Twenty-two per cent of Australia's population, 20% of our general practitioners (GPs), but only 7% of our surgeons, are located outside metropolitan and large rural centres.1 To access specialist services, people from rural and remote areas usually travel to major centres, or, on a third of all occasions, to capital cities,1 which often involves considerable expense, time off work and dislocation from their usual support networks.2
Evidence from the United Kingdom, Europe and Canada suggests that the distance to specialists and the rurality of general practice influence GPs' referral decisions.3-7 Large samples are needed, however, to account for the wide variations in referral rates observed among individual practitioners.8 No detailed analysis of referrals by Australian GPs has previously been undertaken, despite there being substantial geographic barriers to specialist care in rural areas, as well as Medicare data showing decreasing use of specialist services with increasing distance from capital cities.1
Our study examined the effect that proximity of a surgical specialist has on Australian GPs' referral rates of surgical problems to specialist care. Thus, it is in effect determining whether GPs in rural or remote areas are as likely as those in urban areas to refer surgical problems.
Data from the Bettering the Evaluation and Care of Health (BEACH) program (Box 1) covering the period April 1998 to March 2001 were analysed.
The outcome of interest was a new referral to a procedural specialist (hereafter referred to as a "specialist"). We included the broad range of specialties in which surgical procedures form a large part of practice, as well as referrals for endoscopy and to clinics usually attended by surgeons or obstetricians, such as breast, antenatal and in-vitro fertilisation clinics. Referrals to specialists' rooms, to hospital outpatients and to emergency departments contributed to the total number of referrals. No distinction was made between the type or location of specialists to whom patients were referred, as there is variation in the breadth of practice between individual clinicians,13 and uncertainty about specialists' exact qualifications.
We limited our study to patients' problems in the domain of the surgical specialties (hereafter referred to as "problems" — "problems" were used rather than "patients", as patients may have had more than one surgical problem). "Problems" were defined for the purpose of our analysis as (i) all problems referred to surgical specialists at least once in every 10 presentations, or (ii) those referred in fewer than 10% of presentations, but which were considered by a panel of specialists at Royal Darwin Hospital to be "a usual part of their practices". Each problem was allocated to the most relevant of the following specialty groups, which were chosen to minimise potential overlap: general/vascular/plastic surgery, orthopaedic surgery, otolaryngology (ENT), obstetrics and gynaecology, ophthalmology, urology, and other.
We tested the difference in referral rates of GPs with and without a local specialist, without considering the actual distance between the GP and the nearest specialist. GPs were defined as having a "local specialist" if a specialist's principal practice address was located within the same population centre. Population centres were defined using the boundaries in the Rural, Remote and Metropolitan Areas (RRMA) classification system, which surround the perimeter of capital cities, regional centres and smaller population centres.14
We determined principal practice addresses for all surgical specialties using current lists of Fellows' practice locations obtained from the Royal Australasian College of Surgeons (which included ophthalmologists) and the Royal Australian and New Zealand College of Obstetricians and Gynaecologists. If there was any uncertainty, local hospitals were contacted by telephone. We acknowledged the fact that many rural general surgeons have considerable experience in managing orthopaedic, ENT, urological, ophthalmological, and obstetric and gynaecological problems when specialists in these disciplines are not available locally.13 We therefore used the presence of a general surgeon or the relevant subspecialist as the criteria for a "local specialist".
The "survey estimator" commands in Stata 7.0 were used to account for the design effect of the cluster sample.15,16 Calculations of all reported P values and 95% CIs were based on the standard error, adjusted using the robust variance estimator method.
Characteristics of the GPs, patients and problems, grouped according to the presence or absence of local surgical specialists, were compared using two-way tables and 95% CIs. Problems were used as the unit of analysis for modelling the predictors of specialist referrals. Two-way tables were then used to compare the unadjusted differences, according to the availability of a local specialist, in the proportion of problems referred in each specialty.
The independent predictors of referral were determined using multiple logistic regression. Because the relationship between the unadjusted proportion of problems referred and specialist proximity differed between specialties, interaction terms were created to test for effect modification of specialist proximity on the proportion referred to each specialty, as well as the proportion referred in cancer-related and injury-related problems. A hierarchical model with all main effects and interaction terms of interest was fitted. Backward elimination of the terms and effects was based on the Wald statistic, adjusted for the cluster sample. Significant interaction terms were retained (α = 0.01), along with their main effects, and other factors were further reduced (α = 0.05). For significant interactions, proximity contrasts were performed by refitting the model using each specialty in turn as the reference group. The main effect of proximity then gave the simple effect of absence of a local specialist on the likelihood of referral of problems in each specialty, after controlling for other factors. The strength of fit of the model was examined using the area under the receiver operating characteristics (ROC) curve.
In any specialty in which proximity of a specialist was found to be significantly associated with referral, major diagnostic subcategories (decided in advance) were examined to see where these differences might lie.
A total of 449 277 problems among 303 000 patient encounters were recorded in the BEACH program between April 1998 and March 2001. Thirty-two per cent (141 531) were classified as surgical problems. These were identified in 125 293 patient encounters and 13 518 (9.5%) were referred to a specialist.
Fourteen per cent (434/3030) of GPs recruited in the BEACH program practised in locations where there were no local specialists (Box 2). GPs with a local specialist referred 11 443 (9.6%) surgical problems; those without a local specialist referred 2075 (9.2%) problems. Overall, no significant difference existed between GPs with and without a local specialist in the number of problems managed per encounter or the proportion of problems referred (Box 2).
In areas where there were no local specialists, GPs were more often men, in full-time practice and had fewer practice partners. Their encounters were more often with patients who held a Health Care Card or identified as Aboriginal or Torres Strait Islanders, and were less often with patients from a non-English-speaking background. There were also some differences in the casemix of the surgical problems in areas with and without a surgical specialist (Box 2).
The proportion of problems referred in each specialty, where local specialists were and were not available, is shown in Box 3. GPs without a local specialist referred a lower proportion of obstetric and ophthalmological problems. There were no significant differences in the proportion of problems referred in the other specialties.
The full logistic regression model therefore included interaction terms with their main effects, and GP, patient and problem characteristics as listed in Box 2. The factors with main effects significantly associated with referral in the final model are shown in Box 4, and contrasts for significant interaction terms are shown in Box 5. There was no association between referral and GP's age, part-time status and number of practice partners, nor with patients from Aboriginal and Torres Strait Islander or non-English-speaking backgrounds. The area under the ROC curve for the final model was 0.667.
While the univariate analysis found that absence of a local specialist had no significant effect on the proportion of problems referred (Wald statistic F1,3028 = 0.14; P = 0.71), adjustment for other significant factors revealed a significant effect modification of specialist proximity on referral in individual specialties (Wald statistic F7,3022 = 8.89; P < 0.001). Highly significant differences were found when each specialty was examined individually (Box 5). GPs without a local specialist were 44% less likely to refer obstetric problems, 40% less likely to refer ophthalmological problems, but 18% more likely to refer orthopaedic problems.
In further analysis (data not shown) antenatal problems, but not problems related to delivery or postnatal care, were much less likely to be referred if there was no local specialist. Patients with a painful/red eye, visual loss, cataract, glaucoma, ophthalmic trauma, refractive error, diabetes and other systemic ocular conditions were less likely to be referred in the absence of a local specialist, differences not seen in those with muscle imbalance/squint or lid and conjunctival disorders. The presence or absence of a local specialist had little influence on the proportion of all ophthalmological problems referred to optometrists (2.3% v 2.4%).
This analysis shows that the presence or absence of a local specialist does not significantly affect the proportion of general surgical (including vascular and plastic surgery), orthopaedic, ENT, urological or gynaecological problems referred by GPs. Antenatal and eye problems, however, are over 40% less likely to be referred by GPs without a local specialist, an effect greater than the other influences on referral which were included in the model.
While highly significant, our model was only a moderate predictor of referrals, and suggests there are influences other than those we have considered. Qualitative studies have shown that the decision to refer is complex, being related not only to clinical factors and specialist availability, but also to characteristics of the referring doctor (eg, willingness to tolerate uncertainty, legal risks and concern about how the consultant will evaluate the referral), the patient (eg, their expectations, circumstances and assertiveness), and the relationships the GP has both with the patient and the specialist.17-19
Some of the factors we identified as lowering referral rates to surgical specialists, such as the sex of the GP (male GPs refer a lower proportion of problems) and the age of the patient (fewer younger patients are referred), are consistent with international studies.5 In addition, when we controlled for pattern of morbidity, we found that low socioeconomic status (indicated by a Health Care Card) was associated with a lower likelihood of referral.
Because of shortages of surgical specialists in rural and remote areas of Australia, our study, in effect, compares referral patterns in rural and urban areas. Rural GPs are more likely than their urban colleagues to provide routine antenatal care, and many have had extra training to do so. This is consistent with our observations that obstetric problems formed a greater part of rural general practice, but a smaller proportion of referrals.
However, unlike antenatal care, the contribution and casemix of ophthalmological problems, as a proportion of all surgical problems, was similar regardless of proximity to a specialist. This suggests that the lower proportion of eye problems referred cannot be explained by a greater number of GP consultations per episode of illness, nor is it likely to be owing to chance given that it is highly statistically significant. The true difference may be even greater than the observed difference, however, because we included general surgeons as the minimum criteria for a "local specialist".
The difference may reflect differences in GPs' real or perceived ability to manage eye problems. Rural GPs may be more willing to intervene, or they may be more accustomed to obtaining specialist advice over the telephone, and therefore refer less often than urban GPs.
Relating quality of care to high or low referral rates is difficult though,20 and GPs with specific expertise may actually refer more patients because of their better assessment of patients' needs or greater awareness of investigative and treatment options.21,22 Nonetheless, it is important to identify under-referral, which could deprive some patients of treatment from which they could benefit, and over-referral, which may expose patients to unnecessary risks associated with treatment and lead to excessive consumption of resources.20,23 Comparison of primary care and specialist management of ophthalmological disorders in urban and rural settings would help to identify the settings, patients, problems and severity for which specialist referral is of greatest benefit. Services could then be more accurately tailored to maximise access and minimise the problems of under- and over-referral.
The finding that there were similar referral rates to general/vascular/plastic surgery, orthopaedic, ENT, urological and gynaecological specialists in areas with and without local specialists is remarkable given that some of these problems require only minor procedures within the capabilities of many rural and remote GPs. Three factors may have concealed a real difference:
Through random sampling the BEACH program reflects the geographic distribution of all GPs and therefore includes only small numbers of very remote GPs, whose patients face the greatest geographic barriers.
Specialists without Australian fellowship status, who are more likely to be practising in rural areas, were not included in our study; and
The BEACH program does not record measures of problem severity, and it is possible that some problems are more severe or present later in remote areas. This may also explain why a slightly higher proportion of orthopaedic problems were referred.
Finally, it is important to appreciate that not all patients referred by GPs consult a specialist. Many rural patients need to travel long distances to access a specialist or wait for visiting specialist services. When access barriers are too great, patients may not complete their referrals.24
Our study has identified systematic influences on referral decisions, and supports further examination of the need for and supply of ophthalmological services in particular. Overall, absence of a surgical specialist locally does not diminish demand by GPs for specialist care for their patients. This is an important consideration for policy relating to the rural specialist workforce, outreach services, telemedicine, and maintenance of broad skills in rural and remote general practice.
1: The BEACH program
The Bettering the Evaluation and Care of Health (BEACH) program <http://www.fmrc.org.au/beach.htm> has been undertaken to describe general practice activity in Australia.9 Its design and scale minimise the potential problems of inappropriate numerators, denominators and sample size that often befall studies comparing referral rates.10
Each year about 1000 general practitioners are randomly selected from all active GPs in Australia. Each GP involved in the study prospectively records information about 100 consecutive encounters with patients, including free-text entry of the problems managed and referrals made. Data are subsequently classified by trained personnel according to the International classification of primary care (ICPC-2)11 and coded with ICPC-2 Plus, an extended vocabulary of terms which covers the range of diagnoses and symptoms commonly seen in general practice, and the commonly undertaken tasks.12
2: Characteristics of general practitioners, patient encounters and surgical problems, by proximity of surgical specialist
Local specialist |
No local specialist |
||||||||||
Characteristics of GPs and practice |
|||||||||||
Number of GPs |
2596 |
434 |
|||||||||
Mean age (95% CI) (years) |
48.7 (48.3–49.1)* |
48.0 (47.0–48.9)* |
|||||||||
Proportion of GPs (95% CI) |
|||||||||||
Male sex |
68.1% (66.3%–69.9%)* |
76.7% (72.5%–80.5%)* |
|||||||||
Full-time practice |
68.9% (67.1%–70.6%)* |
77.7% (73.5%–81.3%)* |
|||||||||
Practice size: |
|||||||||||
Solo |
18.2% (16.8%–19.8%) |
19.8% (16.2%–23.9%) |
|||||||||
2–4 GPs |
38.1% (36.2%–40.0%)† |
46.4% (41.6%–51.2%)† |
|||||||||
5–9 GPs |
36.5% (34.7%–38.4%) |
30.9% (26.7%–35.5%) |
|||||||||
10+ GPs |
7.2% (6.2%–8.3%)† |
2.9% (1.7%–5.0%)† |
|||||||||
Characteristics of patient encounters |
|||||||||||
Number of encounters |
105 530 |
19 763 |
|||||||||
Mean age of patients (95% CI) (years) |
47.4 (47.0–47.8)* |
48.8 (48.0–49.7)* |
|||||||||
Proportion of encounters (95% CI) |
|||||||||||
Male sex |
41.1% (40.5%–41.7%)† |
43.4% (42.0%–44.7%)† |
|||||||||
Health Care Card holder |
37.9% (37.1%–38.8%)* |
43.9% (42.1%–45.7%)* |
|||||||||
Aboriginal/Torres Strait Islander |
0.7% (0.5%–0.8%)* |
2.3% (1.6%–3.3%)* |
|||||||||
Non-English-speaking background |
9.7% (9.0%–10.4%)* |
1.7% (1.3%–2.3%)* |
|||||||||
Multiple problems managed at encounter |
46.5% (45.8%–47.3%) |
46.1% (44.4%–47.7%) |
|||||||||
Characteristics of surgical problems |
|||||||||||
Number of problems |
118 973 |
22 558 |
|||||||||
Proportion of problems (95% CI) |
|||||||||||
New problem |
36.4% (35.7%–37.1%)† |
34.0% (32.5%–35.5%)† |
|||||||||
Specialty group of problem: |
|||||||||||
General/vascular/plastic surgery |
38.6% (38.1%–39.0%)† |
40.1% (39.2%–41.1%)† |
|||||||||
Orthopaedics |
31.3% (30.7%–31.9%)* |
29.1% (28.2%–30.0%)* |
|||||||||
Ear, nose and throat |
9.4% (9.1%–9.6%)† |
8.4% (7.9%–8.9%)† |
|||||||||
Obstetrics and gynaecology |
7.8% (7.5%–8.2%)† |
9.3% (8.4%–10.3%)† |
|||||||||
Ophthalmology |
3.7% (3.5%–3.8%) |
3.5% (3.2%–3.8%) |
|||||||||
Urology |
4.5% (4.3%–4.7%) |
4.9% (4.5%–5.2%) |
|||||||||
Other |
4.8% (4.7%–5.0%) |
4.7% (4.4%–5.0%) |
|||||||||
Injury-related problem |
12.0% (11.7%–12.3%) |
11.4% (10.7%–12.2%) |
|||||||||
Cancer-related problem |
3.6% (3.5%–3.8%)* |
5.4% (5.0%–5.8%)* |
|||||||||
* P < 0.001; † P < 0.01. |
|||||||||||
3: Proportion (and 95% CIs) of problems referred in each specialty, by availability of specialist
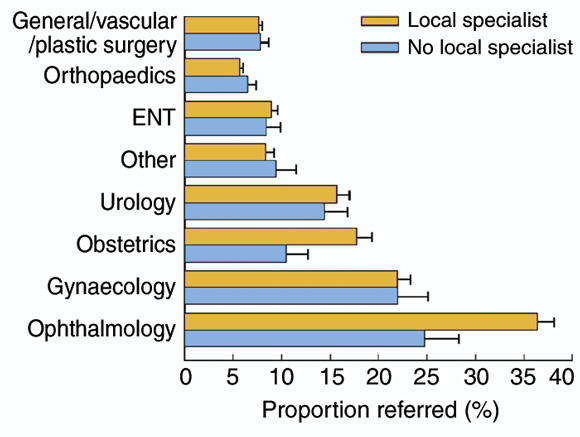
GPs without a local specialist referred a lower proportion of obstetric and ophthalmological problems.
4: Main effects in the final model: significant independent main effect predictors of referral to a specialist*
Main effect predictors |
Adjusted odds ratio (95% CI) of referral to a specialist |
||||||||||
Patient age group (reference, 65 years and over)† |
|||||||||||
Less than 15 years |
0.60 (0.55–0.66) |
||||||||||
15–24 years |
0.79 (0.73–0.86) |
||||||||||
25–44 years |
0.95 (0.89–1.01) |
||||||||||
45–64 years |
1.08 (1.02–1.14) |
||||||||||
Injury-related problem |
0.82 (0.77–0.89) |
||||||||||
Each extra problem at encounter |
0.84 (0.82–0.87) |
||||||||||
Male patient |
1.08 (1.04–1.13) |
||||||||||
Not a Health Care Card holder |
1.13 (1.08–1.18) |
||||||||||
New problem |
1.15 (1.10–1.21) |
||||||||||
Female GP |
1.18 (1.11–1.24) |
||||||||||
Cancer-related problem |
1.29 (1.17–1.42) |
||||||||||
* The interaction between problem specialty and proximity of specialist was significant (adjusted Wald statistic, F7,3022 = 8.89; P < 0.001); details are shown in Box 5. † Adjusted Wald statistic F4,3025 = 47.44; P < 0.001. |
|||||||||||
5: Interaction contrasts in the final model: effect of absence of a local specialist on the likelihood of referral by GPs in each surgical specialty
Surgical specialty |
Adjusted odds ratio (95% CI) of referral |
||||||||||
Obstetrics |
0.56 (0.44–0.70) |
||||||||||
Ophthalmology |
0.60 (0.49–0.73) |
||||||||||
Urology |
0.92 (0.76–1.12) |
||||||||||
Ear, nose, throat |
0.96 (0.80–1.14) |
||||||||||
Gynaecology |
1.02 (0.83–1.24) |
||||||||||
General/vascular/ plastic surgery |
1.03 (0.93–1.15) |
||||||||||
Other |
1.11 (0.88–1.40) |
||||||||||
Orthopaedics |
1.18 (1.03–1.34) |
||||||||||
- Russell L Gruen1
- Ross S Bailie2
- Stephanie Knox3
- Helena Britt4
- 1 Flinders University Northern Territory Clinical School, and Menzies School of Health Research, Casuarina, NT.
- 2 Australian Institute of Health and Welfare General Practice Statistics and Classification Unit, and Family Medicine Research Centre, University of Sydney, Westmead Hospital, Westmead, NSW.
We wish to thank the 3030 GPs who participated in this period of the BEACH program, which is conducted by the General Practice and Statistics Unit, a collaborating unit of the Australian Institute of Health and Welfare and the University of Sydney. Over the 1998–2001 period the program has been funded by the Commonwealth Department of Health and Aged Care, the Commonwealth Department of Veterans' Affairs (1998–99), the National Occupational Health and Safety Commission (1998–99), Astra Zeneca (Aust.), Aventis-Pharma Pty Ltd, Roche Products Pty Ltd, and Janssen-Cilag Pty Ltd (2001).
Dr Gruen is supported by a National Health and Medical Research Council Medical Postgraduate Scholarship, and a Surgeon Scientist Award from the Royal Australasian College of Surgeons Foundation.
None identified.
- 1. Australian Institute of Health and Welfare (AIHW). Health in rural and remote Australia. AIHW Cat. No. PHE 6. Canberra: AIHW, 1998.
- 2. Rankin SL, Hughes-Anderson W, House AK, et al. Costs of accessing surgical specialists by rural and remote residents. Aust N Z J Surg 2001; 71: 544-547.
- 3. Roland M, Morris R. Are referrals by general practitioners influenced by the availability of consultants? BMJ 1988; 297: 599-600.
- 4. Noone A, Goldacre M, Coulter A, Seagroatt V. Do referral rates vary widely between practices and does supply of services affect demand? A study in Milton Keynes and the Oxford region. J R Coll Gen Pract 1989; 39: 404-407.
- 5. Garcia-Olmos L, Abraira V, Gervas J, et al. Variability in GPs' referral rates in Spain. Fam Pract 1995; 12: 159-162.
- 6. Langley GR, Minkin S, Till JE. Regional variation in nonmedical factors affecting family physicians' decisions about referral for consultation. CMAJ 1997; 157: 265-272.
- 7. Aaraas I, Fylkesnes K, Forde OH. GPs' motives for referrals to general hospitals: does access to GP hospital beds make any difference? Fam Pract 1998; 15: 252-258.
- 8. Moore AT, Roland MO. How much variation in referral rates among general practitioners is due to chance? BMJ 1989; 298: 500-502.
- 9. Britt H, Miller GC, Charles J, et al. General practice activity in Australia 1999-2000. GEP 5. Canberra: Australian Institute of Health and Welfare, 2000.
- 10. Roland M. General practitioner referral rates. BMJ 1988; 297: 437-438.
- 11. Classification Committee of the World Organisation of Family Doctors (WONCA). ICPC-2: International Classification of Primary Care. 2nd edition. Oxford: Oxford University Press, 1998.
- 12. Britt H. A new coding tool for computerised clinical systems in primary care — ICPC plus. Aust Fam Physician 1997; 26(Suppl 2): S79-S82.
- 13. Tulloh B, Clifforth S, Miller I. Caseload in rural general surgical practice and implications for training. Aust N Z J Surg 2001; 71: 215-217.
- 14. Department of Primary Industries and Energy and Department of Human Services and Health. Rural, remote and metropolitan areas classification. 1991 census edition. Canberra: AGPS, 1994.
- 15. Levy PS, Lemeshow S. Sampling of populations: methods and applications. 3rd edition. New York: Wiley, 1999.
- 16. Stata [computer program], release 7.0. College Station, Tex: Stata Corporation, 2001.
- 17. Dowie R. General practitioners and consultants — a study of outpatient referrals. London: King Edward's Hospital Fund for London, 1983.
- 18. Newton J, Hayes V, Hutchinson A. Factors influencing general practitioners' referral decisions. Fam Pract 1991; 8: 308-313.
- 19. Langley GR, MacLellan AM, Sutherland HJ, Till JE. Effect of nonmedical factors on family physicians' decisions about referral for consultation. CMAJ 1992; 147: 659-666.
- 20. Roland MO, Bartholomew J, Morrell DC, McDermott A, Paul E. Understanding hospital referral rates: a user's guide. BMJ 1990; 301: 98-102.
- 21. Reynolds GA, Chitnis JG, Roland MO. General practitioner outpatient referrals: do good doctors refer more patients to hospital? BMJ 1991; 302: 1250-1252.
- 22. Calman NS, Hyman RB, Licht W. Variability in the decision to consult and its relationship to diagnostic uncertainty. J Fam Pract 1992; 35: 31-38.
- 23. Nutting PA, Franks P, Clancy CM. Referral and consultation in primary care: do we understand what we're doing? J Fam Pract 1992; 35: 21-23.
- 24. Gruen RL, Bailie RS, d'Abbs PH, et al. Improving access to specialist care for remote Aboriginal communities: evaluation of a specialist outreach service. Med J Aust 2001; 174: 507-511.





Abstract
Objective: To determine the effect of proximity of surgical specialists on general practitioners' (GPs') rates of referral of surgical problems to specialist care (ie, are surgical referral rates of GPs in rural or remote areas similar to those of GPs in urban centres?).
Design: A cross-sectional survey of GP–patient encounters.
Setting: The Bettering the Evaluation and Care of Health (BEACH) program, which involves all active registered GPs in Australia.
Participants: A random sample of 3030 GPs, each providing details of 100 consecutive patient encounters.
Main outcome measures: Proportion of surgical problems (including ophthalmological and obstetric and gynaecological) referred to surgical specialists (surgeons' rooms, hospital outpatient departments or hospital emergency departments).
Results: Absence of a local specialist did not significantly influence the proportion of surgical problems referred by GPs overall, but the proportion referred was significantly lower for obstetric (odds ratio [OR], 0.56; 95% CI, 0.44–0.70) and ophthalmological (OR, 0.60; 95% CI, 0.49–0.73) problems. Other factors independently associated with referral of a lower proportion of problems included male GPs, female and younger patients, holders of a Health Care Card, injury-related and non-cancer-related problems, follow-up presentations, and more than one problem managed at an encounter.
Conclusions: Our findings confirm that rural and remote GPs undertake much of their patients' antenatal care, and are less likely to use specialists when managing ophthalmological problems. Absence of local specialists in other surgical specialties is not a barrier to referral of patients with surgical disorders.