We report eight cases of Chikungunya virus infection in travellers to Australia between February 2006 and September 2007. As clinicians became aware of the Indian Ocean epidemic, unwell travellers returning from affected countries were tested for Chikungunya virus. Before this epidemic, only one case of Chikungunya virus infection had been reported in Australia; this involved importation of the virus from Indonesia to Darwin in 1989.1
The eight cases of Chikungunya virus infection were identified after reviewing the database of the Victorian Infectious Diseases Reference Laboratory between February 2006 and September 2007. The review was undertaken to raise awareness among medical practitioners of Chikungunya virus infection. Chikungunya virus was diagnosed by performing a generic alphavirus reverse transcriptase polymerase chain reaction (RT-PCR) on serum.2 The diagnosis was confirmed in all eight patients by sequencing the alphavirus RNA product.
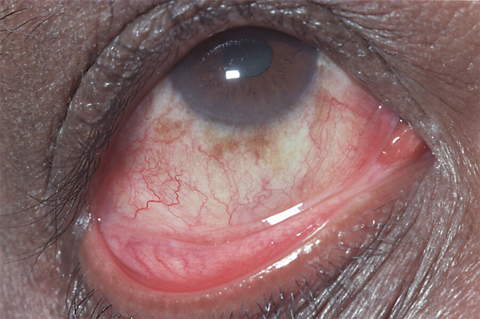
The first patient diagnosed with Chikungunya virus infection was a 59-year-old Mauritian man who presented to hospital 5 days after travelling from Mauritius for the 2006 Commonwealth Games. He reported a 2-day history of fevers, rigors, and headaches with associated arthralgia, conjunctivitis (Box 1), and left lower limb erythema. Investigations revealed leukopenia, thrombocytopenia, and mildly abnormal liver function tests. Blood taken at admission was positive for alphavirus RT-PCR, and sequencing confirmed Chikungunya virus. The patient received supportive treatment and had fully recovered on review 1 week later. A detailed description of his illness has been reported previously.2
Six subsequent patients had travelled from Sri Lanka, and the most recent patient travelled from India in June 2007 (Box 2). All patients described fevers, rigors and headaches. Six patients presented with arthralgia, five with rash, and two had conjunctivitis. Investigations revealed six patients had leukopenia, three had thrombocytopenia, and three patients had abnormal liver function tests with raised serum alanine aminotransferase levels. All patients recovered. Clinician awareness of the outbreak resulted in early diagnosis for all eight patients.
These eight patients illustrate the typical clinical presentation of Chikungunya virus infection. The illness is of abrupt onset, characterised by high fevers accompanied by rigors, arthralgia or arthritis, myalgia and headache. A maculopapular rash occurs on the second to fifth day in 50% of patients. The incubation period ranges from 2 to 12 days, and the febrile period lasts typically 3–7 days. Patients generally make a full recovery. Patients may experience persistent joint symptoms. Serious complications are rare. Neuroinvasive disease (encephalitis) and deaths have been reported during the outbreak in Réunion.3 Laboratory tests reveal a mild leukopenia and relative lymphocytosis. No specific drug therapy is available, and treatment is supportive. Chikungunya virus infection is believed to confer lifelong immunity. No licensed Chikungunya virus vaccine is currently available.4,5
Laboratory diagnosis in these patients was by detecting viral RNA by RT-PCR. The viraemic phase of alphaviruses is 2–8 days, so the success of RT-PCR to detect the virus depends on early presentation and the clinical suspicion of a possible alphavirus infection.6 Diagnosis of Chikungunya virus infection may be made serologically at major virology reference laboratories (Westmead Hospital, Sydney, NSW; PathWest Laboratory Medicine WA, Perth, WA; and Queensland Health Scientific Services, Brisbane, QLD).
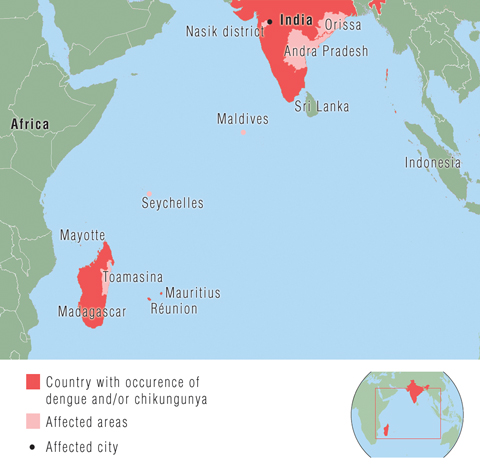
Chikungunya virus is an arthropod-borne alphavirus classified within the family Togaviridae. It is geographically distributed in Africa, India, and South-East Asia, and periodic outbreaks have been described in the past 50 years.7 The most recent epidemic began in Kenya in 2004. By early 2005, there was an outbreak in the Comoro Islands, which promptly spread to other Indian Ocean islands: Réunion, Mauritius, Seychelles and Madagascar (Box 3).4,8 As of September 2006, Réunion had an estimated 266 000 cases, including a reported 248 deaths (population, 770 000).3 The epidemic subsequently spread to India, Sri Lanka, the Maldives and Malaysia, with reports of imported cases in Europe, the United States, and Hong Kong.5,9-11 The outbreak is ongoing in India, with an estimated 1.4 million cases reported and attack rates as high as 45%.4,12-14
In August 2007, an outbreak of Chikungunya virus infection occurred in the Ravenna district in Italy. As of 13 September 2007, 254 cases had been reported. The first case was attributed to a traveller from India. This outbreak demonstrates the vulnerability of receptive countries to Chikungunya virus emergence. The mosquito vector, Aedes albopictus, is present in at least 12 European countries.15
This infection has potential implications for Australia. An outbreak similar to that seen in Italy could occur in Australia, and medical practitioners should consider the possibility of local transmission of Chikungunya virus from an infected patient if imported disease occurs. They should take measures to minimise that risk, particularly if a viraemic patient is at risk of being bitten by mosquitoes. Mosquitoes are the vector for Chikungunya virus, and humans are the major reservoir during epidemics. The mosquito Aedes aegypti has been the major vector in India, Asia and Africa, and A. albopictus is the likely vector in Réunion and Italy.4,15,16 Chikungunya virus may also be spread by other mosquitoes of the genera Aedes and Culex.7 The known vectors are present in Australia — A. aegypti is found in northern Queensland and A. albopictus has been recovered at ports around Australia,17,18 so it may be of particular importance that infected travellers be diagnosed promptly in these locations and isolated from mosquito exposure early in their illness. No local transmission has yet been reported in Australia.
- Douglas F Johnson1
- Julian D Druce2
- Scott Chapman3
- Ashwin Swaminathan1
- Josh Wolf4
- Jack S Richards5
- Tony Korman3
- Chris Birch2
- Michael J Richards5
- 1 Austin Hospital, Melbourne, VIC.
- 2 Victorian Infectious Diseases Reference Laboratory, Melbourne, VIC.
- 3 Monash Medical Centre, Melbourne, VIC.
- 4 Royal Children’s Hospital, Melbourne, VIC.
- 5 Royal Melbourne Hospital, Melbourne, VIC.
None identified.
- 1. Harnett GB, Bucens MR. Isolation of Chikungunya virus in Australia. Med J Aust 1990; 152: 328-329.
- 2. Druce JD, Johnson DF, Tran T, et al. Chikungunya virus infection in traveler to Australia. Emerg Infect Dis 2007; 13: 509-510.
- 3. International Society for Infectious Diseases. Chikungunya — Indian Ocean update (32). ProMED-mail 2006; 14 Oct. Archive number 20061014.2953. http://www.promedmail.org (accessed Oct 2007).
- 4. Pialoux G, Gauzere B, Jaureguiberry S, Strobel M. Chikungunya, an epidemic arbovirus. Lancet Infect Dis 2007; 7: 319-327.
- 5. Centers for Disease Control and Prevention. Chikungunya fever diagnosed among international travellers — United States, 2005–2006. MMWR Morb Mortal Wkly Rep 2006; 55: 1040-1042.
- 6. Lee N, Wong CK, Lam WY, et al. Chikungunya fever, Hong Kong [letter]. Emerg Infect Dis 2006; 12: 1790-1792.
- 7. Berger SA, Calisher CH, Keystone JS. Chikungunya virus infection. In: Exotic viral diseases: a global guide. London: BC Decker, 2003: 48-51.
- 8. Charrel R, de Lamballerie X, Raoult D. Chikungunya outbreaks — the globalization of vectorborne diseases. N Engl J Med 2007; 356: 769-771.
- 9. Bodenmann P. Chikungunya: an epidemic in real time. Lancet 2006; 368: 258.
- 10. International Society for Infectious Diseases. Chikungunya — Indian Ocean update (17): spread to France. ProMED-mail 2006; 21 Apr. Archive number 20060421.1166. http://www.promedmail.org (accessed Oct 2007).
- 11. International Society for Infectious Diseases. Chikungunya — Indian Ocean update (33): Maldives. ProMED-mail 2006; 24 Dec. Archive number 20061224.3598. http://www.promedmail.org (accessed Oct 2007).
- 12. International Society for Infectious Diseases. Chikungunya — Indian Ocean (06): Sri Lanka, India, Islands. ProMED-mail 2007; 20 Mar. Archive number 20070320.0974. http://www.promedmail.org (accessed Oct 2007).
- 13. International Society for Infectious Diseases. Chikungunya – Indian Ocean update (12): India (Delhi). ProMED-mail 2007; 13 Jun. Archive number 20070613.1935. http://www.promedmail.org (accessed Oct 2007).
- 14. World Health Organization. Chikungunya in India. 2006; 17 Oct. http://www.who.int/csr/don/2006_10_17/en/index.html (accessed Oct 2007).
- 15. International Society for Infectious Diseases. Chikungunya — Italy (Emilia Romagna) (06). ProMED-mail 2007; 21 Sep. Archive number 20070921.3134. http://www.promedmail.org (accessed Oct 2007).
- 16. Yergolkar P, Tandale B, Arankalle V, et al. Chikungunya outbreaks caused by African genotype, India. Emerg Infect Dis 2006; 12: 1580-1583.
- 17. Russell RC, Williams CR, Sutherst RW, Ritchie SA. Aedes (Stegomyia) albopictus — a dengue threat for southern Australia? Commun Dis Intell 2005; 29: 296-298.
- 18. Beebe N, Whelan P, van der Hurk A, et al. Genetic diversity of the dengue vector Aedes aegypti in Australia and implications for future surveillance and mainland incursion monitoring. Commun Dis Intell 2005; 29: 299-304.





Abstract
We report eight recent cases of Chikungunya virus infection in travellers to Australia. Patients presented with fevers, rigors, headaches, arthralgia, and rash.
The current Indian Ocean epidemic and Italian outbreak have featured prominently on Internet infectious disease bulletins, and Chikungunya virus infection had been anticipated in travellers from the outbreak areas.
Diagnosis was by a generic alphavirus reverse transcriptase polymerase chain reaction with confirmatory sequencing.
Prompt diagnosis of Chikungunya virus infections is of public health significance as the mosquito vectors for transmission exist in Australia. There is potential for this infection to spread in the largely naïve Australian population.