The clinical presentation in our case was rather trivial, but the combined results from two basic investigations — an elevated d-dimer level and an abnormal chest x-ray — heightened our clinical suspicion for aortic dissection and led us to perform aortic imaging.
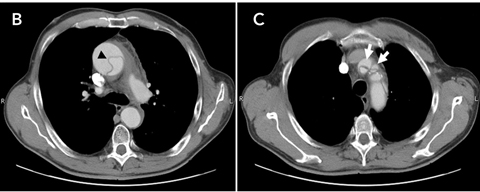
Thoracic aortic dissection generally results from a laceration of the intimal lining of the aorta. This allows blood leakage into the aortic wall resulting in a propagating separation of the aortic media, thereby creating a false blood-filled lumen.1 Hence, the major criterion for definitive diagnosis of aortic dissection includes visualisation of a so-called intimomedial flap that divides the aorta into a true and a false lumen. Several aortic imaging techniques can be used for this purpose, of which contrast-enhanced computed tomography (CT) and transoesophageal echocardiography (TOE) are the most feasible to perform in an emergency department setting.1,2 Moreover, these investigations help to localise the dissection, thereby allowing appropriate classification. Currently, the Stanford classification of aortic dissection is the most widely adopted system.1,2 This system has the virtue of merely dividing aortic dissection into two subtypes, depending on whether the ascending aorta is involved (type A) or not (type B).1,2
While the definitive diagnosis of aortic dissection is usually straightforward, making the initial clinical diagnosis can be extremely challenging. Aortic dissection is associated with a dramatic rate of misdiagnosis and delayed recognition.3 This is no doubt partially explained by the highly variable clinical presentation of the condition.
Our case is a striking illustration of why acute aortic dissection is colourfully called a “clinical chameleon”.1 Although most patients with aortic dissection present with severe chest or back pain (Box 1), the pain can be variably localised to the neck, jaw or throat.4 Throat pain occurs most often in cases of a dissection of the aortic arch, particularly when the supra-aortic vessels are involved. Our patient complained only of a sore throat, and denied having thoracic pain. Only two similar cases have been previously reported.5,6
Moreover, findings on physical examination can be very subtle.1 Classical signs consistent with the diagnosis of thoracic aortic dissection, such as an aortic insufficiency murmur or decreased femoral arterial pulsation, were not present in our patient. According to the International Registry of Acute Aortic Dissection,7 these so-called typical findings are infrequently detected during physical examination (Box 1). In our case, the only notable features of the physical examination were diaphoresis and a right carotid artery murmur. The latter was presumably the result of propagation of the dissection into the right brachiocephalic trunk.
d-dimer analysis has only recently come to the fore, with several studies focusing on the stringent association between the d-dimer level and aortic dissection.3,8,9 The pathophysiological mechanism for this relationship is well explained by the release of tissue factor from the dissected aortic wall. This sets off a cascade of events — activation of the extrinsic coagulation system, generation of fibrin, and secondary fibrinolysis with d-dimer formation.8 The d-dimer assay is reported to have an excellent sensitivity and negative predictive value for aortic dissection (Box 1). The quoted sensitivity is equal for both types of dissection, although absolute d-dimer values tend to be higher in type A aortic dissections as they are usually more extended.10 Given its high sensitivity and negative predictive value, d-dimer testing is an attractive tool for the diagnostic work-up of aortic dissection, particularly in the setting of a low pretest probability for aortic dissection. In such cases, a normal d-dimer result can reliably exclude the presence of aortic dissection, hence obviating the need for further investigations.9,10
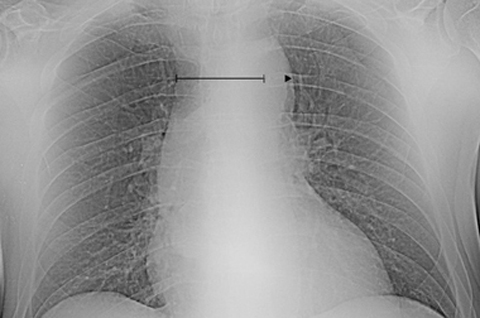
Besides elevation of the d-dimer level, the clinical suspicion for aortic dissection should also be heightened if the chest radiograph is abnormal (Box 1). Mediastinal widening (relative mediastinum to chest-width ratio > 0.25;11 Figure A) is the most common radiographic finding in aortic dissection.7 Of note, absolute estimations of the mediastinal width are practically inaccurate, as these measurements are influenced by the distance between the roentgenographic source and the thorax.12 It is worth mentioning that one in three patients with aortic dissection has a normal chest x-ray.11 Thus, relying on chest radiography alone as the initial diagnostic modality is inefficient as it clearly carries a high risk of misdiagnosis.
When readily available, contrast-enhanced CT and TOE are the preferred imaging modalities in an acute care setting. Both investigations have a comparable diagnostic accuracy and allow a definitive diagnosis of aortic dissection to be established.1,2 However, the diagnosis must first be suspected before it can be confirmed — this case serves as a reminder of this life-threatening condition’s wide variability in clinical presentation, and the need to maintain continuing vigilance.
1 Clinical and basic diagnostic features of thoracic aortic dissection, and percentages of patients presenting with these features who are subsequently diagnosed with Stanford type A or B aortic dissection1,2
Lessons from practice
Thoracic aortic dissection is characterised by a highly variable clinical picture, which has led to the condition being called a “clinical chameleon”.
d-dimer testing can be of value in excluding aortic dissection.
A normal chest x-ray does not rule out the possibility of aortic dissection.
Advanced aortic imaging should be performed early in patients who have symptoms suggestive of aortic dissection in order to prevent misdiagnosis.
- 1. Rehders T, Ince H, Nienaber CA. Aortic dissection: from aetiology to therapeutic management. Medicine 2006; 34: 296-301.
- 2. Golledge J, Eagle KA. Acute aortic dissection. Lancet 2008; 372: 55-66.
- 3. Sutherland A, Escano J, Coon TP. d-dimer as the sole screening test for acute aortic dissection: a review of the literature. Ann Emerg Med 2008; 52: 339-343.
- 4. Vilacosta I, Román JA. Acute aortic syndrome. Heart 2001; 85: 365-368.
- 5. Averbeck T, Hemmanouil I, Bredt M, Stover T. Therapy refractory throat pain. Dissecting aneurysm of the aorta with cardiac tamponade. HNO 2002; 50: 946-947.
- 6. Liu WP, Ng KC. Acute thoracic aortic dissection presenting as sore throat: report of a case. Yale J Biol Med 2004; 77: 53-58.
- 7. Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA 2000; 283: 897-903.
- 8. Marill KA. Serum d-dimer is a sensitive test for the detection of acute aortic dissection: a pooled meta-analysis. J Emerg Med 2008; 34: 367-376.
- 9. Sodeck G, Domanovits H, Schillinger M, et al. d-dimer in ruling out acute aortic dissection: a systematic review and prospective cohort study. Eur Heart J 2007; 28: 3067-3075.
- 10. Ohlmann P, Faure A, Morel O, et al. Diagnostic and prognostic value of circulating d-dimers in patients with acute aortic dissection. Crit Care Med 2006; 34: 1358-1364.
- 11. von Kodolitsch Y, Nienaber C A, Dieckmann C, et al. Chest radiography for the diagnosis of acute aortic syndrome. Am J Med 2004; 116: 73-77.
- 12. Gleeson CE, Spedding RL, Harding LA, Caplan M. The mediastinum — is it wide? Emerg Med J 2001; 18: 183-185.





We wish to pay tribute to Luc Vanuytsel, coauthor of this article, who died suddenly during the internal review phase of this manuscript.
None identified.