Last year marked the 10-year anniversary of the widespread use of highly active antiretroviral therapy (HAART) for treating HIV infection. HAART — a combination of three antiretrovirals (ARVs) from at least two drug classes1,2 — has led to significant reductions in HIV-related morbidity and mortality and is a highly cost-effective medical intervention.3-7 The goal of combination ARV therapy is firstly to suppress HIV viral load in plasma to below the limit of detection and secondly to restore immune function, as demonstrated by an increased number of CD4+ T cells.
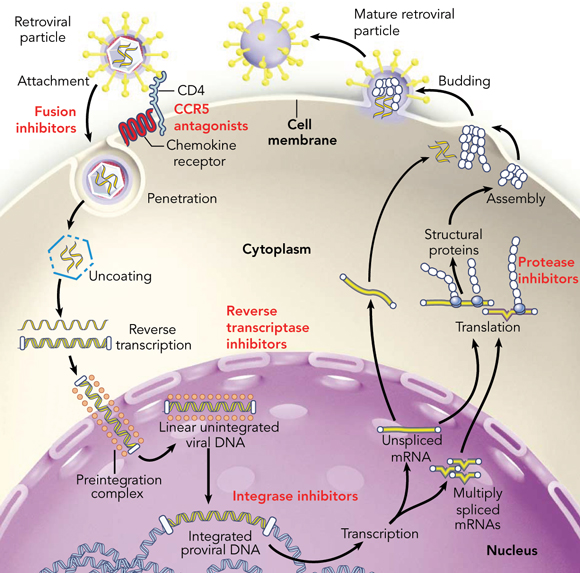
To understand how ARVs work, a limited understanding of the HIV life cycle is required. HIV is an RNA virus that primarily infects CD4+ T lymphocytes. After attachment and binding to the CD4 receptor and specific chemokine co-receptors (primarily CCR5 and/or CXCR4), the virus and host cell membranes fuse and HIV RNA enters the target cell. The HIV RNA undergoes reverse transcription from RNA to DNA and is then transported into the nucleus to integrate with the host DNA. Multiple copies of full-length and spliced HIV RNA are made and exported from the nucleus. Viral proteins are processed by the protease enzyme and, together with full-length HIV RNA, are packaged at the cell surface and viral particles are released (Box 1).
E1–E4 denote evidence levels I–IV of the National Health and Medical Research Council (thus E1 = I; E2 = II; E3 = III; E31 = III-1; etc).10
Zidovudine (AZT) is the oldest ARV and is still frequently used.8 Its major toxic effects include bone marrow suppression, gastrointestinal upset and headache. On full blood examination, macrocytosis is almost universal. Zidovudine penetrates the central nervous system and has shown efficacy in settings such as prevention of intrapartum mother-to-child transmission (E2),9 HIV-related thrombocytopenia,11-13 AIDS dementia complex14 and post-exposure prophylaxis.15
Lamivudine (3TC) has activity against both HIV and hepatitis B virus (HBV), with few side effects. Used alone, HIV resistance to lamivudine emerges within weeks. HBV also acquires resistance to lamivudine — at a greater frequency in HIV–HBV co-infected individuals than in HBV-mono-infected individuals.16
Abacavir (ABC) is a well tolerated NRTI with low affinity for human mitochondrial DNA polymerase γ.17 A hypersensitivity reaction is seen in 5% of patients. The reaction commonly occurs within 6 weeks of drug commencement and manifests with fever, rash, gastrointestinal, and respiratory symptoms. In the event of hypersensitivity, rechallenge with abacavir is absolutely contraindicated due to risk of anaphylaxis and death (E4).18,19 This hypersensitivity syndrome is strongly associated with the HLA-B57 haplotype.20-22 Positive and negative predictive values of HLA-B*5701 screening in a predominantly white Western Australian cohort were 79% and 99%, respectively.22 Therefore, screening for HLA-B*5701 before abacavir use can be cost-effective and reduce morbidity (E32).23,24
Tenofovir (TDF) is a nucleotide NRTI that is also highly effective against HBV, although it is currently not licensed for treatment of HBV in the absence of HIV infection. Tenofovir is well tolerated; nephrotoxicity (reduced creatinine clearance and/or Fanconi syndrome) has been reported and may occur in individuals with pre-existing renal failure, diabetes mellitus and low CD4+ T-cell count (E32).25,26
NRTIs make up an important component of the ARV regimen. Most recommended regimens contain at least two NRTIs combined with an ARV from another class. Triple NRTI combinations are inferior to a combination regimen containing at least two classes of ARVs.27 Current preferred combinations of NRTIs are based largely on efficacy and toxicity and include zidovudine, abacavir or tenofovir plus lamivudine, or emtricitabine plus tenofovir. Most of these drugs are now available as fixed-dose combinations.
Hepatotoxicity and rash can occur with both NNRTIs. Nevirapine-related hepatotoxicity is more common and can be fatal in rare cases.28 Efavirenz-related rash occurs more readily in children.29 NNRTIs are not associated with insulin resistance,30,31 although efavirenz is associated with mild hyper-cholesterolaemia.32,33
Nevirapine strongly induces CYP450 3A4 isoenzymes, while efavirenz is a mixed inducer/inhibitor of the same enzyme. NNRTIs have multiple drug interactions, including the oestrogen-based contraceptive pill (summarised in Box 2). Alternative methods of birth control are recommended if NNRTIs are used.
Efavirenz (EFV) is highly potent, as seen in several randomised trials that compared efavirenz-based combinations with other agents (E1).34 Efavirenz is associated with high rates of central nervous system side effects, such as insomnia, vivid dreams, irritability and, less commonly, psychosis. These generally diminish over the first 2–4 weeks of therapy. Efavirenz is teratogenic (pregnancy class C); therefore all women with childbearing potential should use effective contraception.
Nevirapine (NVP) is associated with rash and hepatotoxicity, with the latter occurring in up to 17% of patients.28 Hepatotoxicity is more common in women, especially those with CD4+ T-cell counts > 250 cells/mL at initiation of therapy (E1).35 All patients suspected of having drug-related rash should be assessed for hepatotoxicity as the two may occur simultaneously. Single-dose nevirapine is highly effective in prevention of intrapartum mother-to-child transmission (E2),36 although development of resistance is frequent.37 Second generation NNRTIs with activity against HIV resistant to nevirapine or efavirenz (etravirine, [TMC 125]) are under evaluation and now available through the Special Access Scheme.38
Efavirenz and nevirapine are equally effective, but differences in toxicity profile and potential for drug interaction lead to preferential use in particular settings (E2).32 Efavirenz should be avoided in patients with a history of severe psychiatric illness. Nevirapine is the drug of choice for women of childbearing potential or during pregnancy, but is avoided in patients taking antimycobacterial agents concurrently due to the risks of hepatotoxicity.
The use of both nevirapine and efavirenz in the same regimen has not been shown to have additional efficacy over the use of either agent alone, and causes more adverse events than each drug separately (E2).32 Therefore, this approach is not recommended.
PIs prevent cleavage of viral precursor proteins into the subunits required for the formation of new virions (see Box 1). PIs block the production of virus from infected cells. Older PI-containing regimens are used less frequently now because of inconvenient dosing, food restrictions (indinavir, nelfinavir), and large pill burdens (amprenavir, saquinavir). PIs have extensive interactions with the CYP450 system (Box 2). Ritonavir, even at a low dose, is a potent inhibitor of the CYP450 3A4 isoenzymes. Low-dose ritonavir (usually 100 mg) together with a second PI is referred to as a “boosted PI” regimen, and this regimen is generally preferred to the use of a PI without ritonavir boosting. Low-dose ritonavir will inhibit metabolism of the second PI leading to an increase in serum levels and the need for less frequent dosing of the second PI. Newer PIs and ritonavir “boosted” PI regimens have improved pharmacokinetics, reduced pill burden, and a higher barrier to the development of ARV resistance.
Atazanavir offers the advantage of once-daily dosing and is associated with less diarrhoea, dyslipidaemia and insulin resistance than other PIs. Dose-dependent asymptomatic hyperbili-rubinaemia is commonly observed. Comparison of an “un-boosted” atazanavir regimen with an efavirenz-based combination showed similar antiviral efficacy (E2).39 Co-administration with macrolides may lead to prolongation of the QTc interval.
Enfuvirtide (T20) prevents fusion of the HIV viral membrane with the target cell membrane and therefore blocks HIV entry into CD4+ T cells. Enfuvirtide is not orally bioavailable and requires reconstitution before subcutaneous injection. Injection site reactions are common. Randomised trials of enfuvirtide in individuals with multidrug resistant HIV have shown that addition of enfuvirtide to an “optimised” ARV regimen including at least another active agent leads to significant virological and immunological improvement (E2).40 Enfuvirtide is not licensed for use in treatment-naïve patients.
This exciting new class of ARVs irreversibly inhibit the integration of HIV DNA into the host genome. Some agents have shown high potency in both treatment-naïve and treatment-experienced patients. An agent in this class has recently become available for use in patients with multidrug resistant HIV and advanced immuno-deficiency via the Special Access Scheme.38
Several international bodies publish guidelines for the use of antiretroviral therapy. The rapid changes in available agents, descriptions of new adverse events, and information on resistance and treatment strategies require that recommendations in guidelines are frequently updated. For this reason, Australia does not publish its own guidelines, but a set of extensive commentaries on the United States Department of Health and Human Services (US DHHS) guidelines provides information and guidance on Austra-lian specific scenarios. Both US DHHS guidelines and the Austra-lian commentaries are updated 6 monthly (http://www.ashm.org.au/guidelines). (Box 3)
Current recommendations for initial therapy for HIV infection include the use of dual NRTI (AZT/3TC, TDF/FTC, ABC/3TC) with either an NNRTI (efavirenz or nevirapine) or a boosted PI (lopinavir/ritonavir). The selection of a suitable HAART regimen should account for factors such as pill burden, adverse effects, pregnancy potential, co-infection with hepatitis B or C, efficacy, and comorbidities such as renal disease or metabolic syndrome. The management of HIV infection is a complex and rapidly changing arena. Studies have shown better outcomes for patients who receive care from physicians with experience in HIV medicine.41
Lipodystrophy is a syndrome of both increased fat deposition (lipohypertrophy) and subcutaneous fat loss (lipoatrophy).42 Fat accumulation occurs in the dorsal cervical fat pad (buffalo hump), abdominal visceral fat, and breast tissue. Lipoatrophy occurs predominantly in the extremities, resulting in prominence of veins, and loss of bilateral buccal fat pads. Both NRTIs and PIs have been associated with lipodystrophy, which can occur with or without dyslipidaemia. The risk of lipodystrophy increases with prolonged ARV exposure (E4).43 Switching to a non-PI regimen is associated with reduction in visceral fat deposition (E32).44 Switching the thymidine analogue (stavudine or zidovudine) to an abacavir- or tenofovir-based regimen is associated with a slow increase in peripheral subcutaneous fat.45,46
Dyslipidaemia can result from ARV administration. Regular monitoring is required and lipid-lowering agents are often indicated. The metabolic syndrome, type 2 diabetes and vascular events are also complications of ARVs. An association between PI exposure and risk for increased cardiovascular events is well established (E2).30,31 The link (although weaker) has also been demonstrated with NRTIs and NNRTIs. New ARV drugs with less effect on lipids and insulin resistance are under development.
Adherence is a critical component to the success of HAART. There is good evidence that sustained virological response is strongly correlated with drug adherence (E1).47 Greater than 95% adherence is required to achieve viral suppression in 80% of individuals using PIs,48 although the adherence requirement may be less rigorous for NNRTIs than PIs.49
Education regarding potential drug interactions is important. Many ARVs inhibit, induce or are substrates for the CYP450 system, and undesirable pharmacokinetic interactions not uncommonly result (Box 2). Drug–drug interactions may occur between ARVs themselves, leading to reduced antiretroviral activity. Only combinations of ARVs that have undergone formal pharmaco-kinetic evaluation should be used. As the list of drug–drug interactions is extensive, it is recommended that physicians consult a pharmacist or online resources before prescribing medications in individuals receiving ARVs (http://www.hiv-druginteractions.org/).
Numerous strategies have been studied to identify a safe and effective approach to treatment interruptions. A large randomised study showed an increased risk of HIV disease progression and death with intermittent CD4-guided ARV therapy compared with continuous therapy.50 Once treatment is initiated in chronic HIV infection, it is recommended that it be continued without interruption (E2).
Drug resistance rapidly emerges if viral replication is not fully suppressed in the presence of drugs.51 Increased transmission of drug-resistant HIV has been reported in many parts of the developed world,52-54 and expert opinion now recommends resistance testing before initiation of ARV therapy (E32).55 In Australia, viral resistance is measured by sequencing the reverse transcriptase and protease genes to detect mutations that are associated with drug resistance. Use of antiviral susceptibility testing in the management of chronic infection, especially in the setting of a failing regimen, has been shown to improve outcome (E32), and is widely used in Australia.
The choice of ARVs for an HIV-infected individual has substantially increased over the past 10 years. Despite increased ease of administration and reduced toxicity, the management of ARV therapy, particularly in a treatment-experienced patient, is complex. ARV therapy has substantially improved the quality of life for HIV-infected individuals.56-58 Unfortunately, ARVs are not universally available. Many challenges remain in the management of HIV infection: these include enhanced availability of ARVs globally, reduction of side effects and drug resistance, and increased options for treatment-experienced individuals.
2 Effect of protease inhibitors (PIs) and non-nucleoside reverse transcriptase inhibitors (NNRTIs) on hepatic cytochrome P450 (CYP450 3A4) and specific drug–drug interactions*
3 Indications for initiation of combination antiretrovirals*
All patients with a history of an AIDS-defining illness or severe symptoms of HIV infection regardless of CD4+ T-cell count (E1)
Asymptomatic individuals with < 200 CD4+ T cells/mm3 (E1)
Asymptomatic individuals with CD4+ T-cell counts of 200–350 cells/mm3 should be offered treatment (E3)
For asymptomatic individuals with CD4+ T-cell counts of > 350 cells/mm3 and plasma HIV RNA > 100 000 copies/mL, most experienced clinicians defer therapy but some clinicians may consider initiating treatment
Therapy should be deferred for individuals with CD4+ T-cell counts of > 350 cells/mm3 and plasma HIV RNA < 100 000 copies/mL
* As recommended by the Australasian Society for HIV Medicine (ASHM) (http://www.ashm.org.au/aust-guidelines/) and the United States Department of Health and Human Services (AIDSinfo website, http://aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf).
- Luke F Chen1
- Jennifer Hoy1,2
- Sharon R Lewin2
- 1 Infectious Diseases Unit, The Alfred Hospital, Melbourne, VIC.
- 2 Department of Medicine, Monash University, Melbourne, VIC.
Sharon Lewin is supported by a National Health and Medical Research Council Practitioner Fellowship #251651. We acknowledge the helpful comments made by Dr Alan Street.
GlaxoSmithKline provided Luke Chen with travel assistance for the 2005 Annual Meeting of the Australasian Society for HIV Medicine. Jennifer Hoy has a consultancy with Narhex Life Sciences Limited; is a member of the Advisory Boards of Abbott, Bristol–Myers Squibb, Roche and Tibotec; is in receipt of honoraria from Roche, Bristol–Myers Squibb, Boehringer Ingelheim and Tibotec; has received travel grants from Roche, Abbott and Bristol–Myers Squibb; and reimbursement for clinical trial research from the following pharmaceutical companies: Abbott, Avexa, Boehringer Ingelheim, Bristol–Myers Squibb, CSL, Gilead, GlaxoSmithKline, Johnson & Johnson, Merck Sharp & Dohme, Pfizer, Roche, Schering-Plough, and Tibotec. Sharon Lewin has received travel assistance from Boehringer Ingelheim, Roche, Gilead and Abbott to attend meetings.
- 1. Hammer SM, Squires KE, Hughes MD, et al. A controlled trial of two nucleoside analogues plus indinavir in persons with human immunodeficiency virus infection and CD4 cell counts of 200 per cubic millimeter or less. AIDS Clinical Trials Group 320 Study Team. N Engl J Med 1997; 337: 725-733.
- 2. Gulick RM, Mellors JW, Havlir D, et al. Treatment with indinavir, zidovudine, and lamivudine in adults with human immunodeficiency virus infection and prior antiretroviral therapy. N Engl J Med 1997; 337: 734-739.
- 3. Detels R, Munoz A, McFarlane G, et al. Effectiveness of potent antiretroviral therapy on time to AIDS and death in men with known HIV infection duration. Multicenter AIDS Cohort Study Investigators. JAMA 1998; 280: 1497-1503.
- 4. Murphy EL, Collier AC, Kalish LA, et al; Viral Activation Transfusion Study Investigators. Highly active antiretroviral therapy decreases mortality and morbidity in patients with advanced HIV disease. Ann Intern Med 2001; 135: 17-26.
- 5. Sendi PP, Bucher HC, Harr T, et al. Cost effectiveness of highly active antiretroviral therapy in HIV-infected patients. Swiss HIV Cohort Study. AIDS 1999; 13: 1115-1122.
- 6. Moore RD. Cost effectiveness of combination HIV therapy: 3 years later. Pharmacoeconomics 2000; 17: 325-330.
- 7. Beck EJ, Mandalia S, Gaudreault M, et al. The cost-effectiveness of highly active antiretroviral therapy, Canada 1991–2001. AIDS 2004; 18: 2411-2418.
- 8. Fischl MA, Richman DD, Grieco MH, et al. The efficacy of azidothymidine (AZT) in the treatment of patients with AIDS and AIDS-related complex. A double-blind, placebo-controlled trial. N Engl J Med 1987; 317: 185-191.
- 9. Connor EM, Sperling RS, Gelber R, et al. Reduction of maternal-infant transmission of human immunodeficiency virus type 1 with zidovudine treatment. Pediatric AIDS Clinical Trials Group Protocol 076 Study Group. N Engl J Med 1994; 331: 1173-1180.
- 10. National Health and Medical Research Council. A guide to the development, implementation and evaluation of clinical practice guidelines. Canberra: NHMRC, 1999. http://www.nhmrc.gov.au/publications/_files/cp30.pdf (accessed Nov 2006).
- 11. Pottage JC Jr, Benson CA, Spear JB, et al. Treatment of human immunodeficiency virus-related thrombocytopenia with zidovudine. JAMA 1988; 260: 3045-3048.
- 12. The Swiss Group for Clinical Studies on the Acquired Immunodeficiency Syndrome (AIDS). Zidovudine for the treatment of thrombocytopenia associated with human immunodeficiency virus (HIV). A prospective study. Ann Intern Med 1988; 109: 718-721.
- 13. Neil BJ, Johnson GJ, Pomeroy C. Zidovudine therapy for severe human immunodeficiency virus-related thrombocytopenia. Am J Med 1988; 85: 744-745.
- 14. Sidtis JJ, Gatsonis C, Price RW, et al. Zidovudine treatment of the AIDS dementia complex: results of a placebo-controlled trial. AIDS Clinical Trials Group. Ann Neurol 1993; 33: 343-349.
- 15. Cardo DM, Culver DH, Ciesielski CA, et al. A case-control study of HIV seroconversion in health care workers after percutaneous exposure. Centers for Disease Control and Prevention Needlestick Surveillance Group. N Engl J Med 1997; 337: 1485-1490.
- 16. Matthews GV, Bartholomeusz A, Locarnini S, et al. Characteristics of drug resistant HBV in an international collaborative study of HIV-HBV-infected individuals on extended lamivudine therapy. AIDS 2006; 20: 863-870.
- 17. Hammond E, Nolan D, McKinnon EJ, et al. Differential effects of nucleoside reverse transcriptase inhibitor (NRTI) regimens on adipocytes mitochondrial DNA depletion in HIV-infected patients. 6th International Workshop on Adverse Drug Reactions and Lipodystrophy in HIV; 2004 Oct 25–28; Washington, DC, USA. Abstract 16.
- 18. El-Sahly HM. Development of abacavir hypersensitivity reaction after rechallenge in a previously asymptomatic patient. AIDS 2004; 18: 359-360.
- 19. Walensky RP, Goldberg JH, Daily JP. Anaphylaxis after rechallenge with abacavir. AIDS 1999; 13: 999-1000.
- 20. Mallal S, Nolan D, Witt C, et al. Association between presence of HLA-B*5701, HLA-DR7, and HLA-DQ3 and hypersensitivity to HIV-1 reverse-transcriptase inhibitor abacavir. Lancet 2002; 359: 727-732.
- 21. Hetherington S, Hughes AR, Mosteller M, et al. Genetic variations in HLA-B region and hypersensitivity reactions to abacavir. Lancet 2002; 359: 1121-1122.
- 22. Martin AM, Nolan D, Gaudieri S, et al. Predisposition to abacavir hypersensitivity conferred by HLA-B*5701 and a haplotypic Hsp70-Hom variant. Proc Natl Acad Sci U S A 2004; 101: 4180-4185.
- 23. Rauch A, Nolan D, Martin A, et al. Prospective genetic screening decreases the incidence of abacavir hypersensitivity reactions in the Western Australian HIV cohort study. Clin Infect Dis 2006; 43: 99-102.
- 24. Phillips EJ. Genetic screening to prevent abacavir hypersensitivity reaction: are we there yet? Clin Infect Dis 2006; 43: 103-105.
- 25. Barrios A, Garcia-Benayas T, Gonzalez-Lahoz J, et al. Tenofovir-related nephrotoxicity in HIV-infected patients. AIDS 2004; 18: 960-963.
- 26. Karras A, Lafaurie M, Furco A, et al. Tenofovir-related nephrotoxicity in human immunodeficiency virus-infected patients: three cases of renal failure, Fanconi syndrome, and nephrogenic diabetes insipidus. Clin Infect Dis 2003; 36: 1070-1073.
- 27. Rutherford GW, Sangani PR, Kennedy GE. Three- or four- versus two-drug antiretroviral maintenance regimens for HIV infection. Cochrane Database Syst Rev 2003; (4): CD002037.
- 28. Sanne I, Mommeja-Marin H, Hinkle J, et al. Severe hepatotoxicity associated with nevirapine use in HIV-infected subjects. J Infect Dis 2005; 191: 825-829.
- 29. Starr SE, Fletcher CV, Spector SA, et al. Combination therapy with efavirenz, nelfinavir, and nucleoside reverse-transcriptase inhibitors in children infected with human immunodeficiency virus type 1. Pediatric AIDS Clinical Trials Group 382 Team. N Engl J Med 1999; 341: 1874-1881.
- 30. Friis-Moller N, Sabin CA, Weber R, et al. Combination antiretroviral therapy and the risk of myocardial infarction. N Engl J Med 2003; 349: 1993-2003.
- 31. Friis-Moller N, Weber R, Reiss P, et al. Cardiovascular disease risk factors in HIV patients — association with antiretroviral therapy. Results from the DAD study. AIDS 2003; 17: 1179-1193.
- 32. van Leth F, Phanuphak P, Ruxrungtham K, et al. Comparison of first-line antiretroviral therapy with regimens including nevirapine, efavirenz, or both drugs, plus stavudine and lamivudine: a randomised open-label trial, the 2NN Study. Lancet 2004; 363: 1253-1263.
- 33. van Leth F, Phanuphak P, Stroes E, et al. Nevirapine and efavirenz elicit different changes in lipid profiles in antiretroviral-therapy-naive patients infected with HIV-1. PLoS Med 2004; 1: e19.
- 34. Staszewski S, Morales-Ramirez J, Tashima KT, et al. Efavirenz plus zidovudine and lamivudine, efavirenz plus indinavir, and indinavir plus zidovudine and lamivudine in the treatment of HIV-1 infection in adults. Study 006 Team. N Engl J Med 1999; 341: 1865-1873.
- 35. Stern JO, Robinson PA, Love J, et al. A comprehensive hepatic safety analysis of nevirapine in different populations of HIV infected patients. J Acquir Immune Defic Syndr 2003; 34 Suppl 1: S21-S33.
- 36. Dorenbaum A, Cunningham CK, Gelber RD, et al. Two-dose intrapartum/newborn nevirapine and standard antiretroviral therapy to reduce perinatal HIV transmission: a randomized trial. JAMA 2002; 288: 189-198.
- 37. Cunningham CK, Chaix ML, Rekacewicz C, et al. Development of resistance mutations in women receiving standard antiretroviral therapy who received intrapartum nevirapine to prevent perinatal human immunodeficiency virus type 1 transmission: a substudy of pediatric AIDS clinical trials group protocol 316. J Infect Dis 2002; 186: 181-188.
- 38. Therapeutic Goods Administration. Department of Health and Ageing. Access to unapproved therapeutic goods via the Special Access Scheme. Canberra: Department of Health and Ageing, 2004. http://www.tga.gov.au/docs/pdf/unapproved/sas.pdf (accessed Dec 2006).
- 39. Squires K, Lazzarin A, Gatell JM, et al. Comparison of once-daily atazanavir with efavirenz, each in combination with fixed-dose zidovudine and lamivudine, as initial therapy for patients infected with HIV. J Acquir Immune Defic Syndr 2004; 36: 1011-1019.
- 40. Lalezari JP, Henry K, O’Hearn M, et al. Enfuvirtide, an HIV-1 fusion inhibitor, for drug-resistant HIV infection in North and South America. N Engl J Med 2003; 348: 2175-2185.
- 41. Kitahata MM, Koepsell TD, Deyo RA, et al. Physicians’ experience with the acquired immunodeficiency syndrome as a factor in patients’ survival. N Engl J Med 1996; 334: 701-706.
- 42. Carr A, Samaras K, Burton S, et al. A syndrome of peripheral lipodystrophy, hyperlipidaemia and insulin resistance in patients receiving HIV protease inhibitors. AIDS 1998; 12: F51-F58.
- 43. Martinez E, Mocroft A, Garcia-Viejo MA, et al. Risk of lipodystrophy in HIV-1-infected patients treated with protease inhibitors: a prospective cohort study. Lancet 2001; 357: 592-598.
- 44. Carr A, Hudson J, Chuah J, et al. HIV protease inhibitor substitution in patients with lipodystrophy: a randomized, controlled, open-label, multicentre study. AIDS 2001; 15: 1811-1822.
- 45. Carr A, Workman C, Smith DE, et al. Abacavir substitution for nucleoside analogs in patients with HIV lipoatrophy: a randomized trial. JAMA 2002; 288: 207-215.
- 46. Martin A, Smith DE, Carr A, et al. Reversibility of lipoatrophy in HIV-infected patients 2 years after switching from a thymidine analogue to abacavir: the MITOX Extension Study. AIDS 2004; 18: 1029-1036.
- 47. Mannheimer S, Friedland G, Matts J, et al. The consistency of adherence to antiretroviral therapy predicts biologic outcomes for human immunodeficiency virus-infected persons in clinical trials. Clin Infect Dis 2002; 34: 1115-1121.
- 48. Paterson DL, Swindells S, Mohr J, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med 2000; 133: 21-30.
- 49. Bangsberg DR, Moss AR, Deeks SG. Paradoxes of adherence and drug resistance to HIV antiretroviral therapy. J Antimicrob Chemother 2004; 53: 696-699.
- 50. The Strategies for Management of Antiretroviral Therapy (SMART) Study Group. CD4+ count-guided interruption of antiretroviral treatment. N Engl J Med 2006; 355: 2283-2296.
- 51. Perelson AS, Neumann AU, Markowitz M, et al. HIV-1 dynamics in vivo: virion clearance rate, infected cell life-span, and viral generation time. Science 1996; 271: 1582-1586.
- 52. de Mendoza C, Rodriguez C, Colomina J, et al. Resistance to nonnucleoside reverse-transcriptase inhibitors and prevalence of HIV type 1 non-B subtypes are increasing among persons with recent infection in Spain. Clin Infect Dis 2005; 41: 1350-1354.
- 53. Wensing AM, Boucher CA. Worldwide transmission of drug-resistant HIV. AIDS Rev 2003; 5: 140-155.
- 54. Wensing AM, van de Vijver DA, Angarano G, et al. Prevalence of drug-resistant HIV-1 variants in untreated individuals in Europe: implications for clinical management. J Infect Dis 2005; 192: 958-966.
- 55. Little SJ, Holte S, Routy JP, et al. Antiretroviral-drug resistance among patients recently infected with HIV. N Engl J Med 2002; 347: 385-394.
- 56. Gill CJ, Griffith JL, Jacobson D, et al. Relationship of HIV viral loads, CD4 counts, and HAART use to health-related quality of life. J Acquir Immune Defic Syndr 2002; 30: 485-492.
- 57. Carrieri P, Spire B, Duran S, et al. Health-related quality of life after 1 year of highly active antiretroviral therapy. J Acquir Immune Defic Syndr 2003; 32: 38-47.
- 58. Liu C, Weber K, Robison E, et al. Assessing the effect of HAART on change in quality of life among HIV-infected women. AIDS Res Ther 2006; 3: 6.





Abstract
Over the past 10 years, the management of HIV infection has been transformed by an increased number of effective antiretrovirals (ARVs), with more convenient dosing and improved tolerability.
Optimal management of HIV infection includes at least three effective ARVs; from at least two different drug classes.
Current strategies and drugs can effectively control HIV and significantly reduce morbidity and mortality. However, no cure is yet possible.
Appropriate use of ARVs leads to suppression of virological replication (to below the limit of detection using commercial assays to measure HIV in plasma) and an increase in CD4+ T cells with few adverse effects.
Greater than 95% adherence to drug therapy is required for effective viral suppression and immunological improvement.
Monotherapy, two-drug combinations, sequential ARVs, drug “cycling”, and treatment interruptions are ineffective management strategies and lead to earlier disease progression and emergence of drug resistance.
Drug–drug interactions are common and caution is required when prescribing ARVs that inhibit or induce the cytochrome P450 pathway.