT study investigators. The objective medical emergency team activation criteria: a case-control study. Resuscitation 2007; 73: 62-72.
- 12. Jones D, George C, Hart GK, et al. Introduction of medical emergency teams in Australia and New Zealand: a multi-centre study. Crit Care 2008; 12: R46.
- 13. Chen J, Bellomo R, Flabouris A, et al. The relationship between early emergency team calls and serious adverse events. Crit Care Med 2009; 37: 148-153.
- 14. DeVita MA, Braithwaite RS, Mahidhara R, et al; Medical Emergency Response Improvement Team. Use of medical emergency team responses to reduce hospital cardiopulmonary arrests. Qual Saf Health Care 2004; 13: 251-254.
- 15. Jones D, Bellomo R, DeVita MA. Effectiveness of the Medical Emergency Team: the importance of dose. Crit Care 2009; 13: 313.
- 16. Wong MC, Turner P, Yee KC. Involving clinicians in the development of an electronic clinical handover system — thinking systems not just technology. Stud Health Technol Inform 2008; 136: 490-495.
- 17. Soo S, Berta W, Baker GR. Role of champions in the implementation of patient safety practice change. Healthc Q 2009; 12 Spec No Patient: 123-128.





Abstract
Objectives: To measure the frequency and content of electronic handover before and after implementation of the Blue BARRWUE handover system, and to measure its effect on patient safety and hospital efficiency over weekends.
Design, setting and participants: Point-prevalence study comparing outcomes for general medical inpatients present over weekends before implementation (1 May 2008 to 30 April 2009) and after implementation (1 May 2009 to 30 April 2010) of the Blue BARRWUE handover system at Geelong Hospital.
Intervention: Implementation of the Blue BARRWUE handover system and its components (updated working diagnosis, background, alerts, resuscitation status, requests, who to do what and when, updates and executable discharge plan).
Main outcome measures: Presence of any written handover notes or updated working diagnoses in the BOSSnet clinical information system, content of handover notes, frequency of weekend discharges and medical emergency team (MET) calls before and after implementation.
Results: In the 12 months before implementation of the Blue BARRWUE handover system, 976 patients (47.98%) had a handover note in BOSSnet, versus 1646 patients (95.09%) in the 12 months after implementation (P < 0.001; rate ratio [RR], 20.75; 95% CI, 16.33–26.44). Before implementation, 289 patients (14.21%) were discharged over weekends, versus 353 patients (20.39%) after implementation, (P < 0.001; RR, 1.44; 95% CI, 1.25–1.65). MET calls were made for 152 general medical patients before implementation (7.47%), versus 95 general medical patients (5.49%) after implementation (P = 0.01; RR, 0.73; 95% CI, 0.57–0.94).
Conclusions: The Blue BARRWUE system has sustainably improved written handover in our organisation and was associated with improvement in both patient safety and hospital efficiency.