The primary health care provider’s initial diagnosis and management can be critical to the patient’s ophthalmic outcome. In one United Kingdom study of 55 patients in which an ophthalmologist had diagnosed a red-eye disorder, only nine had been correctly diagnosed by the referring practitioner.1 To our knowledge, no study of the accuracy of diagnosis of eye conditions by primary health care providers in Australia has yet been published. We audited the hospital records of 1062 new patients presenting to the eye emergency services of the ophthalmology departments of the two major Brisbane hospitals, and analysed the accuracy of the diagnosis and implications of the initial care provided to these patients by their local doctor or optometrist.
Lessons from practice
Patients with acute eye problems presenting to primary health care providers are often misdiagnosed or mismanaged.
Topical antibiotic therapy is overprescribed for acute eye conditions.
Particular attention should be paid to sentinel warning symptoms — in particular the presence of one or more of pain, photophobia or blurred vision — as these symptoms almost always indicate serious acute eye disease rather than conjunctivitis.
If a patient with a red eye reports pain, photophobia or blurred vision he or she should be given no treatment and referred immediately.
Data were collected for 1062 patients during the designated periods at the two hospitals: 614 (57.8%) from PAH and 448 (42.2%) from RBWH. The referring PHCP was a GP in 50.4%, hospital emergency department doctor in 38.9%, and an optometrist in 10.7% of cases. The 10 most common reasons that PHCPs referred patients to ophthalmology departments are shown in Box 1.
Preventable adverse outcomes: In 123 of the 1062 patients (11.6%), there was an adverse outcome resulting from misdiagnosis or mismanagement by the PHCP. Adverse outcomes in these 123 patients were mild in 63 (51%), moderate in 49 (40%) and severe in 11 (9%). Conditions that were misdiagnosed and subsequently associated with a severe adverse patient outcome are shown in Box 2. In most cases (74%), adverse outcomes were associated with misdiagnosis by PHCPs; in the remainder (26%), there had been a correct initial diagnosis, but subsequent incorrect treatment, or a significant delay in referral. In the 123 patients with preventable adverse outcomes resulting from misdiagnosis or mismanagement, the PHCP was a GP in 78%, an emergency department doctor in 17% and an optometrist in 5% of cases. The 11 most severe preventable adverse outcomes are described in Box 3.
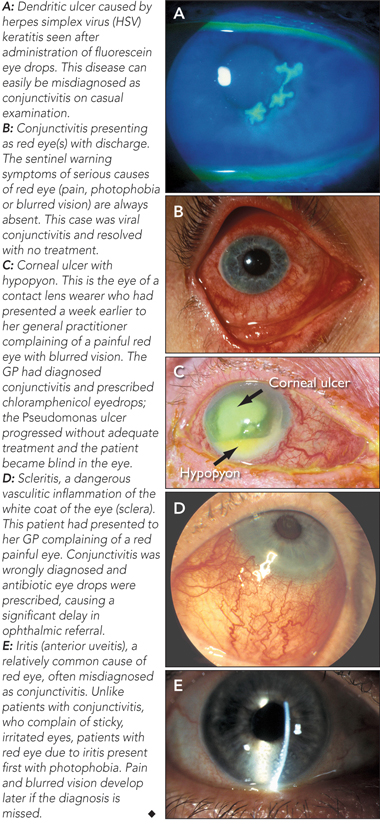
Patients with acute eye problems presenting to PHCPs, especially GPs, are often misdiagnosed or mismanaged. In most cases, this does the patient no harm — for example, misdiagnosing viral conjunctivitis as bacterial conjunctivitis and inappropriately prescribing antibiotic eye drops is unlikely to cause complications, and the patient will spontaneously recover from the infection. However, in some acute eye conditions, the prescription of topical antibiotics can be very harmful indeed — not through any ill effects of the drug, but through the subsequent delay in referral. In the case of serious acute eye conditions like severe iritis or acute glaucoma, a delay of even a few days can result in permanent loss of vision or even blindness. Examples of potentially serious eye diseases that may present to PHCPs are shown in Box 4.
There is a perception among many ophthalmologists that many GPs “call every red eye conjunctivitis” and that topical antibiotics are overprescribed for acute eye problems. In our review, in more than 50% of cases in which topical antibiotic therapy had been commenced by the PHCP, it was immediately ceased at the first ophthalmology review as being unnecessary or inappropriate. In addition to contributing to a serious delay in patient referral, topical antibiotic use can occasionally cause serious local and rarely systemic complications2 (eg, agranulocytosis from chloramphenicol). There may also be concerns that using antibiotics unnecessarily contributes to increasing antibiotic resistance of organisms.3
To address these problems, it is suggested that GPs pay careful attention to the symptoms reported by patients with eye complaints, given the difficulty of accurately evaluating their signs. Particular attention should be paid to sentinel warning symptoms — in particular the presence of one or more of pain, photophobia or blurred vision — as these symptoms almost always indicate serious acute eye disease rather than conjunctivitis.4 Patients reporting one or more of these symptoms should be given no treatment, and referred to an ophthalmologist urgently. It should also be recognised by GPs that although unilateral viral conjunctivitis is common, a single red eye should be viewed with more suspicion than bilateral red eyes, which are more likely due to conjunctivitis.
1 The 10 most common reasons that primary health care providers referred patients to ophthalmology department emergency services
2 Conditions originally misdiagnosed by primary health care providers, leading to adverse events for patients
- 1. Harrison RJ, Wild JM, Hobley AJ. Referral patterns to an ophthalmic outpatient clinic by general practitioners and ophthalmic opticians and the role of these professionals in screening for ocular disease. BMJ 1988; 297: 1162-1167.
- 2. Smith JR, Wesselingh S, Coster DJ. Is it time to stop using chloramphenicol? Aust N Z J Ophthalmol 1997; 25: 83-88.
- 3. Rang HP, Dale MM, Ritter JM, Moore PK. Pharmacology. 5th ed. Edinburgh: Churchill Livingstone, 2003: 644-645.
- 4. Pane A. Practical ophthalmology: a survival guide for doctors and optometrists. Edinburgh: Churchill Livingstone, 2005.





None identified.