Clare’s story
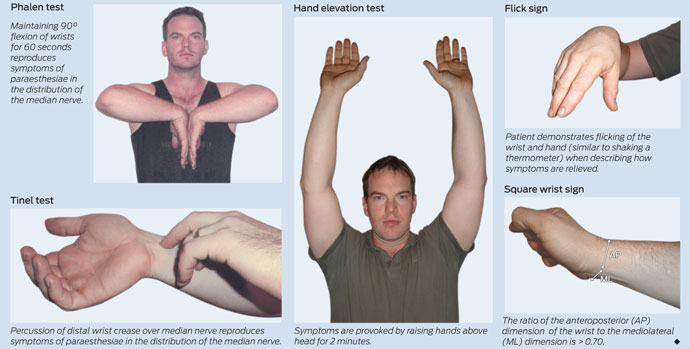
On examination, Clare’s hands appeared normal, with no evidence of muscle wasting and no weakness or incoordination. Sensory examination showed a subjective reduction of sensation in the index and middle fingers and thumb of the right hand. Reflexes were present and symmetrical. Prolonged wrist flexion (Phalen test; Box 1) reproduced symptoms of bilateral hand pain and paraesthesiae, but percussion of the median nerves at the wrist (Tinel test; Box 1) did not. The remainder of the neurological examination was normal.
Clinical tests: Several clinical tests, which vary in their diagnostic utility,1 can be used in the diagnosis of carpal tunnel syndrome (Box 1). There is wide variation in the reported sensitivity and specificity of these tests: the Phalen test, for example, one of the most commonly used, has a reported sensitivity of 10%–91% and specificity of 33%–86%.1 In general, the Phalen and Tinel tests are the most widely used and are both more specific than sensitive.
Neurophysiological investigations: Although an accurate diagnosis of carpal tunnel syndrome can be made clinically in many cases, nerve conduction studies are essential for confirming the diagnosis and assessing severity.2 A baseline study before operative intervention can also assist with documenting a successful carpal tunnel release.
Many neurophysiology laboratories grade severity of carpal tunnel syndrome according to a series of defined parameters, which can include the amplitude of the sensory action potential and the distal motor latency. However, criteria vary between laboratories, and there is often poor correlation of symptom severity with neurophysiological severity. Thus, severity grading may not be clinically useful and should be interpreted with caution.
Although useful, nerve conduction studies can produce false negative results in mild cases, or where intermittent ischaemia of the median nerve occurs without more prolonged demyelination.3 A repeat study after an interval of several months can help to identify such cases.
Radiological investigations: Ultrasonography and magnetic resonance imaging (MRI) can be used in the evaluation of carpal tunnel syndrome, to examine the dimensions of the median nerve at various points along its course and to detect macroscopic compression. However, commonly due to resource constraints with MRI and operator dependence with ultrasound, neither test is used in routine clinical practice at present.3
Clare’s likely diagnosis was bilateral (right worse than left) carpal tunnel syndrome, based on her typical symptoms and neurophysiological evidence of bilateral median neuropathy at the wrist. She had no evidence of an underlying systemic disorder such as rheumatoid arthritis or endocrinopathy. Her manual occupation and recent weight gain were predisposing or exacerbating factors (Box 3).
Two Cochrane reviews have evaluated non-surgical treatments for carpal tunnel syndrome (Grade A evidence).5,6 One review (12 trials, 671 patients) found local corticosteroid injections in the region of the carpal tunnel to be more effective than placebo at 1 month (relative risk, 2.58; 95% CI, 1.72–3.87), and relative to oral steroids at 3 months, with no benefit shown for multiple injections over single injections.5 The other review (24 trials, 884 patients) found moderate evidence (from more than one randomised controlled trial) of short-term benefits (up to 3 months) from oral steroids, typically doses of 10–20 mg of prednisolone per day, and limited evidence (from one randomised controlled trial) in favour of therapeutic ultrasound, splinting and carpal bone mobilisation, which involves physiotherapy-based techniques and stretching to “move” the bones and ligaments of the wrist.6 Few trials have examined long-term outcomes of non-surgical treatments.
Surgery for carpal tunnel syndrome may be performed by hand surgeons, orthopaedic surgeons, plastic surgeons or neurosurgeons. Two Cochrane reviews have evaluated surgical treatments of carpal tunnel syndrome (Grade A evidence). One review (four trials, 317 patients) demonstrated a clear benefit of surgery over splinting overall, although there was insufficient evidence regarding the effect of surgical treatment in the subgroup of milder cases or its relative efficacy over local steroid injection.7 The second review (33 trials, total number of patients not reported) compared endoscopic with open carpal tunnel release, and demonstrated equivalence in short-term and long-term outcomes between these techniques.8
Endoscopic decompression probably shortens the recovery period in uncomplicated carpal tunnel syndrome by about 6 days from an average of around 4 weeks,8 but it is not recommended in complicated cases where there is wrist deformity from arthritis or old fractures.
Prognosis after surgery can be difficult to predict, but a worse outcome is associated with longer duration of symptoms (> 6 months), older age, preoperative thenar wasting and poor response to local corticosteroid injection.9 Surgical failure has been associated with incomplete decompression of the carpal tunnel (when the incision has not been extended far enough into the palm). Horizontal incisions along the line of the wrist crease have been abandoned because of a high failure rate and postoperative dysaesthesiae from severing the small palmar cutaneous branch of the median nerve.
Clare trialled wrist splinting for 1 month, but derived no benefit and was referred to a hand surgeon for carpal tunnel release. She underwent endoscopic release of her right carpal tunnel, with a good immediate result. She returned 3 months later to have the left hand treated, again with good relief of her symptoms. Clare successfully returned to work between the two procedures, performing light duties that involved minimal repetitive wrist movement, such as taking orders and answering phones rather than working on the production line, and returned to her full occupational duties 4 weeks after the second procedure. She did not require any further follow-up.
2 How to interpret Clare’s nerve conduction studies
Median sensory nerve conduction study (recording site: wrist) |
|||||||||||||||
Nerve conduction studies for median motor nerve: normal and abnormal (Clare’s)
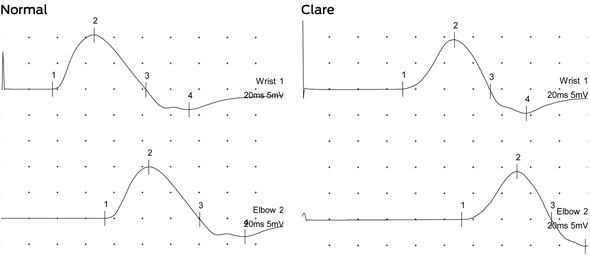 |
3 Pathophysiology of carpal tunnel syndrome
Carpal tunnel syndrome is the most common of the entrapment neuropathies, with a study in the United Kingdom finding an estimated annual incidence of 120 per 100 000 in women and 60 per 100 000 in men.4 It is also a disabling condition; occupation-associated carpal tunnel syndrome reportedly accounts for more work days lost than any other work-related injury or illness, with a median duration off work of 32 days.3
- Marion A Simpson1
- Bruce Day1,2
- 1 MJA 2011; 195: 388–391
- 2 Monash University, Melbourne, VIC.
No relevant disclosures.
- 1. D’Arcy CA, McGee S. The rational clinical examination. Does this patient have carpal tunnel syndrome? JAMA 2000; 283: 3110-3117.
- 2. Jablecki CK, Andary MT, Floeter MK, et al. Practice parameter: electrodiagnostic studies in carpal tunnel syndrome. Report of the American Association of Electrodiagnostic Medicine, American Academy of Neurology, and the American Academy of Physical Medicine and Rehabilitation. Neurology 2002; 58: 1589-1592.
- 3. Hui ACF, Wong S, Griffith J. Carpal tunnel syndrome [review]. Pract Neurol 2005; 5: 210-217.
- 4. Bland JD, Rudolfer SM. Clinical surveillance of carpal tunnel syndrome in two areas of the United Kingdom, 1991–2001. J Neurol Neurosurg Psychiatry 2003; 74: 1674-1679.
- 5. Marshall S, Tardif G, Ashworth N. Local corticosteroid injection for carpal tunnel syndrome. Cochrane Database Syst Rev 2002; (4): CD001554.
- 6. O’Connor D, Marshall S, Massy-Westropp N. Non-surgical treatment (other than steroid injection) for carpal tunnel syndrome. Cochrane Database Syst Rev 2003; (1): CD003219.
- 7. Verdugo RJ, Salinas RA, Castillo JL, Cea JG. Surgical versus non-surgical treatment of carpal tunnel syndrome. Cochrane Database Syst Rev 2008; (4): CD001552.
- 8. Scholten RJPM, Mink van der Molen A, Uitdehaag BMJ, et al. Surgical treatment options for carpal tunnel syndrome. Cochrane Database Syst Rev 2007; (4): CD003905.
- 9. Katz JN, Losina E, Amick BC. Predictors of outcomes of carpal tunnel release. Arthritis Rheum 2001; 44: 1184-1193.





Abstract
Carpal tunnel syndrome, resulting from median nerve compression at the wrist, is a common and often disabling mononeuropathy.
Risk factors include female sex, family history, repetitive hand use, obesity, pregnancy and a variety of medical comorbidities including diabetes mellitus, rheumatoid arthritis, and other connective tissue diseases.
In many cases, an accurate diagnosis can be reached on the basis of clinical history and supportive examination findings alone.
Neurophysiological investigations are essential for confirming the diagnosis, assessing severity and excluding more generalised neuropathies, as well as providing a baseline preoperative index of median nerve function.
Wrist splinting and local corticosteroid injection are effective treatments in the short term, but long-term data are lacking.
Surgical (endoscopic or open) carpal tunnel release is effective and nearly always required to enable a return to work for patients with occupationally induced carpal tunnel syndrome.