A 2-year-old boy and a 10-year-old girl presented to the emergency department with a decreased level of consciousness. The girl had had persistent vomiting and a seizure. Urine metabolic screening tests were positive for γ-hydroxybutyrate (GHB). Samples from toy beads ingested by both children contained 1,4-butanediol, which is metabolised to GHB in humans. Regulatory authorities were notified, leading to an international recall of the toy beads.
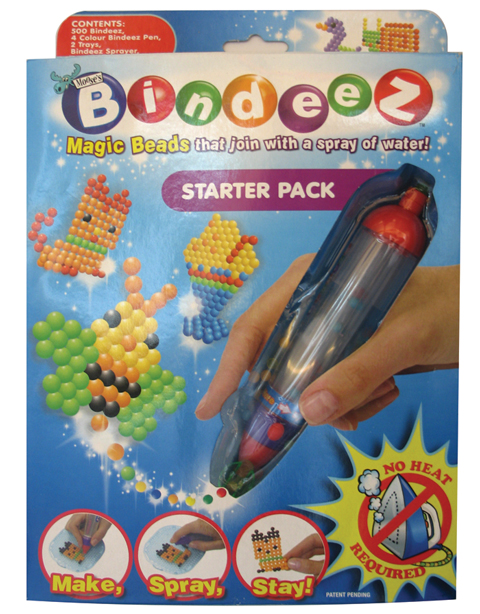
Seven hours after presentation, remarkable clinical improvement was noted, and he became fully alert and cooperative. At this point he vomited and also passed a substantial number of coloured beads in his stool. The family were further questioned about a history of ingestion; the boy’s mother divulged that he had been playing with Bindeez brand toy beads (Moose Enterprise, Melbourne, Vic) (Box).
GHB is an endogenously occurring neurotransmitter derived from γ-amino butyric acid (GABA).1 Its known metabolic precursors are 1,4-BD and γ-butyrolactone. A potent sedative and anaesthetic agent, it was initially synthesised in the 1960s.2 GHB and its precursors have recently found notoriety as recreational and club drugs. In 2000, GHB became a banned substance by the United States Drug Enforcement Agency and classified as Schedule 1 by the US Food and Drug Administration.2,3
1,4-BD is a widely available industrial chemical used as a solvent and in the manufacture of some types of plastics and fibres. When ingested, it is metabolised rapidly by alcohol and aldehyde dehydrogenases to GHB.4,5 Hence, the toxicity and clinical features of 1,4-BD poisoning are similar to those of GHB. While 1,4-BD is not a scheduled drug in Australia, it is a category 1 precursor under the Drug Misuse and Trafficking Regulations 2006, which restrict the supply of 1,4-BD (Pharmaceutical Services, NSW Department of Health, personal communication, 12 Nov 2007).
GHB is an agonist at inhibitory GABAB receptors and is excitatory at specific GHB receptors. There is a dose–response relationship in GHB toxicity. Low doses result in vomiting, drowsiness, visual disturbance and disinhibition, while higher-dose effects include confusion, coma, bradycardia and myoclonic (seizure-like) movements.3 Routine urine toxicology screens do not detect GHB in their profile. Specific analysis with gas chromatography–mass spectrometry (GC–MS) or as part of a urine metabolic screen is required. The urine sample from Patient 1 was investigated for possible inherited metabolic diseases, including urinary organic acid analysis by GC–MS.6 This showed a marked increase in GHB (a metabolite seen in succinic semialdehyde dehydrogenase deficiency) but without any increase in 4,5-dihydroxyhexanoate lactone, as would be expected in the inborn error. This pattern strongly suggested an exogenous source of GHB, which was confirmed by the compound being undetectable in a second urine sample taken 3 days later.
Treatment of GHB poisoning is primarily supportive and may involve airway and ventilatory intervention, and atropine for symptomatic bradycardia7 Gastrointestinal decontamination with activated charcoal is not indicated, owing to the rapid absorption of this liquid poison. Additionally, there are no specific antidotes that reliably reverse GHB toxicity.7
The identification of these cases highlights the important role of poisons centres in toxicovigilance and monitoring of potential clusters of poisoning related to new pharmaceuticals and chemical agents. Rapid electronic communication of these cases to worldwide toxicological networks enables health authorities to make a risk assessment of similar toy products overseas. So far, this has resulted in identification of similar suspected cases of GHB poisoning in children and an international withdrawal of the product. Chinese authorities confirmed that toy beads from the Hong Kong manufacturer contained a substance which metabolised to GHB.8
- 1. Quang LS, Levy HL, Law T, et al. Laboratory diagnosis of 1,4-BD and GHB overdose by routine urine organic acid analysis. Clin Toxicol (Phila) 2005; 43: 321-323.
- 2. Strickland RM, Felgate P, Caldicott DGE. Survival of massive γ-hydroxybutyrate/1,4-butanediol overdose. Emerg Med Australas 2005; 17: 281-283.
- 3. Wong CGT, Chan KFY, Gibson KM, Snead OC III. γ-Hydroxybutyric acid — neurobiology and toxicology of a recreational drug. Toxicol Rev 2004; 23: 3-20.
- 4. Zvosec DL, Smith SW, McCutcheon JR, et al. Adverse events, including death, associated with the use of 1,4-butanediol. N Engl J Med, 2001; 344: 87-94.
- 5. Lora-Tamayo C, Tena T, Rodriguez A, et al. Intoxication due to 1,4-butanediol. Forensic Sci Int 2003; 133: 256-259.
- 6. Tanaka K, West-Dull A, Hine DG, et al. Gas-chromatographic method of analysis for urinary organic acids. II. Description of the procedure, and its application to diagnosis of patients with organic acidurias. Clin Chem 1980; 26: 1847-1853.
- 7. Shannon MW, Quang LS. Gamma-hydroxybutyrate, gamma-butyrolactone, and 1,4-butanediol: a case report and review of the literature. Pediatr Emerg Care 2000; 16: 435-440.
- 8. China says Bindeez has toxic substances. Sydney Morning Herald 2007; 11 Nov. http://www.smh.com.au/news/World/China-says-Bindeez-has-toxic-substances/2007/11/11/1194716047932.html (accessed Nov 2007).





We would like to thank Dr Maurice Gett (Paediatrician), Dr Holly Smith (Emergency Fellow) and others who looked after the patients.
None identified.