Clinical record
A 55-year-old woman with type 2 diabetes of 8 years' duration experienced, over 2–3 days, the onset of pain, tenderness and swelling of the medial aspect of her right thigh. She had recently commenced insulin therapy and was displaying good glycaemic control (HbA1c level of 6.4%). She had diabetic complications of autonomic and peripheral neuropathy, but no retinopathy. Other medical problems included chronic renal impairment, hypertension, polyarticular gout and hydralazine-induced lupus. A renal biopsy had not been performed, but her renal insufficiency was believed to be a result of diabetic nephropathy and hypertension. She was taking twice-daily mixed insulin (16 units in the morning and 10 units at night), felodipine (10 mg/day), paroxetine (10 mg/day), allopurinol (75 mg/day) and prednisolone (7.5 mg/day). Her serum creatinine level had peaked at 0.31 mmol/L, but stabilised at 0.21 mmol/L after cessation of an angiotensin-converting enzyme inhibitor. A 24-hour urine collection showed a creatinine clearance rate of 0.12 mL/s (normal range [NR], 1.5–2.5 mL/s) and a protein excretion rate of 4.6 g/day. Renal duplex ultrasound showed that her kidney size was well preserved, but there was a suggestion of renal artery stenosis on the right side. There was no history of recent injury or injection to her thigh. She had not experienced any rigors and was afebrile. The area of the localised, tender swelling on the medial aspect of her right thigh was not erythematous and no local lymphadenopathy was noted. Apart from the thigh swelling, there was generalised wasting and weakness of the lower limbs, loss of ankle reflexes, and loss of sensation in a stocking distribution, consistent with a diagnosis of peripheral neuropathy. Examination of her left foot revealed two small gangrenous areas. Foot pulses were present and the gangrenous areas were thought to be caused by inappropriate footwear. 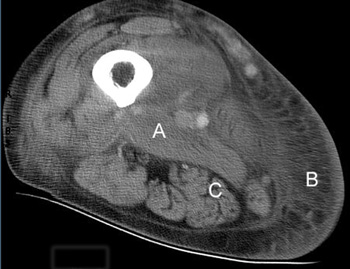 Figure 1: Computed tomography image of the thigh, showing marked oedema and thickening of the adductor muscle group (A), extensive subcutaneous oedema (B), and sparing of the hamstring muscle (C). |
Investigations showed an elevated white cell count of 16 x 109/L (NR, 4.0–11.0 x 109/L), a platelet count of 432 x 109/L (NR, 150–400 x 109/L), an erythrocyte sedimentation rate of 110 mm/h (NR, 7–18 mm/h) and a C-reactive protein level of 119.3 mg/L (NR, 1.6–8.7 mg/L). Creatine kinase (174 U/L; NR, < 215 U/L) and lactate (0.6 mmol/L; NR, 0.5–2.0 mmol/L) levels were normal. Separate to the swelling on the medial aspect of the thigh, a presumed thrombus was palpable in the lateral accessory long saphenous vein. A subsequent ultrasound detected this thrombus extending from the mid thigh to the lateral aspect of the knee, but no deep venous thrombosis was found. She was treated with cephalexin and aspirin. Over the next two weeks, the thigh swelling evolved into a tender, palpable mass measuring 6 x 20 cm. A computed tomography (CT) scan revealed marked swelling of the entire adductor muscle group, but no discrete mass (Figure 1). In the absence of a clear diagnosis, an exploratory operation of her right thigh was performed. This showed no haemorrhage or abscess, but evidence of extensive oedema and necrosis of the adductor muscles. Samples taken for microbiological analysis were sterile. Histological examination of a biopsy specimen showed necrotic muscle, an inflammatory cell infiltrate, fibrosis and evidence of muscle fibre regeneration. The occasional small blood vessel containing fibrin thrombus was also seen, but no features of vasculitis were identified (Figures 2 and 3). A diagnosis of diabetic muscle infarction was made. 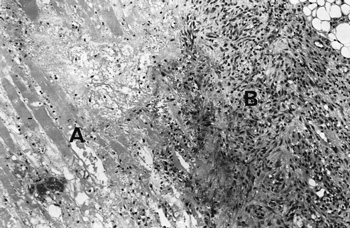 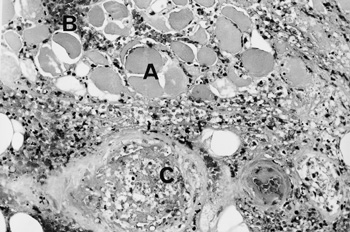 Photomicrographs (original magnification x 250) of a biopsy specimen of the adductor group of muscles. Figure 2: Longitudinal section, showing necrotic muscle fibres (A) and granulomatous tissue (B). Figure 3: Cross-section showing necrotic muscle (A), an inflammatory cell infiltrate (B) and a blood vessel containing a thrombus (C). No evidence of vasculitis was seen. |
The diagnosis of diabetic muscle infarction was made retrospectively on clinical grounds and after reviewing the subsequent investigations. The differential diagnoses — muscle strain, rupture, haematoma, myositis, infection, deep venous thrombosis, thrombophlebitis, femoral artery aneurysm, fracture or a connective tissue tumour — were excluded by the clinical presentation, together with the ultrasound, computed tomography (CT) scan and biopsy findings.
The CT scan did not reveal a discrete mass, but extensive oedema of one muscle group and sparing of an adjacent muscle group. Histologically, there was evidence of skeletal muscle fibre necrosis, with a variable amount of muscle regeneration and fibrosis. These are the typical features of diabetic muscle infarction.1 Reports of spontaneous muscle infarction appear to be virtually confined to patients with diabetes.
Spontaneous muscle infarction is a rare diabetic complication. There have been fewer than 100 patients reported since 1965.1-12 However, it is becoming more frequently recognised; almost half of the cases have been reported since 1999.3-12 It has a predilection for the quadriceps (62%), hip adductors (13%), hamstrings (8%) and hip flexor (2%) muscles. Rarely, the calf and anterior tibial muscles are involved. The pathogenesis of diabetic muscle infarction is still unclear, but a diffuse microangiopathic process, possibly associated with hypoxia–reperfusion injury, has been implicated as a cause.1,10,12
Magnetic resonance imaging (MRI) is the preferred diagnostic test, revealing swollen and oedematous muscles (ie, increased signal intensity of T2-weighted images).4,7 Abnormal MRI findings have been reported in all patients with diabetic muscle infarction. Although, in retrospect, our patient's CT findings were consistent with muscle infarction, a CT scan is considered a less sensitive test, as only 83% of patients with muscle infarction have abnormal CT findings.1 An MRI scan was not performed in our patient, as diabetic muscle infarction was not initially considered in the differential diagnosis. Consensus opinion suggests that muscle biopsy is not necessary in a patient presenting with the typical clinical features of diabetic muscle infarction — without fever, erythema, or elevated white cell count — if the MRI findings are appropriate.1
Management consists of the avoidance of weightbearing, and simple analgesia. After resolution of the acute phase, physical therapy and rehabilitation are useful. As with our patient, total recovery over 4–6 weeks can be expected. In about 50% of patients recurrences occur, but not necessarily in the same muscle group.
- 1. Grigoriadis E, Fam AG, Starok M, et al. Skeletal muscle infarction in diabetes mellitus. J Rheumatol 2000; 27: 1063-1068.
- 2. Angervall L, Sterner B. Tumiform focal muscular degeneration in two diabetic patients. Diabetologia 1965; 1: 39-42.
- 3. Smith AL, Laing PW. Spontaneous tibial compartment syndrome in type 1 diabetes mellitus. Diabet Med 1999; 16: 168-169.
- 4. Aboulafia AJ, Monson DK, Kennon RE. Clinical and radiological aspects of idiopathic diabetic muscle infarction. J Bone Joint Surg Br 1999; 81: 323-326.
- 5. Lafforgue P, Janand-Delenne B, Lassman-Vague V, et al. Painful swelling of the thigh in a diabetic patient: diabetic muscle infarction. Diabetes Metab 1999; 25: 255-260.
- 6. Willenberg HS, Hauner H, Scherbaum WA. A man with diabetes and a swollen leg. Lancet 1999; 353: 1527-1528.
- 7. Jelinek J, Murphey MD, Aboulafia AJ, et al. Muscle infarction in patients with diabetes mellitus: MR imaging findings. Radiology 1999; 211: 241-247.
- 8. Madhan KK, Symmans P, Te Strake LT, et al. Diabetic muscle infarction in patients on dialysis. Am J Kidney Dis 2000; 35: 1212-1216.
- 9. Spengos K, Wohrle JC, Binder J, et al. Bilateral diabetic infarction of the anterior tibial muscle. Diabetes Care 2000; 23: 699-701.
- 10. Silberstein L, Britton KE, Marsh FP, et al. An unexpected cause of muscle pain in diabetes. Ann Rheum Dis 2001; 60: 310-312.
- 11. Pedicelli A, Belli P, Fractino M, et al. Diabetic muscle infarction. Am J Med 2001; 111: 671-672.
- 12. Toh V, Winocour P. Bilateral lower limb pain and swelling in a young girl with type 1 diabetes mellitus. Hosp Med 2001; 62: 783-785.





Acknowledgement: Dr R Hope and Mr J Royle participated in the management of this patient and assisted in preparing the clinical record. We would like to thank Dr R Kalnins and Dr M Richardson, who assisted in obtaining the photomicrograph and computed tomography images.