Epithelial ovarian malignancies occur in over 1000 Australian women annually, and more than 75% of these women eventually succumb to the disease.1
Women with early-stage ovarian cancer have a 5-year survival rate of over 80%, suggesting that early detection may improve survival. To date, it has not been established whether benign (assessed histologically as non-invasive) or borderline ovarian tumours are premalignant. In the absence of a precancerous lesion, the goal of screening is the detection of preclinical disease.
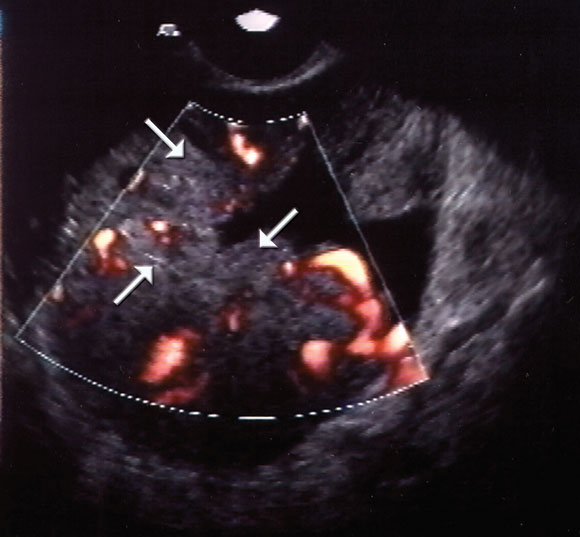
A number of screening tests have been evaluated or are being evaluated currently. These include bimanual pelvic examination, ultrasound examination (Box), with or without colour Doppler flow imaging, and measurement of various circulating proteins.
Bimanual pelvic examination as part of a "well-woman's screen" has not been found to be useful.2
Ultrasound examination alone has neither sufficient specificity nor sufficient predictive value to justify its use in community screening, and it is expensive. It is currently not known whether the addition of Doppler flow imaging substantially improves the sensitivity of ultrasound alone.3
The usefulness of measuring the level of high-molecular-weight glycoprotein CA 125 as a screening test depends on the screening strategy, the cut-off value used and the population of women studied. It is of more benefit when used as part of a multimodal strategy.
In particular, screening by measuring CA 125 level and performing transvaginal ultrasound examination appears to provide the highest specificity and positive predictive value for the detection of ovarian cancer.4
The CA 125 plus ultrasound screening strategy is currently on trial in the United Kingdom and the United States.
In the United Kingdom, CA 125 level plus transvaginal ultrasound examination versus transvaginal ultrasound alone versus no screening is being evaluated in 200 000 postmenopausal women. Quality of life, morbidity and cost-effectiveness are included in the evaluation.5 In the United States, the National Cancer Institute's Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening trial is comparing 37 000 women (aged 55–74) having annual measurement of CA 125 level and transvaginal ultrasound examination, with an equal number of women receiving their usual medical care.6 A large European multicentre trial involves 120 000 postmenopausal women randomly allocated to no screening, transvaginal ultrasound at intervals of 18 months, or transvaginal ultrasound at intervals of 3 years, for a total of 8 years.7 The results of these trials will provide evidence for whether screening provides a survival advantage, and whether this is at an acceptable financial cost. Other important issues, such as age of commencing and discontinuing screening and optimal screening intervals, will need to be established before implementing population-based screening for ovarian cancer.
Groups at high risk for ovarian cancer include:
Women with a strong family history of breast and/or ovarian cancer (two or more first-degree relatives and/or a relative with cancer before menopause) are a high-risk group8 who may carry a mutation of the BRCA1 and BRCA2 genes. These women have a risk of ovarian malignancy of up to 50%.
Women with a strong family history of colon cancer (at least three affected family members in at least two successive generations, with one case below age 50 years) may be at increased risk for endometrial and ovarian malignancy because they carry a mismatch repair gene mutation. These women have a risk of up to 10% for ovarian cancer and 50% for endometrial cancer.
Studies exploring the value of screening these women for ovarian cancer are lacking and are urgently required. Even though population-based screening for ovarian cancer is not recommended, and although there is no level of evidence that this group of women should undergo screening, it seems prudent that, until evidence to the contrary is available, measurement of CA 125 levels and transvaginal ultrasound be undertaken at least on a yearly basis. Certainly, women who may have gene mutations should be referred to family cancer clinics for counselling.
New technologies have increased the possibilities for ovarian cancer screening. The use of genomics and proteomics to identify specific proteomic patterns, gene expression and genetic alterations, using serum or urine, may revolutionise our ability to screen for this disease.9 These new developments will hopefully be of use in population screening.
- 1. Australian Institute of Health and Welfare and Australasian Association of Cancer Registries. Cancer in Australia 1998. Incidence and mortality data for 1998. Canberra: AIHW, 2001: 1-97. (AIHW Catalogue No. CAN-12).
- 2. Grover SR, Quinn MA. Is there any value in bimanual pelvic examination as a screening test? Med J Aust 1995; 162: 408-410.
- 3. Bromley B, Goodman H, Benacerraf BR. Comparison between sonographic morphology and Doppler waveform for the diagnosis of ovarian malignancy. Obstet Gynecol 1994; 83: 434-437.
- 4. Menon U, Jacobs I. Ovarian cancer screening in the general population. Ultrasound Obstet Gynecol 2000; 15: 350-353.
- 5. Menon U, Jacobs IJ. Ovarian cancer screening in the general population: current status. Int J Gynecol Cancer 2001; 11 (Suppl 1): 3-6.
- 6. Gohagan JK, Prorok PC, Hayes RB, Kramer BS. The Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening trial of the National Cancer Institute: history, organization, and status. Control Clin Trials 2000; 21 (6 Suppl): 251S-272S.
- 7. McNeil C. Ovarian cancer screening trials in progress [news]. J Natl Cancer Inst 1995; 87: 1284.
- 8. Chen WY, Garber JE, Higham S, et al. BRCA1/2 genetic testing in the community setting. J Clin Oncol 2002; 20: 4485-4492.
- 9. Mills GGB, Vast RC Jnr, Srivastava S. Future for ovarian cancer screening: novel markers from emerging technologies of transcriptional profiling and proteomics. J Int Cancer Inst 2001; 93: 1437-1439.





Abstract
Ovarian cancer is the leading cause of death from gynaecological malignancies.
No precancerous lesions have been identified.
Bimanual examination has not been proven to be of value as a screening test.
Transvaginal ultrasound examination, with or without measurement of CA 125 levels, is currently being evaluated for population screening.
Women at high risk of ovarian cancer should be screened annually — with measurement of CA 125 level and transvaginal ultrasound examination.