Stent thrombosis is an infrequent but severe complication after coronary stent implantation. Dual antiplatelet therapy has markedly reduced the occurrence of this potentially catastrophic event. The optimal duration of clopidogrel therapy in patients with drug-eluting stents is unknown. We describe a case of stent thrombosis 9 days after discontinuation of clopidogrel therapy, more than 3 years after placement of drug-eluting stents. (MJA 2008; 189: 229-230)
Clinical record
Drug-eluting stents (DES) have been shown to be more effective than bare-metal stents (BMS) in reducing angiographic restenosis, by limiting intimal hyperplasia. This reduces the need for subsequent revascularisation procedures.1-3 However, there is growing concern that delayed endothelisation and incomplete neointimal healing might lead to adverse cardiac outcomes and death as a result of late or very late stent thrombosis.4,5 Mortality rates have ranged from 16% in a recent published registry from Spain documenting definite angiographic thrombus6 to as high as 45% in another series including both definite and probable thrombosis.7
Stent thrombosis is an uncommon but life-threatening complication of stent implantation.7,8 Stent thrombosis may be classified according to the time since implantation:9 acute stent thrombosis occurs within 24 hours of the procedure; subacute stent thrombosis between 1 and 30 days after implantation; late stent thrombosis between 1 month and 1 year after implantation; and very late stent thrombosis more than 1 year after the procedure. The cumulative incidence of stent thrombosis with DES at 9–12 months has ranged from 0.5% to 1.5%, which is comparable to stent thrombosis with BMS,10,11 with an incidence as high as 0.6% per year thereafter.12 Recent clinical trials and registries have raised concern over increased rates of very late stent thrombosis with DES.10,13,14 The cessation of dual antiplatelet therapy has been implicated as a pathophysiological factor in late and very late stent thrombosis.7,11,15 Incomplete endothelisation of the metal struts because of the antiproliferative properties of the drug has also been implicated.7,12,15 Mechanical factors involved in stent thrombosis have included malapposition of the stent to the vessel wall when originally implanted, and late malapposition because of retraction of the vessel wall during vessel remodelling.11,12 Whether this is related to the drug, polymer, or stent platform itself is unknown.12 The optimal duration of dual antiplatelet therapy after DES placement is still unknown. Current guidelines recommend clopidogrel therapy for at least a month and ideally up to a year with BMS, and for at least a year for patients treated with DES after hospitalisation for an acute coronary syndrome.16 However, reports of very late cardiac events among patients with DES, particularly in relation to stent thrombosis and cessation of clopidogrel therapy, have cast doubt on these recommendations.10,17,18 A recent observational study comparing DES with BMS suggested that clinical events related to late stent thrombosis in patients with DES after the discontinuation of clopidogrel therapy might limit the benefit of DES.10
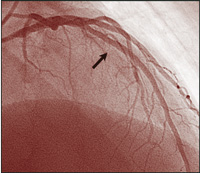
Though there have been similar case reports,17,18 ours is a unique example of an angiographically proven very late stent thrombosis, 3 years after placement of DES. During angiography 9 days prior to the event, no abnormality was noted within the previously implanted DES, nor at the stent edges before the cessation of clopidogrel therapy. Nine days after stopping therapy with this drug, filling defects were seen (Figure, B).
- 1. Morice MC, Serruys PW, Sousa JE, et al. A randomized comparison of a sirolimus-eluting stent with a standard stent for coronary revascularization. N Engl J Med 2002; 346: 1773-1780.
- 2. Moses JW, Leon MB, Popma JJ, et al. Sirolimus-eluting stents versus standard stents in patients with stenosis in a native coronary artery. N Engl J Med 2003; 349: 1315-1323.
- 3. Stone GW, Ellis SG, Cannon L, et al. Comparison of a polymer-based paclitaxel-eluting stent with a bare metal stent in patients with complex coronary artery disease: a randomized controlled trial. JAMA 2005; 294: 1215-1223.
- 4. Ong ATL, McFadden EP, Regar E, et al. Late angiographic stent thrombosis (LAST) events after drug-eluting stents. J Am Coll Cardiol 2005; 45: 2088-2092.
- 5. Nordmann AJ, Briel M, Bucher HC. Mortality in randomized controlled trials comparing drug-eluting vs bare metal stents in coronary artery disease: a meta-analysis. Eur Heart J 2006; 27: 2784-2814.
- 6. de la Torre-Hernández JM, Alfonso F, Hernández F, et al. Drug-eluting stent thrombosis: results from the multicenter Spanish registry ESTROFA (Estudio ESpañol sobre TROmbosis de stents FArmacoactivos). J Am Coll Cardiol 2008; 51: 986-990.
- 7. Iakavou I, Schimdt T, Bonizzoni E, et al. Incidence, predictors and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA 2005; 293: 2126-2130.
- 8. Ong ATL, Hoye A, Aoki J, et al. Thirty-day incidence and six-month clinical outcome of thrombotic stent occlusion after bare-metal, sirolimus, or paclitaxel stent implantation. J Am Coll Cardiol 2005; 45: 947-953.
- 9. Cutlip DE, Windecker S, Mehran R, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation 2007; 115: 2344-2351.
- 10. Pfisterer M, Brunner-La Rocca HP, Buser PT, et al; BASKET-LATE Investigators. Late clinical events after clopidogrel discontinuation may limit the benefit of drug-eluting stents: an observational study of drug-eluting versus bare-metal stents. J Am Coll Cardiol 2006; 48: 2584-2591.
- 11. Moreno R, Fernandez C, Hernandez R, et al. Drug-eluting stent thrombosis results from a pooled analysis including 10 randomised studies. J Am Coll Cardiol 2005; 45: 954-959.
- 12. Serruys PW, Daemen J. Late stent thrombosis: a nuisance in both bare metal and drug-eluting stents. Circulation 2007; 115: 1433-1439.
- 13. Stone GW, Moses JW, Ellis SG, et al. Safety and efficacy of sirolimus- and paclitaxel-eluting coronary stents. N Engl J Med 2007; 356: 998-1008.
- 14. Kastrati A, Mehilli J, Pache J, et al. Analysis of 14 trials comparing sirolimus-eluting stents with bare-metal stents. N Engl J Med 2007; 356: 1030-1039.
- 15. Eisenstein EL, Anstrom KJ, Kong DF, et al. Clopidogrel use and long term clinical outcomes after drug-eluting stent implantation. JAMA 2007; 297: 159-168.
- 16. Anderson JL, Adams CD, Antman EM, et al; American College of Cardiology; American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-elevation Myocardial Infarction); American College of Emergency Physicians; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons; American Association of Cardiovascular and Pulmonary Rehabilitation; Society for Academic Emergency Medicine. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol 2007; 50: e1-e157.
- 17. McFadden EP, Stabile E, Regar E, et al. Late thrombosis in drug-eluting coronary stents after discontinuation of antiplatelet therapy. Lancet 2004; 364: 1519-1521.
- 18. Artang R, Dieter RS. Analysis of 36 reported cases of late thrombosis in drug-eluting stents placed in coronary arteries. Am J Cardiol 2007; 99: 1039-1043.







None identified.