Practice based on the best available evidence and the quality and safety of healthcare have become a major focus for governments, healthcare providers and consumers. This increased awareness comes at a time when new heights have been reached in the technical sophistication of care, healthcare systems have become incredibly complex, and there is a potential for patients to be harmed by healthcare interventions.1
Adverse events can seldom be attributed to a single human error and are usually associated with the complex system interactions.1-3 The Quality in Australian Health Care Study,4 published in 1995, served as a catalyst in Australia for promoting system-based approaches to safety and quality improvement. The Clinical Support Systems Program (CSSP)5 is a practical example of this.
The CSSP emerged through collaboration between the Royal Australasian College of Physicians (RACP) and the Australian Government Department of Health and Ageing (the Department), and was subsequently sponsored and managed by the RACP. The Department provided most of the funding, with the Victorian Department of Human Services and NSW Health each contributing $500 000, resulting in combined funds of $5.5 million. The formal funded phase of the Program ran from 2000 to 2002.
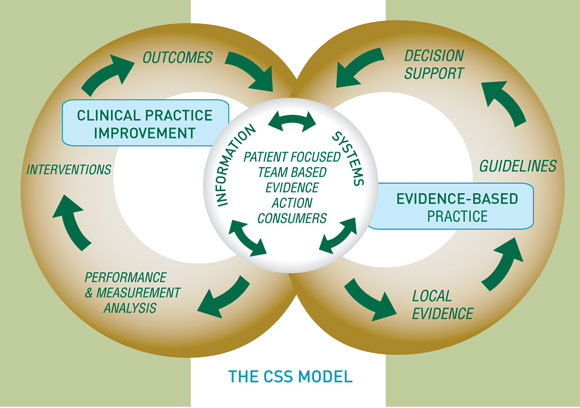
The Program sought to assist the routine uptake of best evidence within clinical practice through a Clinical Support Systems (CSS) model. This model combined the principles of clinical practice improvement (CPI)6 and evidence-based medicine (EBM)7 into a broad framework to enable clinicians to embed best practice routinely in clinical care. It had the following broad specifications (see also Box 1):
involvement by clinical teams, health managers and consumers in design, development, implementation and evaluation;
establishment of organisational and management structures and tools necessary to develop and maintain capacity for CPI;
systematic use of evidence within clinical settings;
systematic clinical work practices to reduce inappropriate variation;
development of data and analysis systems to support CPI; and
routine measurement and review of clinical practices.
The CSS model was tested through four consortium-based projects that collectively involved 17 clinical sites across three states. The four projects were selected through a competitive tendering process, based on specific criteria: the projects should involve areas of care that were high cost, high volume or high risk; and for which there was a significant level of evidence relating to diagnosis and treatment, and tangible indicators for a difference between this evidence and current practice.
The successful consortia and their projects were:
Austin Bowel Cancer Consortium — implemented National Health and Medical Research Council guidelines for colorectal cancer care,8 spanning multiple episodes of acute care (surgery and oncology) in three hospitals: metropolitan, regional and private.
Brisbane Cardiac Consortium — adapted national guidelines for management of acute coronary syndromes9 and congestive heart failure10 and systematically implemented the evidence within three hospitals and in general practice.
Monash University Consortium — developed local protocols based on the best available evidence (in the absence of national guidelines) for managing patients with acute stroke (first 7 days) and implemented them in four hospital sites: tertiary, regional, rural and private.
Towards a Safer Culture (TASC) Consortium — focused on management of acute coronary syndromes9 and stroke (for which there were no such guidelines). The principal area of interest was the emergency department. This program was subsequently extended to the inpatient setting of four hospitals in New South Wales, Queensland and Victoria.
The primary aim of each project was to embed the best available evidence into local routine clinical practice. The focus was not on generating new evidence or on proving that evidence-based care improves outcomes for patients. Instead, the projects focused on the structural and cultural dimensions of care, with tangible outcomes such as developing information systems, protocols, tools and organisational pathways necessary to support evidence-based care and influence clinicians to use evidence routinely and sustainably.
There was considerable variation between the projects. This heterogeneity included the clinical focus, the amount and type of evidence available and the tasks required to implement the evidence; the environment in which changes were sought; and the number, type and geographical spread of project partners. Projects also varied in their interpretations of the CSS model, change management strategies, project objectives and methods. Each project evolved into a unique, integrated combination of these defining features.
The 2-year time frame, and local and wider health system issues over which projects had no direct control, resulted in the projects experiencing varying success. Nevertheless, the consortia all increased their capacity to provide evidence-based care for their patients.
The details of their achievements are described in this Supplement (pages S79, S83, S89 and S92).11-14 These projects illustrate the changes required in the structural and cultural dimensions of care to progress towards evidence-based practice becoming routine (Box 2). The projects also uncovered many issues relating to the clinicians and the environments involved, as well as the underlying strategies needed to support implementation of both EBM and CPI.
Aspects of the CSSP projects have continued beyond the 2-year funding phase in each of the participating hospitals. In two instances, important project components were taken up by state governments. The Brisbane Cardiac Consortium data sets for acute coronary syndrome and congestive heart failure have been adopted by Queensland Health for wider application. The TASC methodology for management of patients presenting to emergency departments with acute coronary syndromes and stroke is now in use in public hospitals in NSW, funded by the NSW Institute for Clinical Excellence. The RACP has actively promoted uptake of the CSS model in other settings. There is a TASC stroke project in Western Australia, a project targeting otitis media in northern South Australia, another in rural Victoria focusing on community-acquired pneumonia (CAP), and three projects in New Zealand. Clinicians around Australia are now implementing various forms of the CSS model.
The CSSP has generated a unique web-based tool that provides a practical introduction to the CSS model and draws heavily on the experiences of clinicians involved in the CSSP.15
An overarching outcome of the CSSP is that it has confirmed that healthcare providers are committed to improving the quality of care. Participants have welcomed the opportunity to reflect on their practice in the light of the best available evidence and CPI. Indeed, the CSSP has created a learning laboratory for its participants and contributed to an increased system capacity to improve healthcare.
Further information about the CSSP can be found by visiting the RACP website www.racp.edu.au/bp
2: The CSSP projects’ achievements in targeting the structural and cultural dimensions of care
Effective teams crossing entrenched structural and professional boundaries
Improved care systems across interfaces
Improved attitudes towards clinical practice guidelines, clinical practice improvement and consumer involvement
Improved staff morale and sense of empowerment
Evidence-based tools for clinicians and consumers
Information systems providing clinicians with timely, meaningful feedback
Improvements in many clinical and organisational outcome indicators
- 1. Committee on Quality Health Care in America; Institute of Medicine. To err is human: building a safer health system. Washington, DC. National Academy Press, 2001.
- 2. Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalised patients. N Engl J Med 1991; 324: 370-376.
- 3. Committee on Quality Health Care in America; Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academy Press, 2001.
- 4. Wilson RMcL, Runciman W, Gibbard R, et al. The Quality in Australian Health Care Study. Med J Aust 1995; 163: 458-471. <eMJA pdf>
- 5. Larkins RG, Long PW, Patterson CG. The Clinical Support Systems Program concept: what is it and where did it come from? Intern Med J 2001; 31: 416-417.
- 6. James B, Horn S, Stephenson R. Managing by fact: what is CPI and how is it used? Clinical practice improvement: a new technology for developing cost-effective quality health care. New York: Faulkner & Grey, 1994.
- 7. Sackett DL, Rosenberg WM, Gray JA, et al. Evidence based medicine: what is it and what it isn’t. BMJ 1996; 312: 71-72.
- 8. National Health and Medical Research Council. Guidelines for the prevention, early detection and management of colorectal cancer. Canberra: NHMRC, 1999. Available at: www.health.gov.au/nhmrc/publications/synopses/cp62syn.htm (accessed Apr 2004).
- 9. Aroney CN, Boyden AN, Jelinek MV, et al. Management of unstable angina. Guidelines – 2000. Med J Aust 2000; 173 (8 Suppl): S65-S88.
- 10. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand Chronic Heart Failure Clinical Practice Guidelines Writing Panel. Guidelines for management of patients with chronic heart failure in Australia. Med J Aust 2001; 174: 459-466. <eMJA full text>
- 11. Mitchell PLR, White CA. Austin Bowel Cancer Consortium: changing culture in bowel cancer care. Med J Aust 2004; 180 (10 Suppl): S79-S82.<eMJA full text>
- 12. Scott IA, Denaro CP, Bennett CJ, et al. Achieving better in-hospital and after-hospital care of patients with acute cardiac disease. Med J Aust 2004; 180 (10 Suppl): S83-S88.<eMJA full text>
- 13. Horne MK. The Monash University Consortium: factors involved in the local implementation of clinical evidence into practice. Med J Aust 2004; 180 (10 Suppl): S89-S91.<eMJA full text>
- 14. Ferry CT, Fitzpatrick MA, Long PW, et al. Towards a Safer Culture: clinical pathways in acute coronary syndomes and stroke. Med J Aust 2004; 180 (10 Suppl): S92-S96.<eMJA full text>
- 15. Initiating Better Practice. A simple effective “how-to” guide drawing on a wealth of experience to help busy professionals start a project to improve the quality of patient outcomes in the clinical setting. Available at: www.improveyourpractice.com.au/start/start.asp(accessed Apr 2004).





We would like to acknowledge the contributions of the CSSP Steering Group (see inside front cover).