People feel well and ill or in dis-ease in their own ways, whether in the presence or absence of identifiable biomedical causes. Social and family context, educational attainment, employment status, local environment and many other factors are known to be important modulators of the health/illness/dis-ease experience.2-3
Health, illness and dis-ease are subjective experiences that need to be distinguished from the objective findings of abnormality.4 Our training has focused on pattern recognition, that is, identifying symptoms and signs that are associated with abnormalities, so that we can give them names (diagnoses) and offer ways of managing them (investigations and treatments). Yet, when feeling ill, people demand more than just the identification and amelioration of biomedical abnormalities: they look for healing,5 the restoration of their personal experience of health.
The manner in which health systems function is clearly fundamental to the achievement of these more complex (diverse and variable) personal outcomes. Structures and processes encompass both the direct care of individuals within their local community, and the multiple levels of health services organisations at local, regional and state levels. We can observe patterns in the functioning of health systems that reflect the system’s underlying complex adaptive dynamics.6 Heath systems are now recognised to be complex adaptive systems (CASs) composed of multiple components (agents) that display diversity, interconnectedness, interdependency and adaptation to input.
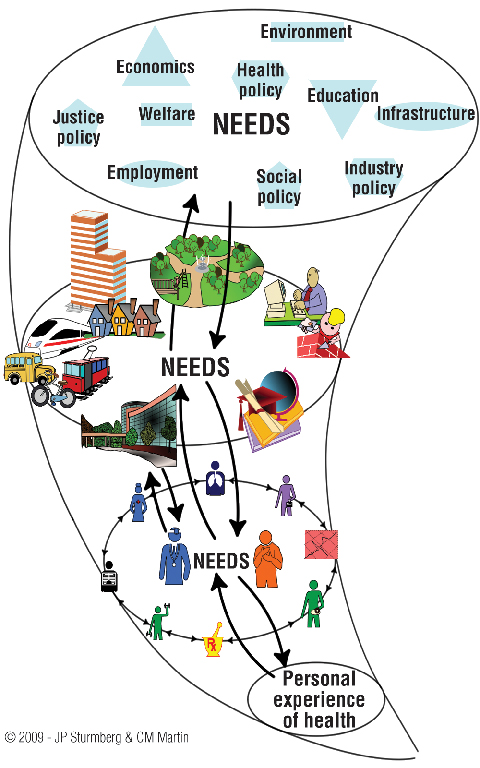
The observed overall behaviour of the system is the result of a huge number of “decisions” or “actions” taken every moment by many individual agents.7 An example of one type of CAS demonstrating complex interactions between pattern, structure and function has been described by Capra through the “vortex funnel of the whirlpool in a bathtub”.8 Despite a health system not actually being a vortex, the vortex metaphor provides many insights to inform health system redesign.
The current health care reform debate offers an opportunity to put the patient into the centre of the healthcare system and to think about the health system and health care delivery as a CAS. The attractor for a people-centred complex adaptive health system ought to be the achievement of the individual patient’s best possible experience of health,5,9 a driver that is distinctively different from those that are currently in place, which focus on diseases and standardised protocol-driven disease management based on the “average” patient.
While the general directions outlined in the Council of Australian Governments (COAG) health agreement (19–20 April 2010)10 are laudable (integrating care, improving access to and responsiveness of care), the specifics (Schedule B — Primary Health Care and Primary Health Care Organisations)11 are worrying, as the general focus remains financial, administrative and micromanagerial, potentially neglecting individual health beliefs and aspirations, and assuming that people will behave according to designed service pathways. A window of opportunity remains to explore how best to design a people-centred health system.
Box 1 shows the healthcare vortex as a metaphorical representation of a complex adaptive people-centred health system. At its centre is the patient’s experience of health — the system’s core attractor — all agents and interactions align and constantly realign around this.
As the people-centred healthcare vortex (Box 1) illustrates, each layer of the system assumes a different responsibility, each with its own “subdriver”. However, as an interconnected whole, all are “attracted to” the system’s core driver at the centre. Through feedback loops, agents in and across every layer fine-tune to optimally respond to the system’s drivers. If, instead of the patient’s health experience, the core drivers are “disease management” or “cost containment”, the system will constantly realign itself around these “less appropriate” drivers.
Our personal and unique experience of health emerges from self-awareness — our ability to make sense of our physical, emotional and social life experiences — and is interrelated with our disorders, moods, social and cognitive circumstances.2,12 The individual is the main agent at this level who optimises his health according to his biopsychosocial and environmental milieu.
Individual service provision represents the microlevel of the healthcare system. When feeling ill, people most commonly seek care from their general practitioner or, less frequently, from pharmacists, nurses, physiotherapists and others. GPs work with people first, at the interface between health, illness and dis-ease,2,13 and between the community and the formal medical care system. They are usually the first to know or identify patterns when things go wrong, when complex human bodies lose their adaptive and self-healing capacities in light of challenges in their natural, physical, social and psychological environments.
Many of these patterns do not fit neatly into conventional discrete diagnostic categories. The core requirement for effective and efficient care at this level is the ability to deal with uncertainty, undifferentiated illness and the management of most chronic stable conditions — this is the particular expertise of the primary care doctor.14 Making sense of the patient’s concerns in this environment is facilitated by an ongoing relationship of trust over time;15 and more time spent with the patient reduces future consumption of scarce health system resources, be they investigations, medications, referrals or hospitalisations.16,17
The local health service integrates local health needs in the context of the immediate environment to create a unique community health service.2-3 The term “health service” embraces three interrelated dimensions — the health-promoting nature or otherwise of local community factors, the engagement with people’s dis-ease and, where required, the delivery of specific medical interventions for discrete disorders. It is this engagement between the community and local health service providers that shapes the local system.
A well functioning people-oriented mesolevel has been shown to deliver greater equity and access to health care, achieve better results against population health indicators, and do so with greater cost-effectiveness.18,19
In a people-centred health system, politicians, health system funders and decisionmakers will embrace health, illness and dis-ease as necessarily personal and local phenomena. The national health framework will consider medical, social and environmental factors when defining the goals and subgoals, policies, principles, broad strategies and equitable resource allocation that enable local (primary) health services to respond flexibly to local care needs.13 A performance and evaluation framework can then be developed which is subservient to, and supportive of, the goal of a people-centred health system.
The need for this macro health framework was outlined in the National Health and Hospitals Reform Commission (NHHRC) report20 and accepted by the COAG.10
Mayo Clinic is a good example of how a core driver — the needs of the patient come first — has shaped function and structure within an organisation’s CAS in a truly patient-centred fashion to achieve its intended outcomes of high-quality care and patient satisfaction at reduced health costs.21 This critical link between a strong patient health focus and improved patient satisfaction, health outcomes and cost is increasingly accepted.18,22 In contrast, the NHHRC’s vision — “a sustainable, high quality, responsive health system for all Australians now and into the future”20 has a prominent focus on the health system, representing a fundamental difference between the visions of Mayo Clinic and the NHHRC; it immediately constrains the scope of possible decisions and actions.
As an example, Box 2 presents an analysis of one NHHRC statement concerning the envisaged directions and outcomes for Australian health care reform across the four organisational levels in the healthcare system. The notion that “we need to redesign health services around people”20 does not appear to be reflected in the thinking23 about the future of the Australian healthcare system. The statement (shaded pink) is:
concrete in regard to economics but vague and somewhat “motherhood” in nature in regard to health care and health services and their organisation; and
concentrated on the macrolevel and, to a lesser degree, the mesolevel, with little to say about the microlevel and individual level.
We have reframed23 this statement to reflect a patient-centred perspective (Box 2, shaded orange) to highlight the important differences. It should be evident that our approach allows for the emergence of dispersed local solutions to the health issues of individuals and communities. The right national health framework will facilitate this “localisation” without compromise to quality, accountability or sustainability.
In practical terms, responsive and appropriate health services would emerge at the local level, based on the knowledge of people, families and communities.24 Process would follow function; general practice-based teams, multidisciplinary care within or across services, and engagement with other sector services would emerge from patients’ personal health needs.25 Individual care would be personalised, being informed (but not dominated) by research findings and opinions based on the “average population”.
In a people-centred health system, financing would require a rational and equitable reallocation of resources according to the nature and level of patients’ and communities’ needs and the outcomes achieved, rather than rationing resources at policy or program/service levels.24 A broadening of the accounting principles associated with health care would eliminate poor investment decisions while strengthening public accountability for health and personal health achievements.17,26
Describing the complex adaptive nature of the health system through the vortex metaphor clearly articulates the opportunities and challenges arising from health system redesign with the improvement of people’s health and health experiences as its main driver. An appreciation of this whole-systems (CAS) view should safeguard against potentially dangerous decisions typically arising from either simplistic interventions or a partial understanding of the system.26-28
Successful health care reform — balancing patient needs and economic sustainability — can only be achieved by aligning the social and environmental determinants of health with accessible, efficient, effective and supportive care environments to achieve and strengthen individual and community health.17 Reorganisation should be locally adaptive, strengthening access to comprehensive integrated care focused on the whole-person, the family and the community.
Last, but not least, successful health systems reform must be assessed against its core driver — has it achieved an improvement in peoples’ health experiences?2
1 Vortex representation of the healthcare system, highlighting the patterns of its organisation, its structures and processes
 |
2 Healthcare reform — comparing National Health and Hospitals Reform Commission (NHHRC) recommendations with “people-centred” recommendations
The final report of the NHHRC20 lists three reform goals, of which we have chosen the second, Redesigning our health system to meet emerging challenges, to illustrate a comparison of the NHHRC approach and a person-centred rephrasing of the same policy objectives.
- Joachim P Sturmberg1,2
- Diana M O’Halloran3
- Carmel M Martin4,5
- 1 Department of General Practice, Monash University, Melbourne, VIC.
- 2 Department of General Practice, University of Newcastle, Newcastle, NSW.
- 3 Department of General Practice, University of Western Sydney, Sydney, NSW.
- 4 Northern Ontario School of Medicine, Sudbury, ON.
- 5 Department of Public Health and Primary Care, Trinity College, Dublin.
Joachim Sturmberg is Chair of the World Organization of Family Doctors (WONCA) Special Interest Group on Systems and Complexity in Health and a member of the special interest group on complexity sciences of the North American Primary Care Research Group (indirect interest only). Carmel Martin received consultancy fees from Ontario College of Family Physicians (via the Primary Health Care Transition Fund [PHCTF]), Health Canada’s PHCTF National Evaluation Strategy, and Balanced Scorecard from the Ministry of Health and Long Term Care, Ontario, a grant for the Patient Journey Record project from the National Digital Research Centre, Dublin, fees as a lecturer on complex systems for Trinity College, Dublin, and is a member of the special interest group on complexity science of the North American Primary Care Research Group. Diana O'Halloran received fees as chair of the board of WentWest (a division and regional training provider — indirect interest only), consultancy fees from NSW Health as Chair of the General Practice Advisory Committee, and sessional payments from the Royal Australian College of General Practitioners for chairing (i) the Presidential Task Force on Health Reform and (ii) the National Standing Committee — Education (indirect interest only), and also provides advice to NSW Health on general practice-related matters including the Primary Health Care Research Capacity Building Program (indirect interest only).
- 1. Mayo Clinic. Tradition and heritage. The needs of the patient come first. The best interest of the patient. http://www.mayoclinic.org/tradition-heritage/best-interest-patient.html (accessed Sep 2010).
- 2. Sturmberg JP. The foundations of primary care. Daring to be different. Oxford: Radcliffe Publishing, 2007.
- 3. World Health Organization Western Pacific Region. People at the centre of health care. Harmonizing mind and body, people and systems. Geneva: WHO Western Pacific Region, 2007.
- 4. Lewis SJ. Illness — an under-rated biological phenomenon. http://sites.google.com/site/sjlewis55/presentations/sshb2007 (accessed Sep 2010).
- 5. Egnew TR. The meaning of healing: transcending suffering. Ann Fam Med 2005; 3: 255-262.
- 6. McDaniel RRJ, Lanham HJ, Anderson RA. Implications of complex adaptive systems theory for the design of research on health care organizations. Health Care Manage Rev 2009; 34: 191-199.
- 7. Cilliers P. Complexity and postmodernism. Understanding complex systems. London: Routledge, 1998.
- 8. Capra F. The web of life. London: HarperCollins Publishers, 1996.
- 9. Sturmberg JP, Martin CM, Moes M. Health at the centre of health systems reform — how philosophy can inform policy. Perspect Biol Med 2010; 53: 341-356.
- 10. The Council of Australian Governments (COAG). Council of Australian Governments Meeting 19 and 20 April 2010, Canberra. Communiqué. http://www.coag.gov.au/coag_meeting_outcomes/2010-04-19/docs/communique_20_April_2010.pdf (accessed Sep 2010).
- 11. Council of Australian Governments. National Health and Hospitals Network Agreement. Canberra, 2010. http://www.coag.gov.au/coag_meeting_outcomes/2010-04-19/docs/NHHN_Agreement.pdf (accessed Sep 2010).
- 12. Sturmberg JP. The personal nature of health. J Eval Clin Pract 2009; 15 (4): 766-69.
- 13. McWhinney IR. Primary care: core values. Core values in a changing world. BMJ 1998; 316: 1807-1809.
- 14. Frenk J. Reinventing primary health care: the need for systems integration. Lancet 2009; 374: 170-173.
- 15. Sturmberg JP, Cilliers P. Time and the consultation — an argument for a “certain slowness”. J Eval Clin Pract 2009; 15: 881-885.
- 16. Hart JT. Expectations of health care: promoted, managed or shared? Health Expect 1998; 1: 3-13.
- 17. Meliones J. Saving money, saving lives. Harv Bus Rev 2000; 78: 57-65.
- 18. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q 2005; 83: 457-502.
- 19. Stange KC, Ferrer RL. The paradox of primary care. Ann Fam Med 2009; 7: 293-299.
- 20. National Health and Hospitals Reform Commission. A healthier future for all Australians. Final report June 2009. Canberra: NHHRC, 2009.
- 21. Mayo Clinic Health Policy Centre. 2010 Symposium: Achieving the vision — advancing high-value health care. http://www.mayoclinic.org/healthpolicycenter/recommendations.html (accessed Sep 2010).
- 22. Wennberg D, Berkson D, Rider B. Building partnerships: addressing overuse, underuse and misuse of care. Healthc Exec 2008; 23: 8-10, 12, 14-15.
- 23. Lakoff G, Johnsen M. Metaphors we live by. London: University of Chicago Press, 2003.
- 24. Stange KC. A science of connectedness. Ann Fam Med 2009; 7: 387-395.
- 25. Haggerty J, Martin CM. Evaluating primary health care in Canada: the right questions to ask. http://www.apps.hc-sc.gc.ca/hcs-sss/phctf-fassp.nsf/WebProject/0069?OpenDocument&lang=eng& (accessed Sep 2010). Full document available on request from the authors.
- 26. Shiell A, Hawe P, Gold L. Complex interventions or complex systems? Implications for health economic evaluation. BMJ 2008; 336: 1281-1283.
- 27. Dörner D. The logic of failure: recognizing and avoiding error in complex situations. New York: Metropolitan Books, 1996.
- 28. Martin CM, Sturmberg JP. Implementing case management — understanding principles and learnings from complex adaptive systems. BMJ 2007; 334: 31. http://www.bmj.com/content/334/7583/31.abstract/reply#bmj_el_157091 (accessed Sep 2010).





Abstract
Health systems are increasingly recognised to be complex adaptive systems (CASs), functionally characterised by their continuing and dynamic adaptation in response to core system drivers, or attractors.
The core driver for our health system (and for the health reform strategies intended to achieve it) should clearly be the improvement of people’s health — the personal experience of health, regardless of organic abnormalities; we contend that a patient-centred health system requires flexible localised decision making and resource use.
The prevailing trend is to use disease protocols, financial management strategies and centralised control of siloed programs to manage our health system. This strategy is suggested to be fatally flawed, as:
people’s health and health experience as core system drivers are inevitably pre-empted by centralised and standardised strategies;
the context specificity of personal experience and the capacity of local systems are overlooked; and
in line with CAS patterns and characteristics, these strategies will lead to “unintended” consequences on all parts of the system.
In Australia, there is still the time and opportunity for health system redesign that truly places people and their health at the core of the system.