There are many strategies to address rural workforce shortages in Australia, but the two most often reported are the rural clinical school program, which represents a visionary educational response, and the recruitment of international medical graduates (IMGs), which represents the most substantial labour initiative. Reflecting international trends, the total number of IMGs in Australia is steadily increasing.1,2 The point of entry into the workforce for most of them is through selective intake to designated rural and remote areas of unmet need, with corresponding location-restricted provider numbers. While nationally they comprise at least 25% of the general practice workforce,3 more than a third of rural general practitioners are IMGs (37% in 2005–064). Thus, these two workforce strategies geographically overlap in Australia’s vast under-served outback, and in the absence of IMGs, Australia’s rural medical services would be unable to function.5 As Australian rural educators, we argue that Australia’s rural education initiatives would also fail without IMGs.
It is the numerical strength of the ethnically diverse workforce of IMGs in Australia that makes their contribution to practice an issue of interest to the whole medical community. For this reason, IMGs’ clinical practice has been subject to particular scrutiny. With a few notable exceptions,6 most published papers on IMGs highlight their needs (eg, training and cultural orientation) or deficient skill sets,7-10 to the extent that, according to Birrell,1,2 40% of practising IMGs in Australia are not able to pass the Australian Medical Council multiple-choice question exam, yet continue to practise in areas of workforce need. If valid, these statistics are immediately worrying — not only for practice, but also for education. Given the geographical intersection of IMG practice with the locations of rural clinical schools across Australia, it seems timely to explore the educational implications of a rural IMG workforce. Here, we discuss the rural teaching experience of the Rural Clinical School of Western Australia (RCSWA).
Along with the first rural clinical schools formed in Australia, the RCSWA was founded in 2002 with the mandate to educate 25% of a cohort of clinical-year students entirely in the bush. There was no mandate as to who could, or should, be appointed as clinical teachers. As might be expected, given that much of rural WA is classified as an area of workforce need,11 the number of IMG GP clinical academics in the RCSWA reflected their high proportion in the rural GP workforce. Of the 40 doctors appointed as clinical teaching academics at the RCSWA from 2002 to 2007, 28% were IMG GPs (Box 1), compared with a national IMG GP average in 2006 of 35%5 (and a 2007 Rural Health West statistic of 49% for GPs in WA whose basic training was obtained overseas12). Another 15% of the RCSWA clinical teaching academics were IMG specialists (Box 1) — three paediatricians, an obstetrician and gynaecologist, and two general physicians. Thus, the RCSWA had a total IMG workforce of 43%, compared with the 2006 national proportion of 20% of the total medical workforce.5
Of the 17 IMG academics at the RCSWA, most were doctors trained in systems similar to Australia’s (namely the United Kingdom and United States) under “competent authority” programs13 (11 doctors), or in South Africa (3). Of the Australian-graduate staff, 16 were locally trained graduates of the University of Western Australia, and seven represented medical migration within Australia. However, these proportions probably under-represent IMG teaching, as our analysis includes only those IMGs employed directly as university staff, thus excluding IMGs at each site who have been hospital and GP preceptors and mentors.
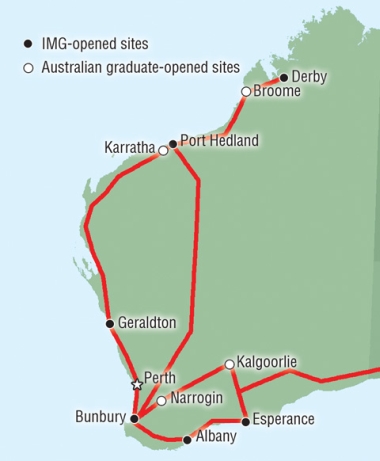
Apart from their substantial staffing contribution, IMG medical coordinators at the RCSWA have been solely responsible for creating rural clinical school centres in six of the 10 currently operating sites (Box 2). Although there is no clear relationship between the size or remoteness of a town and IMG recruitment to the RCSWA, it is apparent that some of the most remote WA sites have consistently been IMG-led, even if this is with an annual succession of newly recruited IMGs, each committed to the RCSWA.
Overall, it appears that the RCSWA has had the involvement of a similar proportion of IMG GPs as the rural GP workforce generally, along with a significant cohort of IMG specialists. However, we contend that the contribution these IMG doctors have made to medical education is disproportionately large compared with what might have been expected from the published literature. We believe that the nationally recognised academic success of the RCSWA14 is largely due to IMG support.
We have also observed that the teaching cohort of IMGs in the RCSWA does not mirror the emerging ethnic patterns of IMGs.1,15 Compared with these patterns, the RCSWA employs disproportionate numbers of teachers from competent authority countries. In this regard, the national implementation of the 2006 recommendation from the Council of Australian Governments to offer a “competent authority pathway” with an accelerated route to registration13 may have significant implications for teaching as well as clinical capacity in rural and remote Australia, if it draws these “competent” clinicians away from rural areas to urban areas for work.
We further contend, based on the RCSWA experience, that focusing on clinical issues without a corresponding analysis of IMGs’ teaching roles may have negatively skewed discussion in the Australian medical fraternity. WA’s IMGs, particularly those from countries with education systems similar to Australia’s, are substantially supporting rural medical education. It appears that they will continue to do so for at least the next decade — at which point the first rural clinical school graduates may be prepared to take over. At this early stage, the workforce impact of rural clinical school graduates is still modest,16-18 and it is yet to be proven whether they will ever supplant the current IMG workforce.
- Denese E Playford1
- Moira A L Maley2
- Rural Clinical School of Western Australia, University of Western Australia, Perth, WA.
None identified.
- 1. Birrell RJ. Australian policy on overseas-trained doctors. Med J Aust 2004; 181: 635-639. <MJA full text>
- 2. Birrell R, Schwartz A. Assessment of overseas trained doctors — the latest chapter. People Place 2007; 15 (3): 67-75.
- 3. Australian Medical Workforce Advisory Committee. The general practice workforce in Australia: supply and requirements to 2013. Sydney: AMWAC, 2005.
- 4. Health Workforce Queensland. ‘Sinking deeper into the abyss’: a concise overview of current and future trends in the Australian urban, rural and remote general practice workforce. Brisbane: HWQ, 2006.
- 5. Spike NA. International medical graduates: the Australian perspective. Acad Med 2006; 81: 842-846.
- 6. Alexander C, Fraser JD. Education, training and support needs of Australian trained doctors and international medical graduates in rural Australia: a case of special needs? Rural Remote Health [Internet] 2007; 7: 681. Epub 2007 Jun 19.
- 7. Arkles RS, Hill PS, Jackson Pulver LR. Overseas-trained doctors in Aboriginal and Torres Strait Islander health services: many unanswered questions. Med J Aust 2007; 186: 528-530. <MJA full text>
- 8. Gardiner M, Sexton R, Kearns H, Marshall K. Impact of support initiatives on retaining rural general practitioners. Aust J Rural Health 2006; 14: 196-201.
- 9. Kidd MR, Zulman A. Educational support for overseas-trained doctors. Med J Aust 1994; 160: 73-75.
- 10. Sullivan EA, Willcock S, Ardzejewska K, Slaytor EK. A pre-employment programme for overseas-trained doctors entering the Australian workforce, 1997–99. Med Educ 2002; 36: 614-621.
- 11. Rural Health West. General practice vacancies. http://www.ruralhealthwest.com.au/go/working-in-wa/general-practice-vacancies (accessed Mar 2008).
- 12. Rural Health West. MDS report and workforce analysis update. November 2007. http://www.ruralhealthwest.com.au/go/about-us/publications (accessed Jun 2008).
- 13. WA Health. Nationally consistent assessment of IMGs: transition to competent authority model. Perth: WA Health, 2007.
- 14. Carrick Institute. Carrick Award recipients 2007. http://www.carrickinstitute.edu.au/carrick/go/home/awards/pid/65 (accessed Mar 2008).
- 15. Scott ML, Whelan A, Dewdney J, Zwi AB. “Brain drain” or ethical recruitment? Solving health workforce shortages with professionals from developing countries. Med J Aust 2004; 180: 174-176. <MJA full text>
- 16. Eley DS, Baker PG. Will Australian rural clinical schools be an effective workforce strategy? Early indications of their positive effect on intern choice and rural career interest. Med J Aust 2007; 187: 166-167. <MJA full text>
- 17. Playford DE, Denz-Penhey H, Skinner L, Murdoch JC. Will Australian rural clinical schools be an effective workforce strategy? Early indications of their positive effect on intern choice and rural career interest [letter]. Med J Aust 2008; 188: 190. <MJA full text>
- 18. Worley P, Martin A, Prideaux D, et al. Vocational career paths of graduate entry medical students at Flinders University: a comparison of rural, remote and tertiary tracks. Med J Aust 2008; 188: 177-178. <MJA full text>





Abstract
The two rural workforce strategies of rural clinical schools and deployment of international medical graduates (IMGs) geographically overlap in Australia’s large expanse of under-served rural and remote areas.
We used the Rural Clinical School of Western Australia (RCSWA) as a model to examine the relative numbers of IMG clinical academics, and the contribution of IMGs to rural clinical school development and education.
IMGs have established six of 10 rural clinical school sites, maintained an academic presence, and continue to staff the RCSWA in high proportions.
In a fragile rural work ecology, WA’s IMGs are contributing to both meeting current workforce needs and the education of future rural doctors.
The “double debt” Australia owes to IMGs, stemming from the rich cross-fertilisation of these two workforce strategies, should be acknowledged.