To the Editor: Rates of health care-associated Staphylococcus aureus bacteraemia (HCA-SAB) and hand hygiene (HH) compliance are now subject to public disclosure on the MyHospitals website (http://www.myhospitals.gov.au). HH compliance and HH alcohol hand rub and liquid soap procurement have been associated with reduced methicillin-resistant (but not methicillin-sensitive) S. aureus bacteraemias, generally in the presence of other co-interventions.1,2 However, the National Hand Hygiene Initiative advocates that all HCA-SAB (with both methicillin-resistant and methicillin-sensitive organisms) be interpreted as a key indicator of HH compliance.
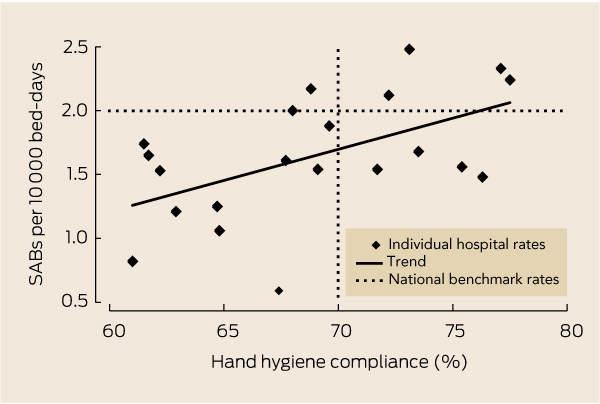
HH compliance and HCA-SAB rates were counterintuitively positively correlated (r = 0.54; Box), with hospitals with greater HH compliance showing higher HCA-SAB rates. For every 10 percentage point increase in HH compliance, the HCA-SAB rate increased by 0.5 cases per 10 000 bed-days (95% CI, 0.1–0.9; P = 0.01). Of the five hospitals with HCA-SAB rates above the national benchmark (2.0 cases per 10 000 bed-days), four also had HH compliance rates above the national benchmark (70%); of the 16 hospitals with lower HCA-SAB rates, 12 had lower HH compliance rates.
This counterintuitive relationship highlights the erroneous use of HCA-SAB as an indicator of the impact of HH compliance, as there are multiple other important causes of HCA-SAB.3 In the absence of a reliable indicator, HH should instead be evaluated simply by compliance. Even if there was a direct causal relationship between HH and HCA-SAB, contemporaneous (rather than the presently available non-contemporaneous) data should be disclosed, particularly where these data encourage judgements about the performance of hospitals.
While HH is clearly important, it is only one of multiple interventions (including intravascular device management4) required to reduce HCA-SAB.5 This may explain why many hospitals are achieving low HCA-SAB rates despite low HH compliance. It is therefore vital that complex multimodal infection control strategies to prevent HCA-SAB and other infections not be simplistically summarised by HH compliance alone. With the media scrutiny of hospitals with HH compliance below the benchmark, it would be unfortunate if hospitals focused only on HH at the expense of other strategies, simply to achieve the HH benchmark and avert negative publicity.
- 1. Grayson ML, Russo PL, Cruickshank M, et al. Outcomes from the first 2 years of the Australian National Hand Hygiene Initiative. Med J Aust 2011; 195: 615-619. <MJA full text>
- 2. Stone SP, Fuller C, Savage J, et al. Evaluation of the national Cleanyourhands campaign to reduce Staphylococcus aureus bacteraemia and Clostridium difficile infection in hospitals in England and Wales by improving hand hygiene: four year, prospective, ecological, interrupted time series study. BMJ 2012; 344: e3005.
- 3. Naber CK. Staphylococcus aureus bacteraemia: epidemiology, pathophysiology, and management strategies. Clin Infect Dis 2009; 48 Suppl 4: 231-237.
- 4. O’Grady NP, Alexander M, Burns LA, et al. Guidelines for the prevention of intravascular catheter-related infections. Atlanta, Ga: Centers for Disease Control and Prevention, 2011. http://www.cdc.gov/hicpac/BSI/BSI-guidelines-2011.html (accessed Jun 2012).
- 5. Kok J, O’Sullivan MV, Gilbert GL. Feedback to clinicians on preventable factors can reduce hospital onset Staphylococcus aureus bacteraemia rates. J Hospital Infect 2011; 79: 108-114.





No relevant disclosures.