Domiciliary oxygen therapy (DOT) is an effective therapy for some patients with cardiopulmonary disease and chronic respiratory failure. The most common indication is for patients with hypoxic chronic obstructive pulmonary disease (COPD), in whom it improves survival.1,2 Other indications for use of oxygen, including ambulatory oxygen therapy (for which there is less evidence) are included in the Australian guidelines for DOT,3,4 but there are limited data on adherence to these guidelines.5,6
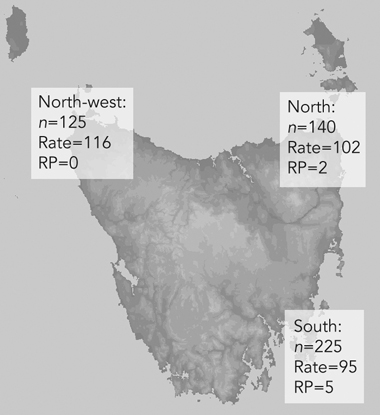
The use of DOT has been evaluated in Tasmania. Tasmania has three distinct regions: south (Hobart area), north (Launceston area) and north-west (Burnie area), and respiratory services differ between these regions. In 2002, high prescription rates of oxygen therapy and associated high costs in the north-west region led to the establishment of an oxygen clinic there.7 This gave us an opportunity to analyse the impact of an oxygen clinic in an area where Australian guidelines were not used to guide oxygen prescriptions (the other regions had local guidelines adapted from the Australian guidelines), and DOT could be prescribed by any medical practitioner.
The use of DOT was compared with the national guidelines current at the time of the study,3 which recommended long-term oxygen treatment for people with COPD with a Pao2 of ≤ 55 mmHg, or for stable, optimally managed patients with cor pulmonale and/or pulmonary hypertension with a Pao2 of 55–59 mmHg. Oxygen use for > 15 hours per day and reassessment within a 1-month timeframe is advised.
Our study documented patterns of government-funded DOT in Tasmania and showed the beneficial impact of a dedicated oxygen clinic. The prevalence of oxygen prescription of 102 patients per 100 000 population in Tasmania, after an oxygen clinic was established in one region, is similar to the prescription rate of 111 per 100 000 in South Australia.8 Extrapolating our data to the whole of Australia suggests that about 21 000 people are currently using DOT in Australia.
We found a regional variation in DOT prescription, which was related to rural residence and the number of respiratory physicians, similar to findings of a study on home oxygen in Denmark.9 COPD was the most common indication for DOT, which has also been found by researchers in other countries.10-14 The total state-wide cost of DOT was over $750 000 per annum, similar on a per-patient basis to the cost of DOT in South Australia.8 If the cost per patient is similar nationally, this would equate to an annual spending of $31.5 million by state governments.
Our study suggested several deficiencies in the DOT service. Over half the patients started oxygen treatment during hospitalisation, and it is unlikely they would have fulfilled the Thoracic Society of Australia and New Zealand’s recommendations for oxygen prescription at this time. Some overseas national guidelines specifically prohibit the prescription of long-term oxygen during a hospital stay.15,16 Even allowing for this, a substantial minority of recipients were prescribed oxygen outside the current guidelines, and this was more likely to occur when prescription was not by a respiratory physician.
Although the median hours of daily use appeared reassuring of guideline adherence, closer analysis showed that 30% of patients prescribed DOT for COPD used oxygen for less than the recommended 15 hours per day.1,2 Perhaps this is not surprising; previous studies of patients with COPD have shown effective usage to vary between 17% and 70%,17-19 one study showing only 45% of patients used oxygen for more than 15 hours.20 In these studies, appropriate DOT use was more likely to occur in those who had more severe disease, and who had received initial education in the use of DOT from a physician and ongoing education from a nurse and physiotherapist. In our study, we also found that specialist input seemed to have a beneficial impact on effective use of oxygen therapy.
We found an unacceptably long time to first reassessment, despite many patients commencing DOT as inpatients (which correlates poorly with ongoing need for oxygen therapy at 2 months).15 The data on reassessment were limited, as some patients were followed up outside the public hospital system, but, as far as we were able to establish, up to 20% of patients had no follow-up at all. The few studies available suggest that follow-up has also been poor outside Australia, with only 17.5% of people in a Danish study being followed up adequately at 10 months after prescription.16
1 The distribution of use of domiciliary oxygen therapy in Tasmania
 |
|
n = total no. of patients receiving domiciliary oxygen therapy. |
2 Indications for prescription of domiciliary oxygen therapy according to region of Tasmania, April 2004
Number (%) of people prescribed |
|||||||||||||||
- Andrew Jones1
- Richard Wood-Baker2
- E Haydn Walters3
- University of Tasmania, Hobart, TAS.
We would like to thank the Department of Health and Human Services, Tasmania, for providing funding for Andrew Jones; Wendy Chatwin for assistance with the oxygen clinic; and Air Liquide Healthcare for providing data.
Andrew Jones is employed by the University of Tasmania and the Department of Health and Human Services, Tasmania, to investigate home oxygen services in Tasmania.
- 1. Nocturnal Oxygen Therapy Trial Group. Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease. Ann Intern Med 1980; 93: 391-398.
- 2. Long term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema. Report of the Medical Research Council Working Party. Lancet 1981; 1: 681-685.
- 3. Young IH, Crockett AJ, McDonald CF. Adult domiciliary oxygen therapy. Position statement of the Thoracic Society of Australia and New Zealand. Med J Aust 1998; 168: 21-25. <MJA full text>
- 4. McDonald CF, Crockett AJ, Young IH. Adult domiciliary oxygen therapy. Position statement of the Thoracic Society of Australia and New Zealand. Med J Aust 2005; 182: 621-626. <MJA full text>
- 5. Crockett A, Moss J, Alpers J. The continuing impact of home oxygen for respiratory patients on a hospital budget. Aust Health Rev 1992; 15: 259-268.
- 6. McKeon JL, Saunders NA, Murree-Allen K. Domiciliary oxygen: rationalization of supply in the Hunter region from 1982-1986. Med J Aust 1987; 146: 73-78.
- 7. Chaney JC, Jones K, Grathwohl K, Olivier K. Implementation of an oxygen clinic to manage users of long term oxygen therapy. Chest 2002; 122: 1661-1667.
- 8. Crockett AJ, Cranston JM, Moss JR. Economic case statement chronic obstructive pulmonary disease. Brisbane: Australian Lung Foundation, 2002.
- 9. Ringback TJ, Lange P, Viskum K. Geographic variation in long term oxygen therapy in Denmark. Chest 2001; 119: 1711- 1716.
- 10. Morrison D, Skwarski K, MacNee W. Review of the prescription of domiciliary oxygen therapy in Scotland. Thorax 1995; 50: 1103-1105.
- 11. Tobiasz M. [Five years of home oxygen in Poland] [Polish]. Pol Tyg Lek 1993; 48: 150-153.
- 12. Bongard JP, de Haller R. [Long term oxygen therapy in Switzerland] [French]. Schweiz Med Wochenschr 1989; 119: 110-115.
- 13. Sivakumaran P, Garrett JE. The prescription of domiciliary long-term oxygen therapy in Auckland. N Z Med J 1996; 109: 439-442.
- 14. Gamez J, Triano E, Romero D, et al. [Domiciliary oxygen therapy. Study of use in a rural area] [Spanish]. An Med Interna 1998; 15: 358-362.
- 15. Eaton TE, Grey C, Garrett JE. An evaluation of short term oxygen therapy: the prescription of oxygen to patients with chronic lung disease hypoxic at discharge from hospital. Respir Med 2001; 95: 582-587.
- 16. Ringbaek TJ, Lange P, Viskum K. Are patients on long term oxygen therapy followed up properly? Data from the Danish Oxygen Register. J Intern Med 2001; 250: 131-136.
- 17. Vergeret J, Bambilla C, Mournier L. Portable oxygen therapy: use and benefit in hypoxemic COPD patients on long term oxygen therapy. Eur Respir J 1989; 2: 20-25.
- 18. Walshaw MJ, Lim R, Evans CC, et al. Factors influencing the compliance in patients using oxygen concentrators for long term home oxygen therapy. Respir Med 1990; 84: 331-333.
- 19. Restrick LJ, Paul EA, Braid GM, et al. Assessment and follow up of patients prescribed long term oxygen therapy. Thorax 1993; 48: 708-713.
- 20. Pepin JL, Barjhoux E, Deschaux C, Brambilla C. Long term oxygen therapy at home. Chest 1996; 109: 1144-1150.





Abstract
Objective: To assess the use of domiciliary oxygen therapy (DOT) in Tasmania and the impact of a specialist oxygen clinic on service provision.
Design: Retrospective observational study.
Participants and setting: Patients prescribed government-funded DOT in Tasmania between December 2002 and April 2004.
Main outcome measures: Indications for DOT; usage, prescription, reassessment and costs of DOT; influence of a specialist-run oxygen clinic.
Results: 490 patients were using DOT, an overall rate of 102 patients per 100 000 population (varying between regions from 95 to 116 per 100 000 population). Of 267 patients (54%) prescribed DOT during hospitalisation, only 72% met national guidelines for DOT at commencement. Chronic obstructive pulmonary disease (COPD) was the most common indication (48% of prescriptions). The median time to reassessment after prescription was 5.5 months. Median usage in patients with COPD was 18.3 hours per day. The average cost per patient was $1498 per year, but differed regionally in relation to costs of ambulatory supplies. The oxygen clinic in the north-west region substantially reduced oxygen prescriptions, improved compliance with guidelines, decreased time to first reassessment from 21 to 6.6 months, and produced major cost savings.
Conclusions: Prescription of DOT was often not in keeping with national guidelines. Reassessment was poor, despite more than half the patients being prescribed DOT as an inpatient. A dedicated oxygen clinic resulted in more appropriate prescription, decreased time to reassessment and a reduction in costs.