Clinical records
Patient 1
A 5-month-old girl presented with biphasic stridor (ie, stridor present during inspiration and expiration) and feeding difficulties since birth. The stridor was not related to her position or to her level of wakefulness. Asthma treatment with bronchodilators, inhaled corticosteroids (up to 500 μg/day fluticasone propionate) and courses of oral steroids were prescribed by several doctors from 6 weeks of age for her “noisy breathing”. These treatments did not alter her symptoms. No investigations were undertaken. There was no significant perinatal or other medical history.
The child appeared well; she was thriving and her development was appropriate for her age. The biphasic stridor was not associated with wheeze or tachypnoea. She had mild tracheal tug and chest wall recession. Her chest was clear, and the findings from the remainder of the examination were normal.
A chest x-ray (CXR) showed a right aortic arch and reduced air–tissue interface at the carina, consistent with tracheomalacia. A barium swallow showed a posterior indentation of the mid-oesophagus, suggestive of a vascular ring (extrinsic compression of the oesophagus and trachea by aberrantly sited blood vessels [Box 1]). Bronchoscopy confirmed these findings and showed significant reflux oesophagitis. A magnetic resonance angiogram confirmed the presence of a vascular ring formed by a double aortic arch, with each arch giving rise to its own common carotid and subclavian arteries.
Surgical correction of the compressive vascular band on the trachea 3 days later was uneventful. The proton pump inhibitor omeprazole was prescribed for the reflux oesophagitis, but this proved insufficient. After further hospitalisations for pulmonary aspiration, a fundoplication was performed and a gastrostomy tube inserted. Twelve months later, she remains asymptomatic with normal growth.
Patient 2
A 9-week-old girl presented with biphasic stridor and a 3-week history of intermittent central cyanosis associated with feeding. She was noted to have had “noisy breathing” from birth.
At age 6 weeks, she had been admitted to another hospital with cough and more prominent biphasic stridor. Her respiratory difficulties were attributed to bronchiolitis caused by respiratory syncytial virus. She required supportive treatment including oxygen for 5 days in hospital. On discharge, she improved, but continued to have very noisy breathing, which was worse when she was active or feeding. She was bottle fed with infant formula and noted to have occasional episodes of transient cyanosis during feeding.
On examination, she appeared well and was thriving. She had a moist cough, moderate subcostal recession and audible biphasic stridor.
A CXR showed a left, normally sited aortic arch and poor delineation of the distal tracheal air column suggestive of tracheomalacia. A barium swallow (Box 2A) showed significant oesophageal compression anteriorly and posteriorly, consistent with a double aortic arch. A magnetic resonance angiogram (Box 2B) confirmed the presence of the double aortic arch, as well as extrinsic, anterior compression of the distal trachea. Bronchoscopy, performed before surgery to divide the vascular ring, showed mild tracheomalacia.
The infant was discharged a week later with reduced stridor and recession. No further episodes of central cyanosis with feeding occurred during the 6-month follow-up period after surgery.
Biphasic stridor from birth or early infancy suggests fixed proximal airway obstruction, which may be intra- or extrathoracic. Conversely, variable inspiratory stridor suggests a less severe, extrathoracic, dynamic obstruction. Patients with biphasic stridor (such as that caused by a vascular ring) are often initially misdiagnosed as having asthma because of noisy respirations, although stridor is never a sign of asthma, but rather of proximal airway compromise. Stridor differs from wheeze in that it has a different pitch and harsher sound than the more musical pitch of a wheeze. Stridor is heard predominantly during inspiration.
Children with a vascular ring usually present in infancy with non-specific symptoms of dyspnoea, cough, inspiratory or biphasic stridor, and sometimes an expiratory “wheeze” (presumably related to downstream obstruction of the intrathoracic trachea) as well as feeding problems.3-5 A vascular ring occurs when one or more aortic arch abnormalities, with or without a patent ductus arteriosus or ligamentum, produce a ring that completely encircles the trachea and oesophagus, leading to symptoms of tracheal or oesophageal compression6 (Box 1).
The differential diagnosis of persistent biphasic stridor in an infant includes severe laryngomalacia, tracheomalacia and, less commonly, vocal cord paresis (causing a hoarse cry), subglottic haemangioma (causing rapidly progressing stridor, sometimes associated with a facial haemangioma) and vascular ring.
Laryngomalacia is the most common cause of neonatal inspiratory stridor, but is an unlikely cause of biphasic stridor from birth, unless it is very severe. Stridor in laryngomalacia more commonly occurs after several weeks of age, is usually limited to inspiration and varies with posture and airflow (eg, it is louder with crying). Signs usually gradually resolve without treatment by 12 to 18 months of age.7
Tracheomalacia, a condition characterised by weakness of the tracheal walls and supporting cartilage (localised to the region of external compression by blood vessels), commonly occurs in association with lesions such as a vascular ring and persists for several years until the tracheal cartilage firms.
The formation of the ring depends on the preservation or deletion of specific segments of the rudimentary aortic arch complex, or the presence of major arteries with anomalous origins or remnants (eg, ligamentum arteriosum) compressing the trachea and oesophagus. The double aortic arch is the most common form of vascular ring,4 and is characterised by persistence of both embryonic aortic arches, with separate carotid and subclavian arteries originating from each arch. The ascending aorta bifurcates anterior to the trachea to form the aortic arches, and each courses either right or left of the trachea and the oesophagus. The larger of the two arches usually crosses posterior to the oesophagus and unites with the other arch in the posterior mediastinum to form the single descending aorta. This can be seen as a posterior indentation on the mid-oesophagus on a barium swallow (Box 2A).
When biphasic stridor is detected in an infant, a chest x-ray (CXR) and a barium swallow are simple initial investigations that together will usually confirm or exclude a vascular ring as the underlying cause.8-10 The CXR may show a right-sided aortic arch, a poorly visualised distal trachea, or another cause for tracheal compression or deviation (eg, a mediastinal mass). A barium swallow may show abnormal indentations on the posterior oesophageal wall. If these abnormalities are detected, referral for more detailed investigations (including bronchoscopy and magnetic resonance angiography) and treatment is appropriate.11,12 Tracheomalacia may occur in isolation, and the diagnosis often relies on the bronchoscopist’s interpretation of the airway calibre and shape at bronchoscopy.
After surgical treatment for a vascular ring, it is essential that the child’s parents receive ongoing management advice, as tracheomalacia will persist, and there is therefore an increased risk of severe croup. The child may continue to display noisy breathing for a period of a few months to several years13 and should be followed up until school age.
In school-age children, any residual inspiratory flow limitation can be quantified using inspiratory flow volume loops with spirometry. Residual tracheomalacia commonly results in difficulty clearing airway secretions (impaired mucociliary clearance) through the functionally narrowed section of trachea at the site of the previous extrinsic wall compression. This may manifest as a brassy, rattly cough that persists longer than expected after a viral infection. It would be appropriate to consider influenza and pneumococcal vaccination in these children.
1: A double aortic arch (as in Patient 1)
The simplified anatomy of a double aortic arch, which produces a vascular ring encircling the trachea and oesophagus, causing symptoms of tracheal or oesophageal compression.
2: Investigations for biphasic stridor (Patient 2)
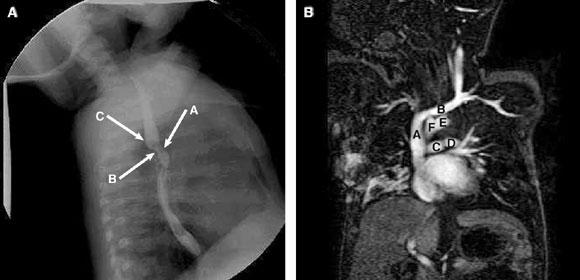
2A: Barium swallow, showing anterior (arrow A) and posterior (arrow B) compression of the oesophagus, together with a posterior bulge (arrow C) caused by a double aortic arch.
2B: Magnetic resonance image, showing the double aortic arch — superior vena cava (A), brachiocephalic vein (B), pulmonary arteries (C, D), prominent left aortic arch (E), and smaller right aortic arch (F).
- 1. Valletta EA, Pregarz M, Bergamo-Andreis IA, et al. Tracheoesophageal compression due to congenital vascular anomalies (vascular rings). Pediatr Pulmonol 1997; 24: 93-105.
- 2. Chun K, Colombani PM, Dudgeon DL, et al. Diagnosis and management of congenital vascular rings: a 22 year experience. Ann Thorac Surg 1992; 53: 597-602.
- 3. Bakker DA, Berger RM, Witensburg M, et al. Vascular rings: a rare cause of common respiratory symptoms. Acta Paediatr 1999; 88: 947-952.
- 4. Bharati S, Lev M. The pathology of congenital heart disease. New York: Futura Publishing Company, 1996.
- 5. McGill TJ, Healy GB. Congenital and acquired lesions of the infant larynx. A refresher survey. Clin Pediatr (Phila) 1978; 17: 584-589.
- 6. Pickhardt PJ, Siegel MF, Gutierrez FR. Vascular rings in symptomatic children: frequency of chest radiographic findings. Radiology 1997; 203: 423-426.
- 7. Lowe GM, Donaldson JS, Backer CL. Vascular rings: 10 year review of imaging. Radiographics 1991; 11: 637-646.
- 8. Skinner LJ, Ryan S, Russell JD. Complete vascular ring detected by barium oesophagography. Ear Nose Throat J 2002; 81: 554-555.
- 9. Beekman RP, Beek FJ, Hazekamp MG, et al. The value of MRI in diagnosing vascular abnormalities causing stridor. Eur J Paediatr 1997; 156: 516-520.
- 10. Beekman RP, Hazekamp MG, Sobotka MA, et al. A new diagnostic approach to vascular rings and pulmonary slings: the role of MRI. Magn Reson Imaging 1998; 16: 137-145.
- 11. Van Son JA, Julsrud PR, Hagler DJ, et al. Surgical treatment of vascular rings: the Mayo Clinic experience. Mayo Clin Proc 1993; 68: 1056-1063.





We would like to acknowledge our surgical colleagues, Dr Ted Beckenham, Dr John Harvey and Dr David Winlaw, for their operative care and Dr Kristina Prelog for assistance with the radiology images.
None identified.