Clinical record
A dietary history revealed that the patient had suffered from self-diagnosed food intolerance for most of his life. Since childhood, his diet had consisted exclusively of potatoes, white bread (but he refused to eat butter and margarine) and cola. He described nausea and vomiting after eating any other foods.
Vitamin A deficiency is a systemic illness which can increase an individual’s risk of blindness, severe infections and mortality.1 It is rare in developed countries like Australia.2 Vitamin A deficiency and xerophthalmia in developed countries are reported in patients with malabsorption syndromes or liver disease, in those who have had major gastrointestinal surgery, in people with alcoholism, and in those with anorexia nervosa and other psychiatric disorders.3-6 This case is unique because our patient did not have any of these risk factors.
Vitamin A is a fat-soluble vitamin found as retinol in dairy products and as provitamin A carotenoids in some fruits and green leafy vegetables.1,7-9 The first clinical evidence of vitamin A deficiency often occurs in the visual system and produces xerophthalmia. The ocular changes of xerophthalmia generally occur in a predictable pattern, as described by the World Health Organization.1
The first stage of xerophthalmia is nyctalopia, the result of defective regeneration of retinal rhodopsin.3,7-9 This responds rapidly to vitamin A therapy, and patients often report regaining their scotopic vision (vision under low-light conditions) within 24–48 hours after the initiation of treatment.1,3,7,9
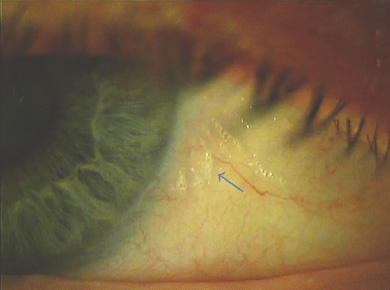
The second stage of xerophthalmia is conjunctival xerosis, or drying, in which loss of goblet cells and squamous metaplasia of the conjunctiva occur.1,3,7,8 Bitôt spots are bilateral triangular patches of keratinised epithelium at the temporal limbus and nasal limbus of the eye.1,3,7 Colonisation of these patches by saprophytic bacilli, including Corynebacterium xerosis, results in a foamy appearance.1,3,8 Conjunctival xerosis and Bitôt spots respond to vitamin A therapy in 1–5 days.1,3
Corneal xerosis occurs primarily because of instability of the tear film as goblet cells are lost, with subsequent keratinising metaplasia of the ocular surface.1,8 Corneal xerosis usually responds to vitamin A therapy in 1–2 weeks.1,9 If left untreated, corneal drying can result in ulceration, with subsequent scarring and keratomalacia.2,3,7,8 Keratomalacia is a rapidly progressive and irreversible liquefactive necrosis of the cornea that can ultimately lead to perforation and spontaneous loss of intraocular contents.1,3,9
Lessons from practice
Vitamin A deficiency is rare in developed countries like Australia.
Visual symptoms can often be the first manifestation of a systemic illness, such as vitamin A deficiency.
A thorough nutritional screen, including a dietary history, is essential, especially in the context of any other nutritional deficiency.
Early diagnosis and treatment of vitamin A deficiency can be curative, preserving vision and life.
Uncommonly, in vitamin A deficiency, the xerophthalmic fundus exhibits yellow and white dots peripherally, sometimes associated with a corresponding scotoma (area of diminished vision).1,7-10 These changes respond well to treatment, often returning to normal within 2–4 months.1,8,9
The diagnosis of vitamin A deficiency is made by a directed history and clinical findings, and confirmed by the presence of a low serum vitamin A level, and an abnormal electroretinography result.3,9 In our case, the diagnosis was made accordingly, and all the pathological findings resolved with vitamin A therapy.
Vitamin A deficiency is usually treated by administering 200 000 IU of vitamin A orally on two successive days, followed by an additional dose 1–4 weeks later.1 Administration of intramuscular vitamin A is reserved for patients with malabsorption, or those who are unable to tolerate medications orally.1 Ocular vitamin A has not been shown to be beneficial because of the systemic nature of vitamin A deficiency.7
- 1. Sommer A. Vitamin A deficiency and its consequences: a field guide to detection and control. 3rd ed. Geneva: World Health Organization, 1995.
- 2. Karande S, Jagtap S, Le Mesurier RT. Ocular sequelae of vitamin A deficiency [snapshot]. Med J Aust 2008; 188: 308. <MJA full text>
- 3. Roncone DP. Xerophthalmia secondary to alcohol-induced malnutrition. Optometry 2006; 77: 124-133.
- 4. Watson NJ, Hutchinson CH, Atta HR. Vitamin A deficiency and xerophthalmia in the United Kingdom. BMJ 1995; 310: 1050-1051.
- 5. Qureshi SH, Selva-Nayagam DN, Crompton JL. Hypovitaminosis in metropolitan Adelaide. Clin Experiment Ophthalmol 2000; 28: 62-64.
- 6. Cooney TM, Johnson S, Elner VM. Keratomalacia caused by psychiatric-induced dietary restrictions. Cornea 2007; 26: 995-997.
- 7. Harris EW, Loewenstein JI, Azar D. Vitamin A deficiency and its effects on the eye. Int Ophthalmol Clin 1998; 38: 155-161.
- 8. Congdon NG, West KP. Nutrition and the eye. Curr Opin Ophthalmol 1999; 10: 464-473.
- 9. Smith J, Steineman TL. Vitamin A deficiency and the eye. Int Ophthalmol Clin 2000; 40: 83-91.
- 10. Sommer A. Xerophthalmia, keratomalacia and nutritional blindness. Int Ophthalmol 1990; 14: 195-199.





We thank Rahul Dubey, Michael C Wei, Philip J Townend, Tanya Karaconji, Ravjit Singh and Ashish Agar for their valuable contributions to this case report.
No relevant disclosures.