Health care reform is a perpetual “political hot potato”, with successive governments talking about the “right” solution for our ailing health system. The way we talk about these reforms matters: as Lakoff has pointed out, the metaphors we use unveil our perceptions, our ways of thinking, and most importantly, our ways of acting.1 So far, debate on health care reform has predominantly been about diseases, although in recent times, the issues of community-based health and illness care for the majority of people have begun to permeate the argument.
This metaphor suggests that the current challenges (our ageing population, increasing levels of chronic illness, high-cost interventions and health workforce shortages) are unmanageable. This is based on a view of health as a negative state — the absence of disease and infirmity (Box 1). Not surprisingly, the focus on disease and infirmity steers discussions towards disease-specific management by hospital specialists, the use of high-cost technologies and therapies, and the need to control medical practice.
The emphasis on a disease-oriented environment — reinforced by media hype — fuels people’s perceptions of a steady decline in their health, exaggerates anxieties about disease and disease risk,2 encourages the denial of death as the eventual endpoint of care, and perpetuates unrealistic expectations of cure or treatment for every ailment.
Over the past century, our disease-free life span and our capacity to manage ill health have increased dramatically. However, vested interest groups and the media are fostering the medicalisation of everyday life by overstating the relevance of everyday symptoms, the risk of future disease, and the successes of novel experimental treatments. Having conquered premature death from acute infectious disease, most of us live with, and will die from, chronic degenerative diseases. Archie Cochrane’s insights are pertinent in this context: “Cure is rare while the need for care is widespread, and ... the pursuit of cure at all costs may restrict the supply of care”.3
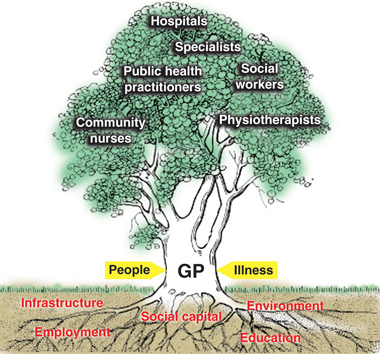
If we regard the current way of thinking as “barking up the wrong tree”, what would the right tree look like (Box 2)? Like a tree, which needs solid foundations to grow and thrive, the health system does not develop autonomously — it is bound and constrained by the broader health, societal and environmental system, and the functioning “whole” of the health system is clearly greater than the sum of its parts.
The focus of GPs/primary care physicians differs markedly from that of other medical professionals. We focus on people, not diseases. Primary care operates in the realm of uncertainty, as people present feeling ill — not diseased or pathological — and expect to be healed, in that they want to feel whole again, rather than achieve the absence of identifiable pathology.4 Healing, since the time of our ancient forebears, has been based on trust, an ongoing relationship between the doctor/healer and patient, and seeing and understanding the patient’s illness as a problem of the whole person in his or her environment.4
Looking specifically at general practice (rather than the broader primary health care system), we regard it as a function of the health system and emphasise the characteristics associated with its proven cost-effectiveness: person-focused care and the C’s of primary care — competence, continuity, comprehensiveness and coordination, inevitably associated with communication, collaboration, compliance and balancing competing demands (Box 3).5
The core function of a tree is to produce fruit; the core function of the health system is to produce health. The fruits of care are represented by our patients’ experience of health, both in the presence and absence of identifiable pathologies.6,7
The reconfigured health system we envisage will primarily measure health, rather than focusing on disease-specific indicators or mortality statistics to demonstrate its achievements.6,7 The difference is important, as recent experiences in the United Kingdom have shown that an undue focus on disease-specific processes and outcomes (especially if imposed without adequate professional review, and attracting financial reward) can rapidly distract from the central components of care that achieve good health outcomes.8-10 The UK has realised the importance of patient health measures and has started to develop indicators.7
Internationally, there is now a strong move towards people-centred health care, with flexible teams configured around the primary care physician.4 This is known to be associated with better, more equitable and more cost-effective care.11
The National Health and Hospitals Reform Commission’s interim report highlights the centrality of the individual and family as the focus for our future reform energies.12 The National Primary Health Care Strategy has identified the importance of continuity of care and a holistic health focus, and the recently established Preventative Health Taskforce will explore the powerful link between health and behaviour.
These skills are particularly important when dealing with patients affected by multiple morbidities, whose management requires integration and coordination, ideally delivered within flexible team-based arrangements at the practice level.13 This is teamwork through clinical leadership, expanded health professional roles and delegation, rather than role substitution. The crucial importance of continuity of care with a primary care provider, rather than a service, is increasingly emerging as the missing ingredient in health care reform, both in Australia and internationally.
- Joachim P Sturmberg1,2
- Diana E O’Halloran3
- Claire Jackson4
- Christopher D Mitchell5
- Carmel M Martin6
- 1 Monash University, Melbourne, VIC.
- 2 University of Newcastle, Newcastle, NSW.
- 3 University of Sydney, Sydney, NSW.
- 4 University of Queensland, Brisbane, QLD.
- 5 Lennox Head, NSW.
- 6 Northern Ontario School of Medicine, Sudbury, Ontario, Canada.
None identified.
- 1. Lakoff G, Johnsen M. Metaphors we live by. Chicago: University of Chicago Press, 2003.
- 2. Barsky A. The paradox of health. N Engl J Med 1988; 318: 414-418.
- 3. Cochrane AL. Effectiveness and efficiency: random reflections on the health services. London: Nuffield Hospitals Trust, 1972.
- 4. Sturmberg JP. The foundations of primary care: daring to be different. Oxford: Radcliffe Publishing, 2007.
- 5. Kroenke K. The many C’s of primary care. J Gen Intern Med 2004; 19: 708-709.
- 6. Hart J. Expectations of health care: promoted, managed or shared? Health Expect 1998; 1: 3-13.
- 7. Timmins N. NHS goes to the PROMS. BMJ 2008; 336: 1464-1465.
- 8. Campbell SM, McDonald R, Lester H. The experience of pay for performance in English family practice: a qualitative study. Ann Fam Med 2008; 6: 228-234.
- 9. Guthrie B, McLean G, Sutton M. Workload and reward in the Quality and Outcomes Framework of the 2004 general practice contract. Br J Gen Pract 2006; 56: 836-841.
- 10. Steel N, Maisey S, Clark A, et al. Quality of clinical primary care and targeted incentive payments: an observational study. Br J Gen Pract 2007; 57: 449-454.
- 11. Wennberg D, Berkson D, Rider B. Building partnerships: addressing overuse, underuse and misuse of care. Healthc Exec 2008; 23: 8-10, 12, 14-15.
- 12. National Health and Hospitals Reform Commission. A healthier future for all Australians. Interim report December 2008. Canberra: NHHRC, 2009. http://www.nhhrc.org.au/internet/nhhrc/publishing.nsf/Content/interim-report-december-2008 (accessed May 2009).
- 13. Martin CM, Sturmberg JP. Complex adaptive chronic care. J Eval Clin Pract 2009; 15: 571–577.





Abstract
Current approaches to health care reform are largely based on the metaphor of imminent flood waves threatening to inundate the health care system. This metaphor reflects the system’s preoccupation with disease and disease management in a hospital-centric environment.
We suggest that the debate needs to be reframed around health, or more precisely the patient’s health experience. Most patients are healthy most of the time, and even those with identifiable morbidities generally regard themselves as being in good health.
The majority of people receive most of their care in the community from primary care professionals. An integrated, effective and efficient primary health care system supports continuity of care through a primary care provider and fosters clinical leadership that is supported by other primary health care professionals and medical specialists.
Each primary care setting will have its own model that best provides flexible and responsive services to meet its patients’ needs and expectations.