Stereotypes about sex differences are rife in the popular press and in the media.1 Men are portrayed as being obsessed with sex and sports, with a beer in one hand and the television remote control in the other. Women are portrayed as being intuitive, in touch with their feelings, generally “connected”, and nurturing. These stereotypes extend to cognition, with men reported to be systemisers and women empathisers.2
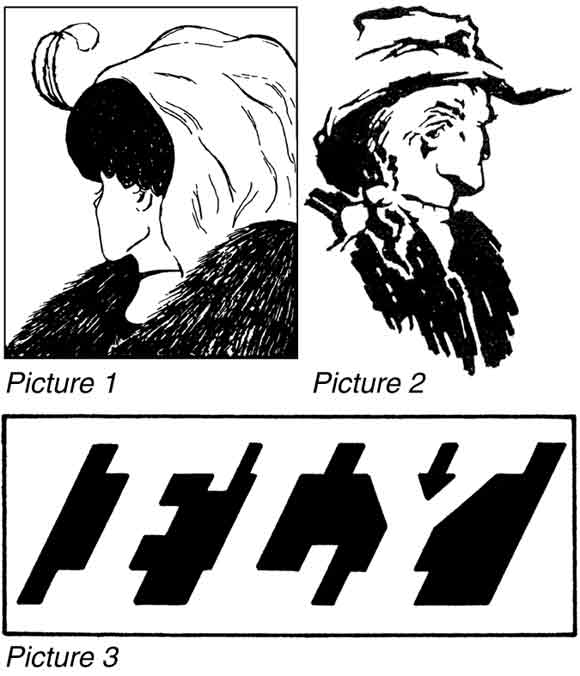
In support of their claims about sex differences, Pease and Pease make use of images that can be perceived in two ways.1 Box 1 shows a well known example of this (Picture 1). First seen on a postcard from Germany in 1888, it was published in Punch as “My Wife and Mother-in-Law” and popularised by the British cartoonist W E Hill in 1915.3 According to Pease and Pease, women are more likely to see an old woman with her chin tucked into the collar of her coat, while men are more likely to see the left-sided profile of a young woman who is looking away. These dual pictures became very fashionable in the 1930s, and many others were developed. For example, Picture 2 in Box 1 can be taken as an old cowboy with his chin tucked into his scarf, or as a young cowboy in right-sided profile, looking away.1
Further generalisations are made along right brain/left brain lines, in claiming that men are more “concrete” in the way they visualise objects, whereas women are more abstract, leading to the many jokes about men, women, maps, and directions. Pease and Pease give the example of Picture 3, claiming that men tend to see geometrical shapes, whereas women recognise the word “FLY”.
Pease and Pease suggest that differences between the sexes evolved over centuries in accordance with specific tasks. Men developed spatial ability and the ability to see objects in three dimensions because of the need to hunt and gather. Women have more peripheral vision because they had to stay in the hut to protect the children from predators.
If these differences exist, we wondered whether healthcare professionals have the same differences in brain function? Does medicine attract more polymathic, flexible types? If healthcare professionals do show the same differences, how is it likely to affect their work? If a male doctor and a female doctor are examining a patient with thyroid swelling, is the male more likely to see it in three dimensions? Should preference be given to male or female ambulance drivers? Do male and female medical students looking at the Krebs Cycle map perceive it similarly? The implications for medical practice and education are enormous.
Thus, we carried out a prospective survey on unsuspecting colleagues to investigate any potential sex-linked differences in perception. We also investigated the effects of age, seniority level, and field of specialisation.
All 90 staff members who were approached participated, giving a 100% response rate. Their average age was 35.5 years (SD, 12.1 years). Fifty-four per cent of participants (49) were men; 65 identified themselves as medical, and 15 as surgical. The two janitors who participated were included in the allied health category. Fifty-three participants were classed as senior (registrar/consultant) and the remaining 37 as junior.
Among female healthcare professionals, the first impression reported for Picture 1 was overwhelmingly of the young woman, with a significant odds ratio of 4.17 compared with men (Box 2). There was a tendency for medical personnel to see the young woman and for surgeons to see the old woman, although this did not reach significance. Seniority and age did not seem to affect initial perception.
With Picture 2, female respondents consistently saw the young cowboy compared with male respondents, who tended to see the old cowboy (Box 2). Again, affiliation, seniority and age did not seem to affect initial perception.
There was no sex-related difference in how people perceived Picture 3. However, junior doctors and medical students were significantly more likely to recognise the word than consultants or registrars (OR, 3.1; Box 3), while there was a trend for surgeons to be more likely than medical staff to do so. Overall, those who recognised the word were significantly younger (age difference of almost 7 years). Box 3 also indicates a trend for surgeons and younger, junior staff to recognise the word faster than their medical or older colleagues, although this trend did not reach statistical significance.
In examining staff members’ ability to form a second impression (ie, to see the alternate image after seeing their first image), we found that junior staff were significantly more likely to see the second image than senior staff, with an odds ratio of 2.5 (95% CI, 1.0–6.2). This appeared to be independent of age. There was also a trend for surgeons to recognise a second image better than their medical colleagues. This trend reached significance for Picture 2, with surgeons being almost 10 times more likely to see the second image than their medical colleagues (OR, 9.95; 95% CI, 1.2–80).
Our study is an initial exploration of differential perception among clinicians and allied healthcare staff. Because the sample size was small, we could only use univariate analyses, and the resulting confidence intervals are wide. Nevertheless, our study affords certain insights into sex-based perceptions, concreteness of thinking, and mental flexibility.
2: First impression of Pictures 1 and 2
|
Picture 1 (Old/young woman)* |
Picture 2 (Old/young man) |
|||||||||
Predictor |
No. |
Old (%) |
Young (%) |
OR (95% CI) |
No. |
Old (%) |
Young (%) |
OR (95% CI) |
|||
Sex |
|
|
|
|
|
|
|
||||
Male |
40 |
50 |
50 |
1 |
47 |
57 |
43 |
1 |
|||
Female |
31 |
19 |
81 |
4.17 (1.41–12.34) |
38 |
32 |
68 |
2.93 (1.19–7.16) |
|||
Affiliation |
|
|
|
|
|
|
|
||||
Medical |
48 |
35 |
65 |
1 |
60 |
52 |
48 |
1 |
|||
Surgical |
14 |
57 |
43 |
0.41 (0.12–1.38) |
15 |
33 |
67 |
2.14 (0.65–7.01) |
|||
Other |
7 |
0 |
100 |
na |
8 |
25 |
75 |
3.21 (0.60–17.18) |
|||
Level of experience |
|
|
|
|
|
|
|
||||
Consultant/Registrar |
41 |
37 |
63 |
1 |
50 |
46 |
54 |
1 |
|||
Student/Intern |
28 |
36 |
64 |
1.04 (0.38–2.82) |
32 |
44 |
56 |
1.10 (0.45–2.67) |
|||
Mean age
(years)
|
70 |
33.7 |
35.0 |
Diff |
|
36.0 |
33.2 |
Diff |
|||
OR = odds ratio; SD = standard deviation; na = not applicable. * Only 71 participants qualified for this part of the testing; the others had seen this image before. Discrepancies in totals are the result of missing data. |
|||||||||||
3: First impression and time taken to see “FLY” in Picture 3
First impression |
Time taken to see “FLY” |
||||||||||
Predictor |
No. |
“Failed” (%) |
“FLY” (%) |
OR (95% CI) |
No. |
< 3 sec (%) |
> 3 sec (%) |
OR (95% CI) |
|||
Sex |
|
|
|
|
|
|
|
||||
Male |
49 |
31 |
69 |
1 |
34 |
47 |
53 |
1 |
|||
Female |
41 |
34 |
66 |
0.85 (0.35–2.06) |
27 |
48 |
52 |
0.96 (0.35–2.63) |
|||
Affiliation |
|
|
|
|
|
|
|
||||
Medical |
65 |
34 |
66 |
1 |
43 |
42 |
58 |
1 |
|||
Surgical |
15 |
7 |
93 |
7.16 (0.88–58.07) |
14 |
71 |
29 |
0.29 (0.08–1.07) |
|||
Other |
8 |
50 |
50 |
0.51 (0.12–2.24) |
4 |
25 |
75 |
2.16 (0.21–22.49) |
|||
Level of experience |
|
|
|
|
|
|
|
||||
Consultant/ Registrar |
53 |
40 |
60 |
1 |
53 |
44 |
56 |
1 |
|||
Student/Intern |
34 |
18 |
82 |
3.06 (1.08–8.66) |
34 |
54 |
46 |
0.67 (0.24–1.87) |
|||
Mean age
(years) |
70 |
39.8 |
32.9 |
Diff
|
|
30.3 |
35.3 |
Diff |
|||
OR = odds ratio; SD = standard deviation. Discrepancies in totals are the result of missing data. |
|||||||||||
- Balakrishnan (Kichu) R Nair1
- Stephen R Mears2
- Karen I Hitchcock3
- John R Attia4
- Steven J Bowe5
- 1 John Hunter Hospital, Newcastle, NSW.
- 2 Centre for Clinical Epidemiology and Biostatistics, University of Newcastle, Newcastle, NSW.
B N is a sensitive, new-age guy who obtained permission from his young wife to do the study. J A is a Canadian who doesn’t drink beer, but is learning the rules of “the footy” after moving to Australia. S M is a librarian still searching for the word “FLY”. K H knows what you are thinking, but has not hidden the remote; she was invited to join the team to provide equity between the sexes. S B is a statistician, who has nothing to add.
- 1. Pease A, Pease B. Why men don’t listen and women can’t read maps. Sydney: Pease International Pty Ltd, 2001.
- 2. Baron-Cohen S. The essential difference: men, women and the extreme male brain. London: Allen Lane, 2003.
- 3. Perceptual ambiguity. Available at: http://psylux.psych.tu-dresden.de/i1/kaw/diverses%20Material/www.illusionworks.com/html/perceptual_ambiguity.html (accessed Nov 2003).





Abstract
Objective: To test for the presence of sex-based differences in perception (the notion that men and women “think” differently, and that differences in perception are biologically based) among healthcare professionals.
Design: Prospective survey.
Setting and participants: 90 medical personnel at a tertiary care hospital in Newcastle, NSW.
Intervention: Healthcare professionals were shown two pictures that could be interpreted as depicting either a young or an old person, and a word that could be seen as geometric shapes.
Main outcome measures: The effects of sex, age, seniority, and specialisation in relation to the first impression of the image, the ability to change one’s perception, and the speed of perception.
Results: Contrary to popular opinion, male physicians were more likely to perceive the older figures, and just as likely as women to be able to change their perception. Surgeons and junior staff were more likely to see, as well as being faster to form, an impression requiring abstract thought, and were more able to change their perceptions.
Conclusions: Traditional sex stereotypes do not apply to medical personnel, but other age-based stereotypes, and professional rivalries (medical versus surgical) may have some empiric basis.