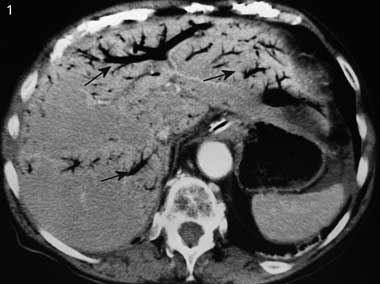
A 90-year-old woman was admitted with acute vomiting for the previous 24 hours and acute, diffuse, intense abdominal pain. Her medical history included atrial fibrillation and hysterectomy. Clinical examination revealed a generally distended, tender, tympanic and silent abdomen. Blood pressure was 98/54 mmHg; her pulse was irregular at 67 beats per minute. A plain x-ray of the abdomen revealed bowel distension without air–fluid levels. A computed tomography scan of the abdomen showed the presence of gas in the portal venous system (Box 1) and the intestinal wall (Box 2). At laparotomy, 142 cm of necrotic ileum was removed. The postoperative course was uneventful, and the patient was discharged 1 month later.
The precise mechanism for formation of gas in the portal venous system is uncertain.1 The primary factors that favour this development are intestinal wall alterations, bowel distension and intra-abdominal sepsis.1 In many cases, two or three of these circumstances may coexist. In 15% of cases, the cause of air in the portal venous system remains unknown.1 Several conditions, such as perforated ulcer, interventional procedures, trauma, and infectious or inflammatory abdominal diseases, but most commonly intestinal ischaemia (as in our patient), can cause alterations of the gastric and bowel wall, permitting the passage of intraluminal gas into the portal venous system.1-3 Gas from the intestinal lumen passes through the intestinal wall and travels via the small mesenteric veins and the superior or inferior mesenteric vein to the portal venous system. Further, the presence of gas simultaneously in the portal venous system and intestinal wall seems to be specific to intestinal ischemia.4
Because hypotension was moderate and usual in our patient, we believe that the intestinal ischaemia was secondary to embolic disease related to atrial fibrillation. This case also demonstrates that portal venous system gas formation does not necessarily imply a worse prognosis and that surgery may be beneficial in the presence of this sign.1,5
- Ali Mofredj1
- Harry Toledano2
- Richard Boutboul3
- Centre Hospitalier Général, Salon De Provence, France.
- 1. Sebastià C, Quiroga S, Espin E, et al. Portomesenteric vein gas: pathologic mechanisms, CT findings, and prognosis. Radiographics 2000; 20: 1213-1224.
- 2. Saksena M, Harisinghani MG, Wittenberg J, Mueller PR. Hepatic portal venous gas: transient radiographic finding associated with colchicine toxicity. Br J Radiol 2003; 76: 835-837.
- 3. Paran H, Epstein T, Gutman M, et al. Mesenteric and portal vein gas: computerized tomography findings and clinical significance. Dig Surg 2003; 20: 127-132.
- 4. Wiesner W, Khurana B, Ji H, Ros PR. CT of acute bowel ischemia. Radiology 2003; 226: 635-650.
- 5. Faberman RS, Mayo-Smith WW. Outcome of 17 patients with portal venous gas detected by CT. AJR Am J Roentgenol 1997; 169: 1535-1538.