The association between smoking and lung cancer is now an accepted fact. Every day, doctors base management decisions on cardiovascular risk calculated using the Framingham equation. It is because of such findings and practical implications that the British doctors study and the Framingham Heart Study from the United States are among the world’s best known longitudinal studies. The stories of these landmark studies in the fields of epidemiology and public health have already been told;1,2 but longitudinal researchers have also been at work in Australia, with implications for our particular population and the wider world. We selected just a few of these (Box 1) — studies that have already demonstrated some longevity and which we judged would be of particular interest to our readership — and interviewed some of their key investigators. What are their stories? How will they make their mark in medicine?
 The Australian Diabetes, Obesity and Lifestyle Study (AusDiab)
The Australian Diabetes, Obesity and Lifestyle Study (AusDiab)“How many Australians suffer from diabetes? How many new cases are diagnosed annually? ... How many people have complications of diabetes that are threatening to their vision or even to their life? ... These are not questions from ‘Trivial Pursuit’ nor is the answer to each of these questions readily available”, wrote Professor Paul Zimmet in the Medical Journal of Australia in 1985.3 At that time, Zimmet was frustrated that there had been little research into the growing problem of diabetes in Australia. Even Papua New Guinea, then one of the poorest countries in the world, had better diabetes data.
Zimmet’s involvement in the epidemiology of diabetes had begun a decade earlier when, in 1975, he had gained funding from the US National Institutes of Health (NIH) to conduct a diabetes prevalence survey on Nauru, a Central Pacific island. The President of Nauru, Hammer DeRoburt, had invited Pincus Taft — his Australian physician and a colleague of Zimmet’s — to the island because he thought diabetes was a problem on Nauru; he was right! Zimmet and Taft’s survey found the highest prevalence of diabetes in the world — about a third of the adult population were affected.4 With further NIH funding, Zimmet and his team were able to survey other Pacific countries and Mauritius, and also, in 1985, to set up the International Diabetes Institute (IDI) in Melbourne as a World Health Organization collaborating centre for the epidemiology of diabetes. “It was really that NIH funding which allowed me to create the institute and establish the framework and the infrastructure that was then able to do AusDiab”, said Zimmet.
In the initial cohort, 11 247 people attended the biomedical examination. The most alarming finding was that almost a million Australian adults had diabetes — equating to 7.4% of the adult population and a 300% increase since 1981.5 A further 16.3% had pre-diabetes, and there was a 60% prevalence of overweight and obesity and a high prevalence of untreated hypertension.
 Bettering the Evaluation And Care of Health (BEACH)
Bettering the Evaluation And Care of Health (BEACH)Each year in Australia, more than 100 million general practice services are provided to about 85% of the population — to the tune of about $4 billion in Medicare payments.6 What really happens in these consultations? What is being diagnosed? In whom? And how is it being treated? Although Medicare statistics can provide some information about general practice services, it is data from the Bettering the Evaluation And Care of Health (BEACH) program that have been able to inform health care policy and clinical practice by answering these questions.
The BEACH program has provided independent data about a range of often controversial topics, including consultation length, payment structures, doctors’ prescribing practices, and adverse drug events, to various stakeholders, including researchers, educators, government departments and agencies, pharmaceutical companies and health care professional organisations. The program has produced 23 books (freely available for download from the BEACH website) and about 100 articles published in recognised journals. Most recently, the group has reported on the prevalence and patterns of chronic disease in Australia, finding that one in four Australians suffer from two or more chronic conditions.7
In 1990, the team successfully secured funding from the National Health and Medical Research Council (NHMRC) and the General Practice Evaluation Program for the first national study of general practice for more than two decades, and for a comparative study of rural and metropolitan general practice. These studies were reported in supplements to the MJA. Thanks to their distinctive covers, they became known as the purple report (Morbidity and treatment in general practice in Australia 1990–1991) and the green report (A comparison of country and metropolitan general practice).8,9
Since the launch of BEACH, funding has remained mixed and uncertain, being renegotiated with all involved parties on an annual or biennial basis. In 2004, the government contribution to funding was withdrawn and, in 2006, there was a real concern that the program would be forced to close. However, this fear was not realised, as the government’s contribution to the program was re-established in mid 2007.6
 The Blue Mountains Eye Study (BMES)
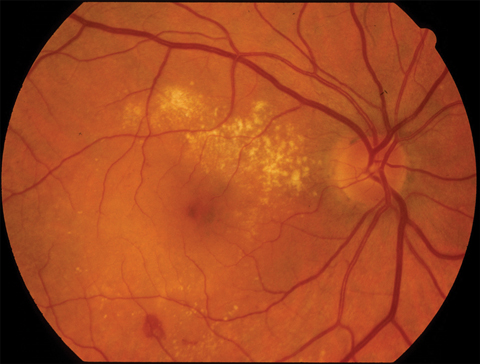
The Blue Mountains Eye Study (BMES)When asked about the study’s highlights, Mitchell nominates the finding that visual impairment has an impact on quality of life that is similar to that from most major systemic conditions, and doubles the need for earlier institutionalised care; it is also associated with about an 80% risk of increased mortality. Further, the BMES was among the first studies in the world to demonstrate the link between smoking and blindness (now a warning on cigarette packets sold in Australia and elsewhere) (Box 2).10 Among the most important of more than 300 papers published from the study, Mitchell includes a New England Journal of Medicine report of the link between using inhaled steroids and developing cataracts.11
 The Busselton Health Study
The Busselton Health StudyFor more than 40 years, and persisting beyond Dr Cullen’s death in 1994, the study’s dedication to the people of Busselton, a picturesque coastal town in the south-west of Western Australia (Box 3), has been returned in kind. This has not only been in terms of study participation, but also in enthusiastic ongoing support, fund-raising and volunteering. As an example — at one time, the local milkman was delivering bottles of glucose solution for the recipients to drink before blood testing for diabetes on the same day.12
The earliest descriptive reports in Australia of the prevalence of common diseases including asthma and other lung problems (the study has always had an emphasis on respiratory disease), diabetes and coronary heart disease are those from the “population laboratory” of Busselton. Numerous papers have been published: interviewees Professor Bill Musk, Associate Professor Alan James and Dr Digby Cullen (son of Kevin) nominated research describing the decline in lung function related to asthma and cigarette smoking,13 and genetic studies into asthma14,15 and haemochromatosis16 as their recent favourites.
 The Dubbo Study
The Dubbo Study
 Tasmanian Longitudinal Health Study (TAHS)
Tasmanian Longitudinal Health Study (TAHS)The TAHS researchers say their most cited article to date is one published in the BMJ in 1994. It reported that only one in four probands who had asthma in childhood continued to have asthma at age 32, and that one in 10 probands who didn’t have asthma as a child developed it later on.19 Among more recent interesting findings, the TAHS found that, for girls, being overweight at 7 years of age triples the risk of developing adult-onset asthma.20
What would you do if you could see an accident waiting to happen that would hasten the deaths of hundreds of people? In 1948, Dr (later, Professor) Eric Saint, who had emigrated from the United Kingdom to Australia, was horrified by dust levels in the crocidolite (blue asbestos) mine and mill at Wittenoom in the Pilbara region of Western Australia, more than 1000 km north of Perth (Box 4). Saint wrote to the head of the WA Health Department advising that the mine would produce the greatest crop of asbestosis the world had ever seen. Unfortunately, responsibility for any decision to halt mining in the area rested with the Department of Mines, and the Health Department could only stand on the sidelines in frustration.
Tragically, in time it became clear that there was another even more lethal health risk to the workers and residents of Wittenoom. The first Wittenoom-related case of mesothelioma was diagnosed in 1960,21 shortly after the initial suggestion of a link between exposure to crocidolite and mesothelioma.22 However, the Wittenoom mine continued to operate until 1966 when, ironically, it was closed for economic rather than health reasons. The mine may have been losing money then; today, the loss in life continues.
 Women’s Health Australia (WHA)
Women’s Health Australia (WHA)More than 41 000 women (14 792 young women, 14 200 middle-aged women and 12 624 older women) responded to the baseline surveys in 1996;23 and now, about 10 000 completed questionnaires are received each year. Over time, themes explored have included health-related behaviour (eg, diet and exercise), time use (eg, paid and unpaid work, and leisure), life stages and key events (eg, childbirth, divorce and widowhood), violence against women, and chronic disease.
Because WHA does not focus on a specific exposure, disease outcome or social problem, publications are highly diverse (http://www.alswh.org.au/public.html). Dobson said, “We’re contributing to the story of the health of Australian women”. There is sustained work on overweight, obesity and physical activity, and in the unfashionable area of incontinence. Professor Julie Byles said, “We’re dispelling the myth that incontinence is just a condition for older people”. WHA is also one of the significant studies of ageing in Australia. In addition, there are add-on studies and collaborations.
Whatever the lifespan of their own study turns out to be, most of the researchers want a future that is better for all longitudinal study investigators. WHA has published a practical guide to conducting longitudinal studies — how to store data, track people, manage collaborators and more.24 Dharmage (TAHS) dreams of establishing a supportive collaboration of longitudinal researchers, all helping each other forward.
1 On our selection: characteristics of some Australian longitudinal studies
The Australian Diabetes, Obesity and Lifestyle Study (AusDiab) |
|||||||||||||||
http://www.sph.uwa.edu.au/go/research-programs/oee/schools-and-centres/schools/school-of-population-health/projects#asb |
|||||||||||||||
2 Macular degeneration
 |
|
Neovascular macular degeneration in the right eye of a 71-year-old woman who smoked heavily. |
Received 12 October 2008, accepted 2 November 2008
- 1. Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ 2004; 328: 1519-1528.
- 2. Richmond C. Thomas Royle Dawber [obituary]. BMJ 2006; 332: 122.
- 3. Zimmet P. Deficient diabetes data [editorial]. Med J Aust 1985; 143: 431-432.
- 4. Zimmet P, Taft P, Guinea A, et al. The high prevalence of diabetes mellitus on a Central Pacific Island. Diabetologia 1977; 13: 111-115.
- 5. Cameron AJ, Welborn TA, Zimmet PZ, et al. Overweight and obesity in Australia: the 1999–2000 Australian Diabetes, Obesity and Lifestyle Study (AusDiab). Med J Aust 2003; 178: 427-432. <MJA full text>
- 6. Russell L, Leeder SR. The Bettering the Evaluation and Care of Health (BEACH) program may be left high and dry [editorial]. Med J Aust 2007; 187: 429-430. <MJA full text>
- 7. Britt HC, Harrison CM, Miller GC, Knox SA. Prevalence and patterns of multimorbidity in Australia. Med J Aust 2008; 189: 72-77. <MJA full text>
- 8. Bridges-Webb C, Britt H, Miles DA, et al. Morbidity and treatment in general practice in Australia 1990–1991. Med J Aust 1992; 157 (8 Suppl): S1-S56.
- 9. Britt H, Miles DA, Bridges-Webb C, et al. A comparison of country and metropolitan general practice. Med J Aust 1993; 159 (9 Suppl): S9-S64.
- 10. Mitchell P, Chapman S, Smith W. “Smoking is major cause of blindness” [editorial]. Med J Aust 1999; 171: 173-174. <MJA full text>
- 11. Cumming RG, Mitchell P, Leeder SR. Use of inhaled corticosteroids and the risk of cataracts. N Engl J Med 1997; 337: 8-14.
- 12. Leeder SR. Preface. In: Welborn TA, editor. The Busselton study: mapping population health. Sydney: Australian Medical Publishing Co, 1998.
- 13. James AL, Palmer LJ, Kicic E, et al. Decline in lung function in the Busselton Health Study: the effects of asthma and cigarette smoking. Am J Respir Crit Care Med 2005; 171: 109-114.
- 14. Daniels SE, Bhattacharrya S, James A, et al. A genome-wide search for quantitative trait loci underlying asthma. Nature 1996; 383: 247-250.
- 15. Hui J, Oka A, James A, et al. A genome-wide association scan for asthma in a general Australian population. Hum Genet 2008; 123: 297-306.
- 16. Olynyk JK, Cullen DJ, Aquilia S, et al. A population-based study of the clinical expression of the hemochromatosis gene. N Engl J Med 1999; 341: 718-724.
- 17. Simons LA, Simons J, Friedlander Y, McCallum J. Usefulness of fasting plasma glucose to predict mortality or coronary heart disease in persons ≥ 60 years of age without diabetes mellitus or in those with undiagnosed diabetes mellitus (from the Dubbo Study). Am J Cardiol 2008; 102: 831-834.
- 18. Simons LA, Simons J, McCallum J, Friedlander Y. Lifestyle factors and risk of dementia: Dubbo Study of the elderly. Med J Aust 2006; 184: 68-70. <MJA full text>
- 19. Jenkins MA, Hopper JL, Bowes G, et al. Factors in childhood as predictors of asthma in adult life. BMJ 1994; 309: 90-93.
- 20. Burgess JA, Walters EH, Byrnes GB, et al. Childhood adiposity predicts adult-onset current asthma in females: a 25-yr prospective study. Eur Respir J 2007; 29: 668-675.
- 21. McNulty JC. Malignant pleural mesothelioma in an asbestos worker. Med J Aust 1962; 49: 953-954.
- 22. Wagner JC, Sleggs CA, Marchand P. Diffuse pleural mesothelioma and asbestos exposure in the North Western Cape Province. Br J Ind Med 1960; 17: 260-271.
- 23. Lee C, Dobson AJ, Brown WJ, et al. Cohort profile: the Australian Longitudinal Study on Women’s Health. Int J Epidemiol 2005; 34: 987-991.
- 24. Loxton D, Byles J, Dobson A, Brown W, editors. Conducting longitudinal research: practical lessons from the Australian Longitudinal Study on Women’s Health. Int J Multiple Research Approaches 2007; 1 (2).







We thank all the interviewees for their time and willing participation.
None identified.